CHAPTER 24 Coronal browlift
Physical evaluation
• Attain a thorough ocular and eyelid history, past medical history, past facial surgical history, craniotomy scars, and forehead trauma.
• Check the visual acuity of each eye.
• Examine the brow position relative to the anterior hairline as well as superior orbital rim.
• Brow ptosis and upper lid skin.
• Skin quality and rhytid depth in the medial and lateral forehead.
• Document the motor and sensory function to the forehead.
Anatomy
Understanding the temporal and forehead anatomy is critical to successful browlift surgery (Fig. 24.1). The scalp is composed of five layers (Skin, Connective tissue, galea Aponeurotica, Loose areolar connective tissue, and Periosteum). The blood supply to the forehead scalp is from the internal (supratrochlear, supraorbital) and external carotid (superficial temporal) arteries. Hair follicles are located in the subcutaneous layer. Injury to the follicles results in temporary or permanent alopecia. The frontal branch of the facial nerve is located in the superficial temporal fascia and innervates the muscles of the forehead (frontalis, corrugators, depressor supercilii, and procerus). The supratrochlear and supraorbital nerves provides sensation to the central and lateral forehead as well as portions of the anterior scalp.
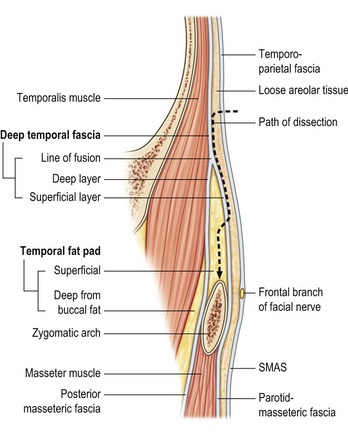
Fig. 24.1 Temporal region.
From Stuzin, JM et al. Anatomy of the frontal branch of the facial nerve: the significance of the temporal fat pad. Plast Reconstr Surg 1989;83:265–271.
No single “ideal” brow position is applicable for all patients. It has been suggested that the ideal brow appearance in women and men are different. In women, the medial brow should be slightly above the supraorbital ridge with the apex of the arch lateral to the mid pupil (Westmore 1974). Men typically should have brows that lie at the level of the supraorbital rim and are less arched. Ethnic variations in desired brow position and shape also must be considered when planning surgery for brow ptosis.
Technical steps
Complications
Complications after open browlift are similar to other aesthetic procedures. Early diagnosis helps to prevent further bruising. Described complications include alopecia, scar widening, sensory nerve deficit, frontal muscle paralysis, skin necrosis, scar pruritis, infection, hematoma and bleeding, asymmetrical eyebrows or eyelids, chronic pain, over correction, and abnormal soft-tissue contour. Minimal tension along properly planned intraoperative incisions helps to reduce scalp alopecia or scar widening. Hair bearing scalp incisions should be placed parallel to direction of hair follicles. Hemostasis with bipolar forceps is used when possible. Galeal reapproximation is important to release hair bearing scalp tension. Management of complications focuses on the etiology of the setback. Revisional surgery is recommended only after a minimum of six months has elapsed. Widened scars or alopecia may benefit from hair transplantation or surgical scar re-excision. Browlift reversal has been described by Yaremchuk (2007). Frontalis muscle paralysis is rare. Injury to the frontal branch of the facial nerve can occur if flap dissection at the lateral orbital rim is too superficial. In the lateral orbital area the frontal branches of the facial nerve on the deep surface of the frontalis muscle can be visualize on the deep surface of the frontalis muscle. If frontalis paralysis is noted, it is almost always temporary. Full return of function may take up to 12 months. Chronic pain may require neurology service evaluation for medical therapy or surgical neurolysis. Brow asymmetry may be corrected temporarily with judicious use of botulinum toxin.
Pearls & pitfalls
Pearls
• Proper thorough preoperative evaluation, patient selection, and surgical planning are critical for successful outcome and decreases risk for surgical misadventure. Patients must fully understand the goal of surgery.
• Excessive browlifts can result in the unfavorable appearance of a surprised look.
• When performing browlift with blepharoplasty, we recommend performing the blepharoplasty first. Dry eye symptoms can also result if excessive upper lid blepharoplasty skin excision is performed concomitantly.
• It is important to dissect in the subperiosteal plane to the superior orbital rim to release orbital retaining ligaments (Mendelson 2002). Inadequate release of these attachment points can result in early relapse.
• The anterior scalp flap should be fixed to the posterior scalp periosteum laterally using a permanent suture to prevent relapse.
• Corrugator, procerus, and depressor supercilü muscle can be divided carefully to provide forehead attachment release. Preservation of supratrochlear and supraorbital nerves prevents potential dyesthesia and parasthesia.
Pitfalls
• Scalp fixation with excessive tension will lead to scar widening and alopecia.
• As described above, improperly planned hair bearing and anterior hairline incisions can also lead to unfavorable scars and excessively elevated frontal hairlines.
• Excessive central muscle release with central periosteal fixation can result in surprised look.
Summary of steps
1. Preoperative markings in the sitting position.
4. Dissection to superior orbital rim with preservation of frontal branch of facial nerve and central forehead neurovascular bundles.
5. Corrugator muscle excision.
6. Permanent suture placement in galea aponeurosis for brow suspension.
Connell BF, Lambros VS, Neurohr GH. The forehead lift: techniques to avoid complications and produce optimal results. Aesthet Plast Surg. 1989;13:217.
Muzaffar AR, Mendelson BC, Adams WP, Jr. Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast Reconstr Surg. 2002;110:873–884.
Ortiz-Monasterio F. Aesthetic surgery of the facial skeleton: the forehead. Clin Plast Surg. 1991;18:19.
Paul MD. The evolution of the brow lift in aesthetic plastic surgery. Plast Reconstr Surg. 2001;108:1409.
Vinas JC, Caviglia C, Cortinas JL. Forehead rhytidoplasty and brow lifting. Plast Reconstr Surg. 1976;57:445.
Yaremchuk MJ, OSullivan N, Benslimane F. Reversing brow lifts. Aesthet Surg J. 2007;27:367–375.









