Pelvic Congestion Syndrome
Synonyms/Description
Etiology
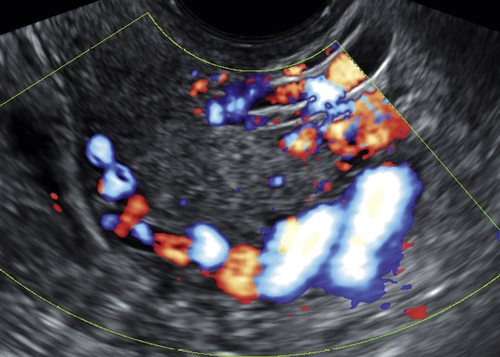
Ultrasound Findings
Differential Diagnosis
Clinical Aspects and Recommendations
Suggested Reading
Beard R.W., Reginald P.W., Wadsworth J. Clinical features of women with chronic lower abdominal pain and pelvic congestion. Br J Obstet Gynecol. 1988;95:153.
Hobbs J.T. The pelvic congestion syndrome. Br J Hosp Med. 1990;43:200.
Ignacio E.A., Dua R., Sarin S., Harper A.S., Yim D., Mathur V., Venbrux A.C. Pelvic congestion syndrome: diagnosis and treatment. Semin Intervent Radiol. 2008;25:361–368.
Tu F.F., Hahn D., Steege J.F. Pelvic congestion syndrome-associated pelvic pain: a systematic review of diagnosis and management. Obstet Gynecol Surv. 2010;65:332–340.