Chapter 9 Contact dermatitis
Marks JG, Elsner P, DeLeo VA: Contact and occupational dermatology, ed 3, St Louis, 2002, Mosby.
Table 9-1. Comparison of Irritant and Allergic Contact Dermatitis
| IRRITANT | ALLERGIC | |
|---|---|---|
| Examples | Water, soap | Nickel, fragrance, hair dye |
| Number of compounds | Many | Fewer |
| Distribution of reaction | Localized | May spread beyond area of maximal contact and become generalized |
| Concentration of agent needed to elicit reaction | High | Can be minute |
| Time course | Immediate to late | Sensitization in 2 weeks; elicitation takes 24–72 hrs |
| Immunology | Nonspecific | Specific type IV delayed hypersensitivity reaction |
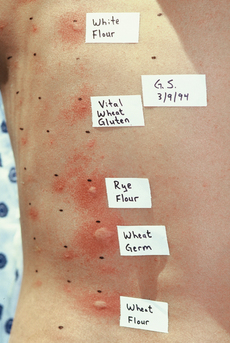
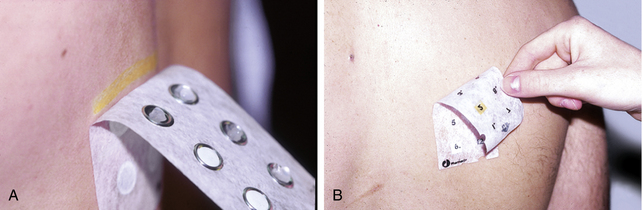
| Diagnostic test | None | Patch test |
Li L, Cruz P: Allergic contact dermatitis: pathophysiology applied to future therapy, Dermatol Thera 17:219–223, 2004.
Table 9-2. Location of Contact Dermatitis and Suspicious Agents
| LOCATION | SUSPICIOUS AGENT |
|---|---|
| Eyelids | Nail polish, eye makeup, airborne allergens |
| Earlobes or neck | Metal jewelry |
| Forehead, scalp margins | Hair dyes |
| Face | Cosmetic fragrances and preservatives, airborne allergens |
| Axilla | Deodorants |
| Hands | Gloves, occupational contacts |
| Waistband | Elastic |
| Dorsal feet | Shoes |
Table 9-3. Allergens Evaluated by the True Test and the Finn Chamber Test
| ALLERGEN | SOURCES |
|---|---|
| Benzocaine 5% | Topical anesthetic |
| Caine mix | Topical anesthetic |
| Nickel sulfate 2.5% | Metal jewelry |
| Potassium dichromate 0.25% | Leather, cement |
| Cobalt | Metal jewelry, paint |
| Neomycin sulfate 20% | Topical antibiotics |
| p-Phenylenediamine 1% | Hair dye |
| Ethylenediamine 1% | Topical medications |
| Cinnamaldehyde 1% | Perfume, flavors |
| Balsam of Peru 25% | Perfume, medications |
| Fragrance mix | Perfume, flavors |
| Formaldehyde 1% | Preservative, fabric finishes |
| Quaternium-15 2% | Cosmetic and industrial preservative |
| Imidazolidinyl urea 2% | Cosmetic preservative |
| Paraben mix | Cosmetic preservative |
| Thimerosal | Cosmetic and medicament preservative |
| Cl+Me− Isothiazoline (MCI/MI) | Cosmetic and industrial preservative |
| Lanolin alcohol 30% | Topical skin care products |
| Epoxy resin 1% | Glues, plastics |
| p-tert-butylphenol formaldehyde resin 1% | Glues |
| Colophony (resin) 2% | Adhesives, solder flux |
| Mercaptobenzothiazole 1% | Rubber, fungicide |
| Carba mix 3% | Rubber, fungicide |
| Thiuram mix 1% | Rubber, fungicide |
| Mercapto mix 1% | Rubber, fungicide |
| Black rubber mix 0.6% | Black rubber |
| Budesonide | Topical corticosteroid |
| Tixocortol 21-pivalate | Topical corticosteroid |
Rietschel RL, Fowler JF: Treatment of contact dermatitis. In Rietschel RL, Fowler JF, editors: Fisher’s contact dermatitis, ed 6, Hamilton, Ontario, BC Decker, 2008, pp 722–729.