18. Cor Pulmonale
Definition
Cor pulmonale is the alteration of the structure and function of the right ventricle as the result of a primary respiratory disorder. Pulmonary hypertension generally results from the connection between the primary lung dysfunction and the heart.
Incidence
Of all patients in the United States with heart disease concomitant with a form of chronic obstructive pulmonary disease (COPD), approximately 6% to 7% will develop cor pulmonale. Exact determination of the incidence of this disease is difficult since not all patients with COPD develop cor pulmonale. The incidence is heavily dependent on “local” conditions, such as local air quality, cigarette smoking, and many other lung disease risk factors.
Etiology
Numerous pathophysiologic mechanisms may produce pulmonary hypertension (see box below). Cor pulmonale is a subsequent pathophysiologic development. The involvement of the right ventricle is somewhat different, depending on whether the underlying condition is chronic or acute. In chronic cor pulmonale, the right ventricle hypertrophies over time; in an acute development situation, the right ventricle becomes dilated to the point of dysfunction.
Pathophysiologic Mechanisms Leading to Cor Pulmonale
• Idiopathic primary pulmonary hypertension
• Increased blood viscosity resulting from blood dyscrasias
• Pulmonary vascular bed compromise as the result of lung disease(s)
• Pulmonary vasoconstriction secondary to alveolar hypoxia or acidemia
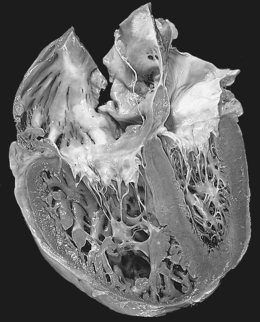 |
| Cor Pulmonale. Chronic cor pulmonale, characterized by a markedly dilated and hypertrophied right ventricle, with thickened free wall and hypertrophied trabeculae (apical four-chamber view of heart, right ventricle on left). The shape of the left ventricle (to the right) has been distorted by the right ventricular enlargement. |
Signs and Symptoms
• Anginal chest pain
• Cough
• Dyspnea on exertion
• Fatigue
• Hemoptysis
• Hoarseness due to left recurrent laryngeal nerve compression (rare)
• Hypoxemia
• Syncope on exertion
• Tachypnea
In Advanced Disease
• Anorexia
• Passive hepatic congestion due to severe right ventricular failure
• Right upper quadrant discomfort
Medical Management
Prognosis is typically poor once cor pulmonale develops as a result of the primary pulmonary disease. The 5-year survival rate is only around 30%.
The patient with acute cor pulmonale requires intense cardiopulmonary support, including fluid loading and vasoconstrictor administration. The primary cause should be determined and corrected, to the extent possible, as soon as possible. If the cause is massive pulmonary embolism, administration of thrombolytic agents should be strongly considered and weighed against the possible need for surgical embolectomy.
Chronic cor pulmonale employs different treatments in various combinations to optimize the long-term management of the disease. The treatment options include oxygen therapy, diuretic administration, vasodilator medications, cardiac glycosides, theophylline, and anticoagulation.
Surgical intervention is indicated predominately for acute cor pulmonale. Phlebotomy may be utilized in the patient with chronic cor pulmonale and chronic hypoxia resulting in polycythemia with hematocrit values ≥65%. Pulmonary embolectomy has proven effective in unresolved pulmonary embolus (emboli) producing pulmonary hypertension. The patient in the terminal phase of the disease, which is further complicated by cor pulmonale, may be treated by transplantation of one lung, both lungs, or heart and lungs.
Complications
• Death
• Hypoxia
• Passive hepatic congestion
• Pedal edema
• Syncope
Anesthesia Implications
A balloon flotation pulmonary artery catheter should be an integral part of monitoring for the patient with cor pulmonale. Once placed, the device provides continuous assessment of pulmonary artery pressure, right ventricular pressure, right ventricular myocardial oxygen demand/supply balance, and pulmonary function. The pulmonary artery catheter can help distinguish between left ventricular failure and respiratory failure. Mixed venous blood sampling provides more accurate information and is a more sensitive indicator of pulmonary dysfunction than the Pao 2 values obtained from arterial blood gas analysis alone.
The degree of pulmonary hypertension has a significant impact on anesthetic management. When pulmonary hypertension is present without concomitant right ventricular failure, the patient may benefit from the use of the potent volatile inhalational anesthetic agents. High concentrations of the volatile agents may decrease hypoxic vasoconstriction and thus decrease the potential for hypoxemia.
If the patient also has pulmonary parenchymal disease and a significant bronchospastic component, incorporation of ketamine may be indicated.
Nitrous oxide may be used, but caution is highly advised because of its tendency to produce increased pulmonary artery pressure.
Hypoxia, hypercarbia, acidosis, and hypothermia should be avoided because of the predisposition to produce pulmonary vasoconstriction.
The primary objective is maintaining or preserving right ventricular function while facing the elevated right ventricular afterload. With this objective in mind, a total intravenous anesthetic technique (TIVA) utilizing an opioid (fentanyl or remifentanil) and a sedative/hypnotic (midazolam and/or propofol) may best facilitate this objective. Further concerns include ventricular preload, heart rate, and the ventricular inotropic state along with ventricular afterload.
Inotropic support is frequently necessary, particularly for the patient with cor pulmonale. The pulmonary effects of the many inotropic agents should be strongly considered before finalizing the choice for any inotropic support that may become necessary. Dobutamine and milrinone are very effective at reducing pulmonary artery pressure and pulmonary vascular resistance in patients with right ventricular failure without concomitant systemic hypotension.
Norepinephrine and epinephrine are the catecholamines of choice for cases where right ventricular contractility is significantly or severely impaired or when right ventricular perfusion pressures need to be maintained. Vasopressin is singularly effective in treating systemic hypotension in patients with right ventricular failure.
Patients may be receiving vasodilators to reduce the right ventricular afterload. These include: sodium nitroprusside, nitroglycerin, milrinone, adenosine, nifedipine, amlodipine, and prostaglandin E 1.
Nitric oxide (NO) is a selective pulmonary vascular dilator and is an effective treatment for pulmonary hypertension.
If a patient has been receiving chronic treatment with epoprostenol, inadvertent discontinuation may precipitate a fatal episode of pulmonary hypertension.






