31 Constrictive pericarditis
Salient features
Examination
• The patient may appear cachectic.
• Pulse may be regular or irregularly irregular (one-third have atrial fibrillation).
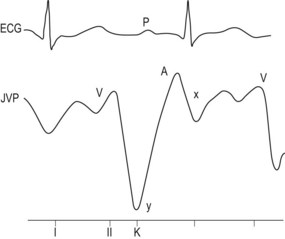
• Prominent ‘x’ and ‘y’ descents in the JVP and the level of the jugular venous pulse may rise with inspiration (Kussmaul’s sign; Fig. 31.1).
• Apex beat is not palpable and there may be apical systolic retraction (Broadbent sign).
• Early diastolic pericardial knock along the left sternal border, which may be accentuated by inspiration.
• Lungs are clear but there may be pleural effusion.
Advanced-level questions
What is the mechanism for pericardial knock?
It is caused by the abrupt halting of rapid ventricular filling.
How would you investigate a patient with constrictive pericarditis?
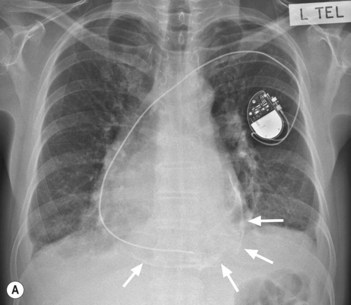
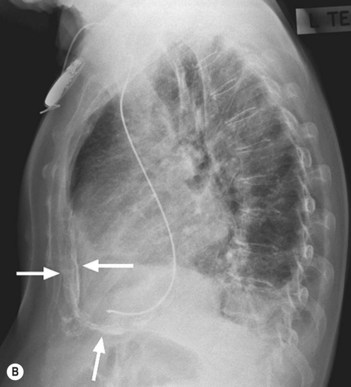
• Chest radiograph typically shows normal heart size and pericardial calcification (note the combination of pulsus paradoxus, pericardial knock and pericardial calcification favour the diagnosis of constrictive pericarditis) (Fig. 31.2).
• ECG shows low voltage complexes, non-specific T wave flattening or atrial fibrillation.
• Echocardiogram shows myocardial thickness is normal and may reveal thickened pericardium; normal ventricular dimensions with enlarged atria and good systolic and poor diastolic dysfunction. Doppler shows increased right ventricular systolic and decreased left ventricular systolic velocity with inspiration, expiratory augmentation of hepatic-vein diastolic flow reversal.
• CT or MRI shows normal myocardial thickness usually and pericardial thickening and calcification.
• Cardiac catheterization typically shows identical left and right ventricular filling pressures and pulmonary artery systolic pressure usually <45 mmHg, with normal myocardial biopsy: haemodynamic tracings show rapid ‘y’ descent in atrial pressure and early dip in diastolic pressure, with pressure rise to plateau in mid or late diastole. Cardiac tamponade and constrictive pericarditis are basically similar in restricting the filling of the heart and raising the systemic and pulmonary venous pressures. The venous pressure waveforms differ, however, reflecting a single wave of forward flow (during systole) in tamponade, compared with a biphasic pattern (a lesser wave in systole and a greater wave in early diastole) in constrictive conditions.
How would you treat a patient with constrictive pericarditis?
• Surgery is the only satisfactory treatment: complete surgical resection of the pericardium (myocardial inflammation or fibrosis may delay symptomatic response).
• Patients with tuberculous pericarditis should be pretreated for TB; if the diagnosis is confirmed after pericardial resection, full anti-tuberculous therapy should be continued for 6–12 months after resection.