8 Congenital Heart Disease
Atrial Septal Defects
Key Points
All Atrial Septal Defects (ASD) (Tables 8-1 and 8-2)
TABLE 8-1 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING PATIENTS WITH AN ATRIAL SEPTAL DEFECT
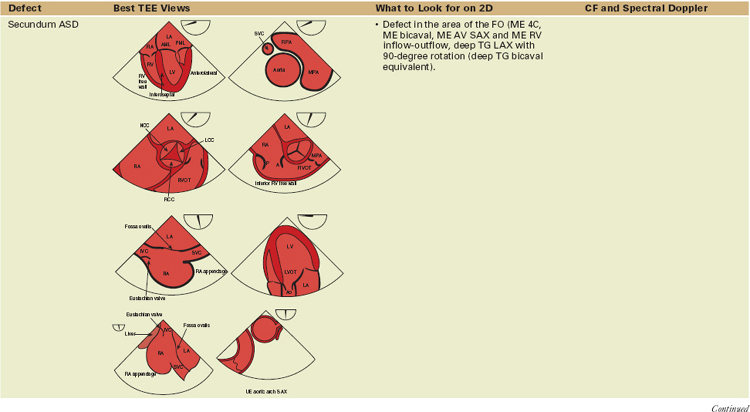
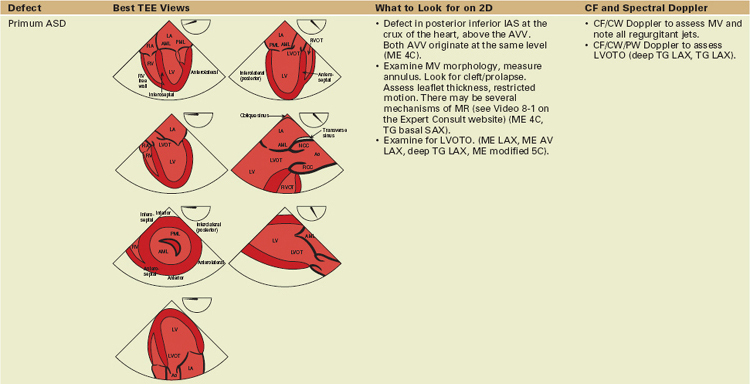
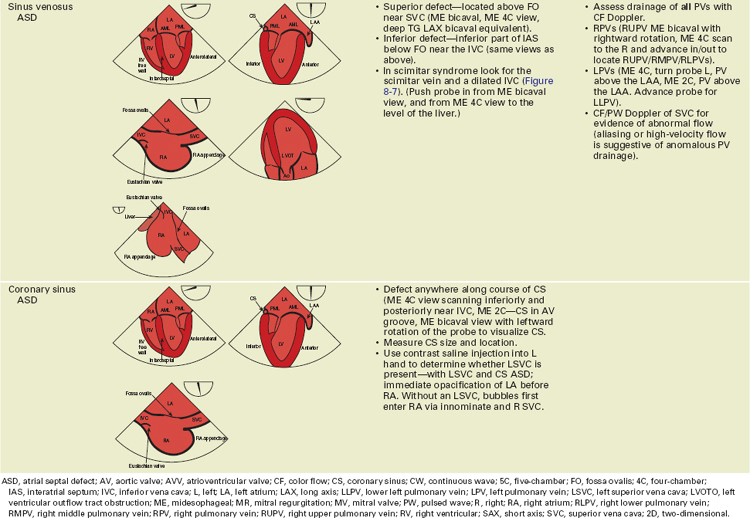
| Defect | What to Look for on 2D | CF and Spectral Doppler |
|---|---|---|
| All ASDs |
• Examine morphology/function of PulmV. Look for number of leaflets, doming leaflets, commissural fusion, restricted motion (ME AV SAX, ME asc aortic SAX, ME RV inflow-outflow, UE aortic arch, SAX).
|
asc, ascending; ASD, atrial septal defect; AV aortic valve; 4C, four-chamber; CF, color flow; IAS, interatrial septum; L, left; LAA, left atrial appendage; LSVC, left superior vena cava; LUPV, left upper pulmonary vein; ME, midesophageal; MR, mitral regurgitation; MV, mitral valve; PAP, pulmonary artery pressure; PBF, pulmonary blood flow; PS, pulmonic stenosis; PulmV, pulmonary valve; PV, pulmonary vein; PW, pulsed wave; R, right; RAE, right atrial enlargement; RV, right ventricular; RVE, right ventricular enlargement; RVH, right ventricular hypertrophy; RVP, right ventricular pressure; SAX, short axis; TR, tricuspid regurgitation; TV, tricuspid valve; 2C, two-chamber; 2D, two-dimensional; UE, upper esophageal.
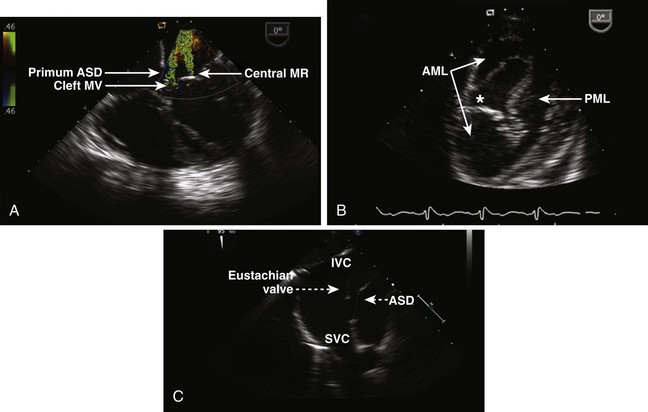
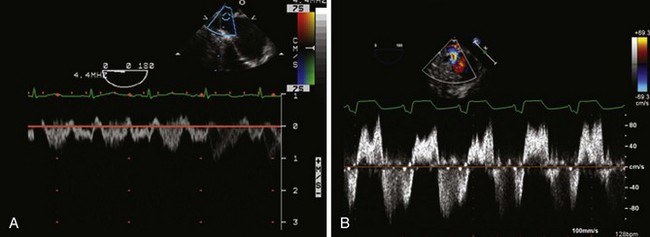
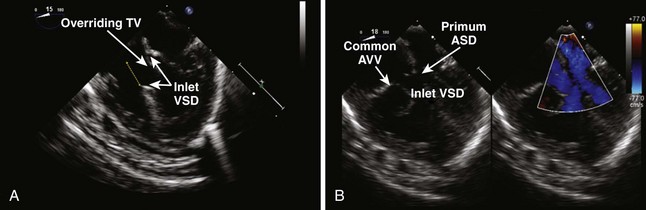
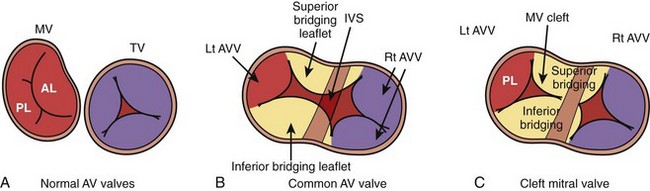
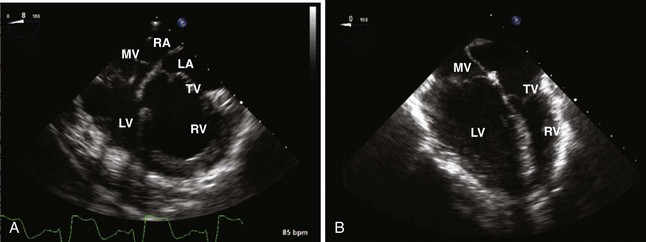
Primum Atrial Septal Defects (Figure 8-1A)
Secundum Atrial Septal Defects (see Figure 8-1C)
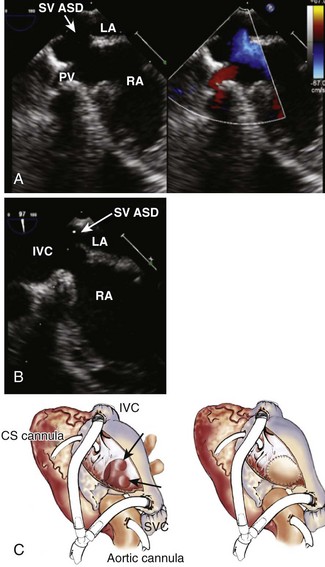
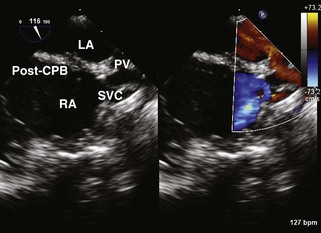
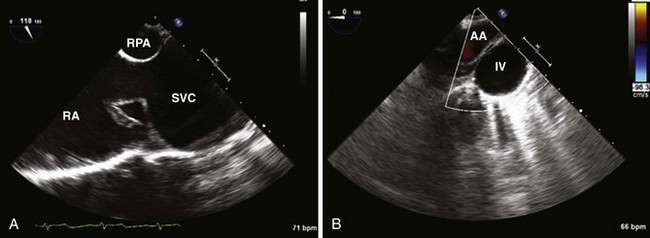
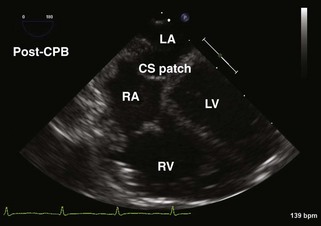
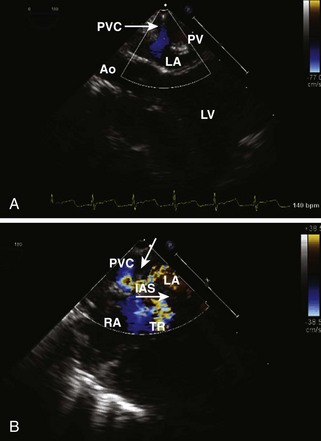
Sinus Venosus Atrial Septal Defects (Figure 8-3)
Principles of Surgical/Interventional Management
Sinus Venosus Atrial Septal Defects
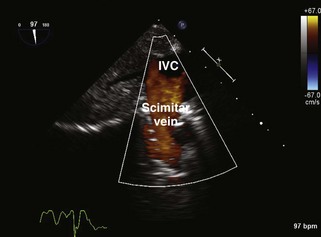
Scimitar Syndrome
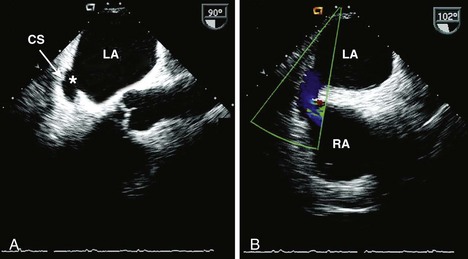
Coronary Sinus Atrial Septal Defects
Postoperative TEE Assessment after Atrial Septal Defect Repair
Ventricular Septal Defects
Key Points
All Ventricular Septal Defects (Tables 8-3 to 8-5)
TABLE 8-3 SURGICAL APPROACH TO VENTRICULAR SEPTAL DEFECT CLOSURE
| Most Common Surgical Approach | Defect | Additional Facts |
|---|---|---|
| RA |
DORV, double-outlet right ventricle; LV, left ventricle; LV, left ventricular; RA, right atrium; RA, right atrial; RV, right ventricle; RV, right ventricular; TOF, tetralogy of Fallot; TV, tricuspid valve; VSD, ventricular septal defect.
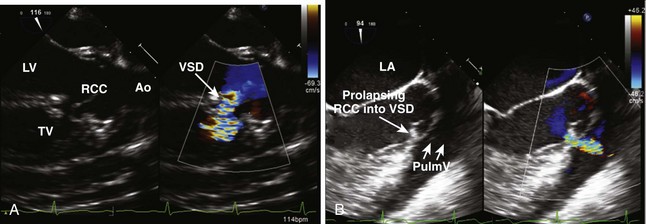
TABLE 8-4 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING PATIENTS WITH A VENTRICULAR SEPTAL DEFECT
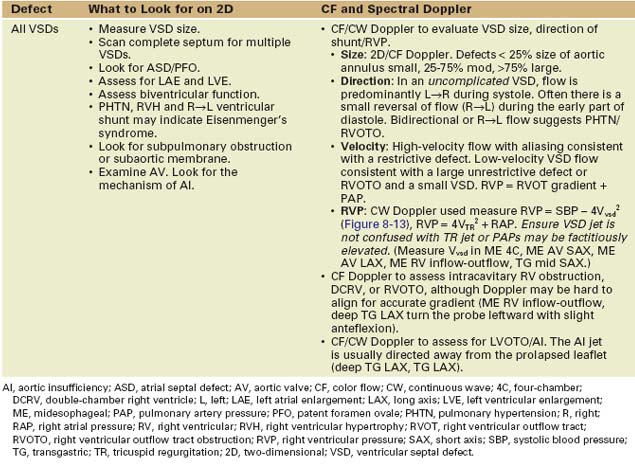
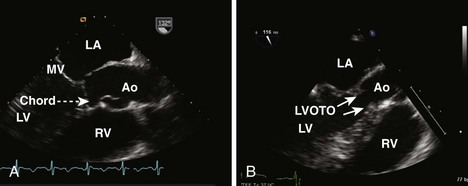
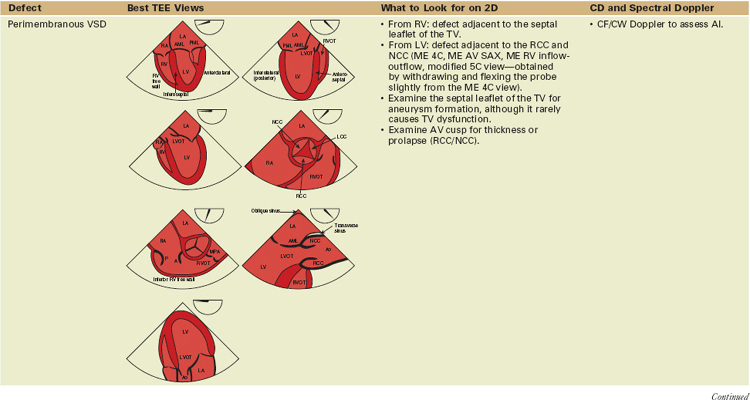
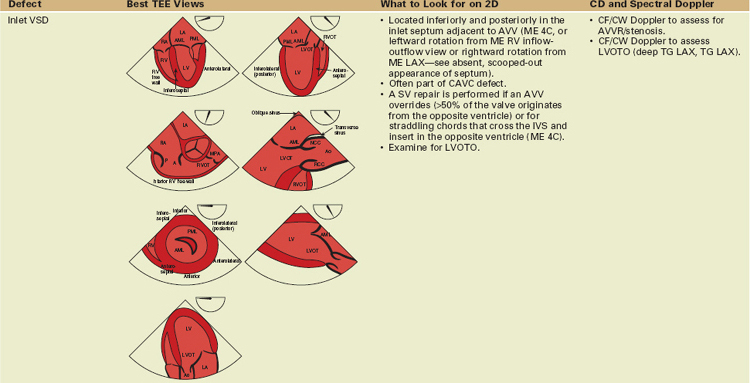
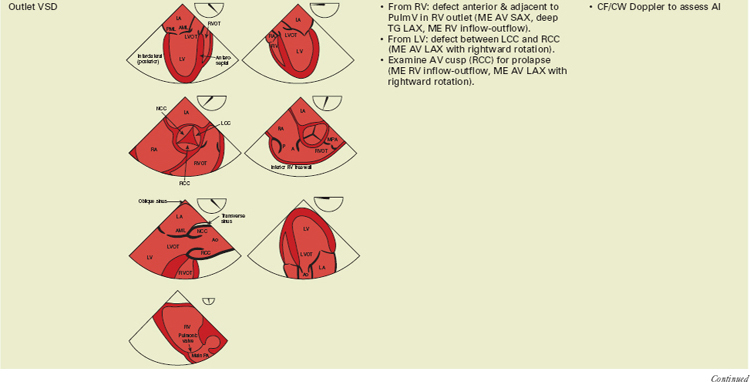
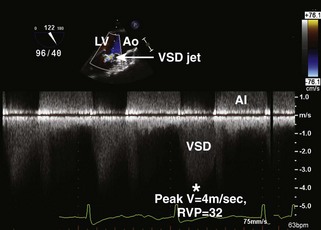
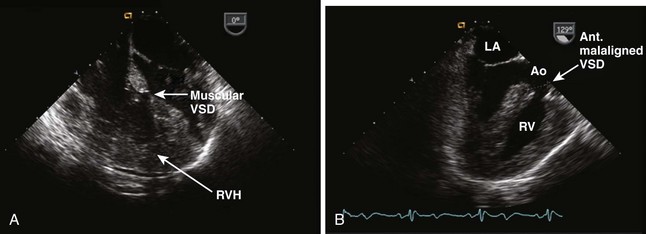
Perimembranous Defects (Figure 8-9A)
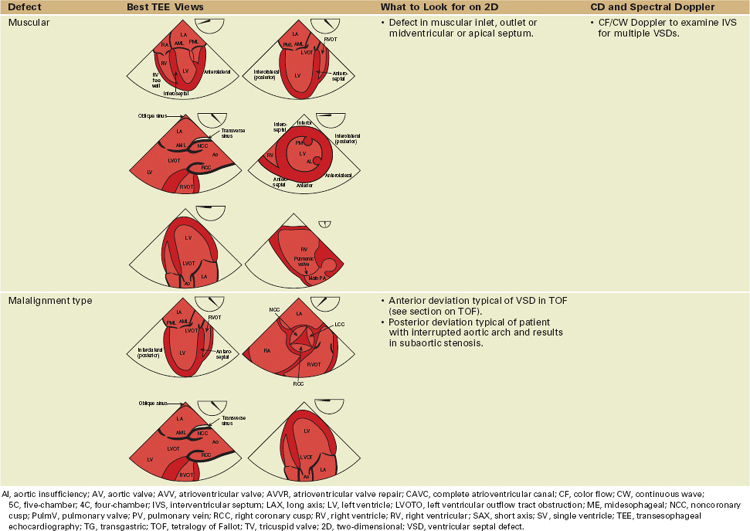
Outlet Defects (see Figure 8-9B)
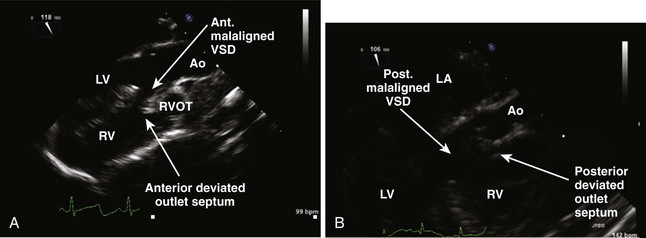
Malalignment Type (Figure 8-12)
Principles of Surgical Management
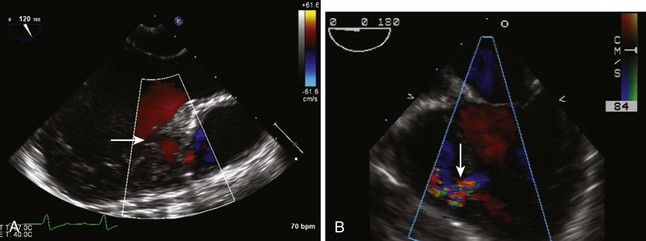
Postoperative TEE Assessment after Primary or Revision Ventricular Septal Defect Repair
Atrioventricular Canal Defects (Table 8-6)
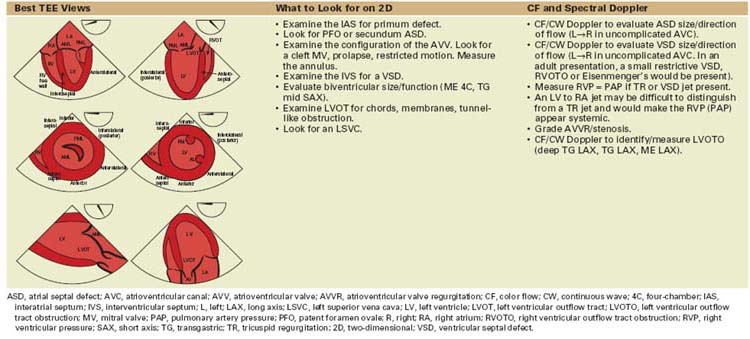
TABLE 8-6 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING PATIENTS WITH REPAIRED OR UNREPAIRED ATRIOVENTRICULAR CANAL DEFECTS
Key Points
Transitional Canal
Common Atrioventricular Canal
Principles of Surgical Management
Tetralogy of Fallot
Key Points
All Tetralogy of Fallot (Tables 8-7 and 8-8)
AI, aortic insufficiency; APV, absent pulmonary valve; ASD, atrial septal defect; AV, aortic valve; AVC, atrioventricular canal; AVVR, atrioventricular valve regurgitation; DORV, double-outlet right ventricle; L, left; MAPCAs, multiple aortopulmonary collateral arteries; PA, pulmonary artery; PFO, patent foramen ovale; PI, pulmonic insufficiency; PS, pulmonic stenosis; PulmV, pulmonary valve; R, right; RA, right atrial; RV, right ventricle; RV, right ventricular; RVOTO, right ventricular outflow tract obstruction; TOF, tetralogy of Fallot; VSD, ventricular septal defect.
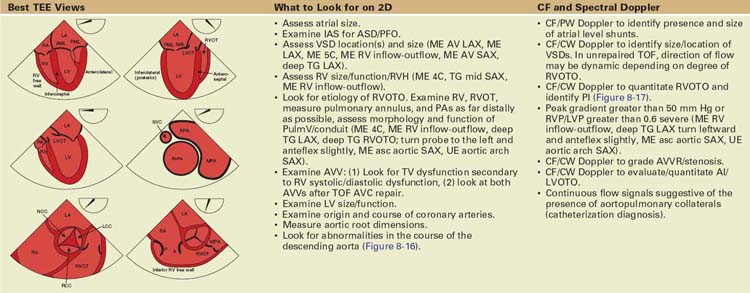
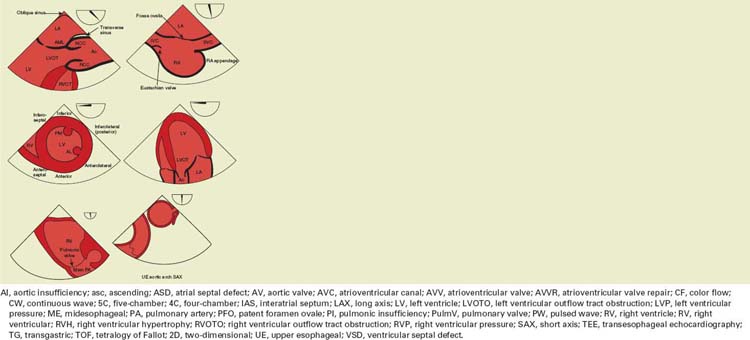
TABLE 8-8 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING REPAIRED/UNREPAIRED TETRALOGY OF FALLOT
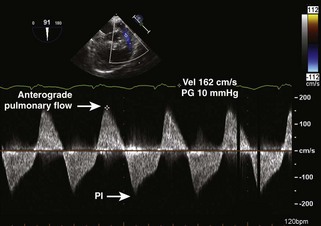
Tetralogy of Fallot with Pulmonic Stenosis
Tetralogy of Fallot with Pulmonary Atresia
Tetralogy of Fallot with Absent Pulmonary Valve
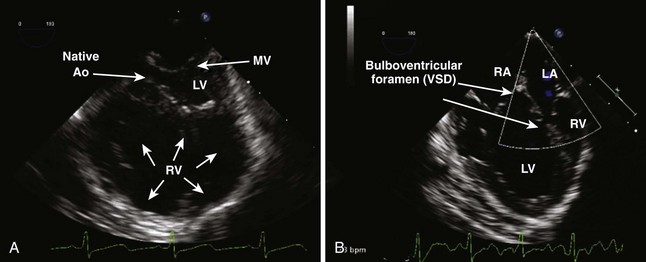
Double-Outlet Right Ventricle–Tetralogy of Fallot Spectrum
Postoperative TEE Assessment after Primary Repair/Reoperation of Tetralogy of Fallot
Transposition of the Great Arteries
Key Points
All Transposition of the Great Arteries (Table 8-9)
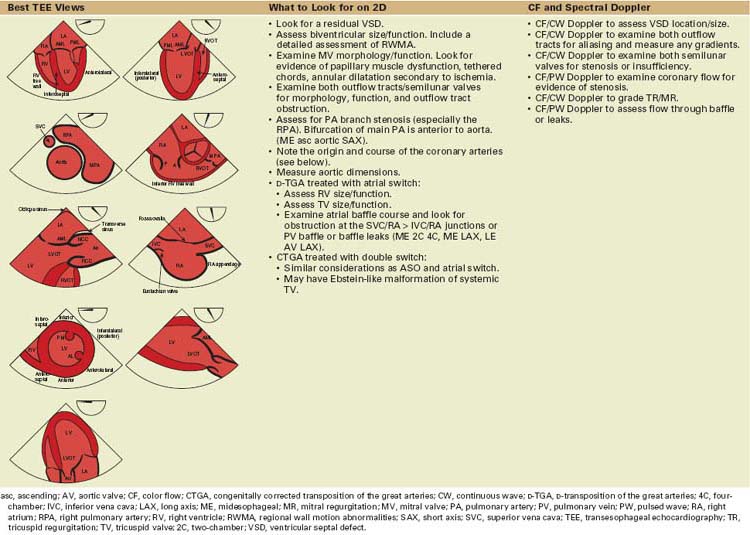
TABLE 8-9 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING REPAIRED D-TRANSPOSITION OF THE GREAT ARTERIES
D-Transposition of the Great Arteries
Surgical Management
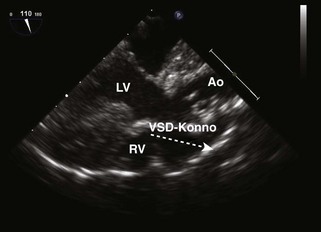
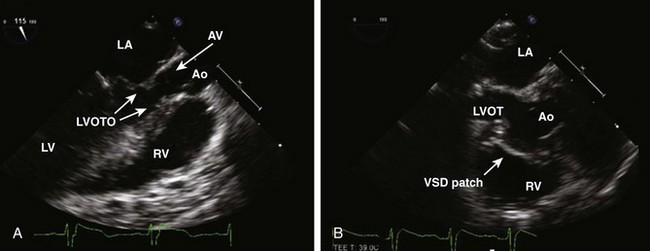
Figure 8-19 ME AV LAX view post Nikaidoh procedure. This patient had TGA with a VSD and PS. The anterior aortic root was translocated posteriorly and is now the LV outflow vessel. The LVOT was enlarged (Konno procedure, see “Left Ventricular Outflow Tract Abnormalities”) and the VSD patch is clearly seen. The stippled arrow is where a patch is placed had a Rastelli been performed (in which case, the great vessels are not switched). The VSD patch is oriented in a more anatomic position with a Nikaidoh. The RV-PA conduit is not visible in this view (see text).
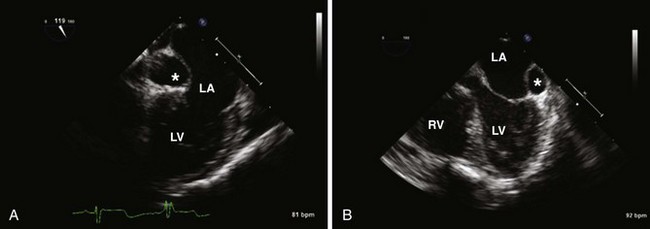
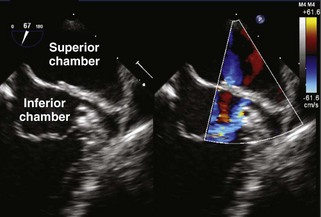
Total Anomalous Pulmonary Venous Drainage (Table 8-10)
TABLE 8-10 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING PRIMARY/REVISION TOTAL ANOMALOUS PULMONARY VENOUS DRAINAGE
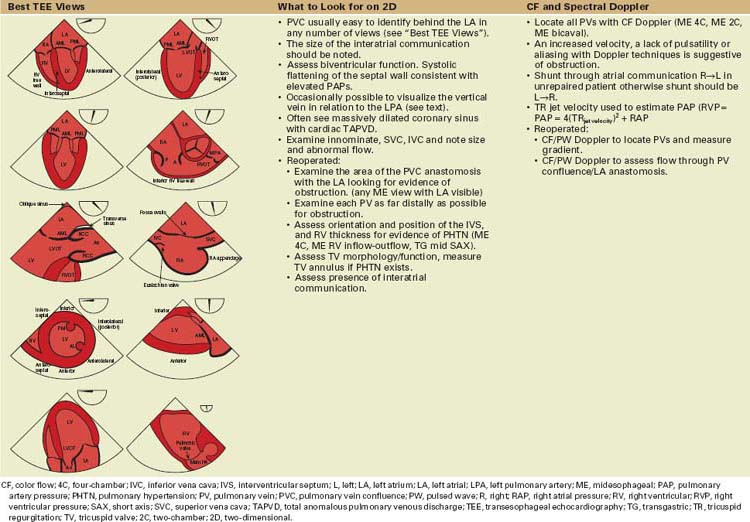
Key Points
Surgical Management
Reoperations/Reinterventions
Truncus Arteriosus (Table 8-11)
TABLE 8-11 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING PATIENTS AFTER TRUNCUS ARTERIOSUS REPAIR
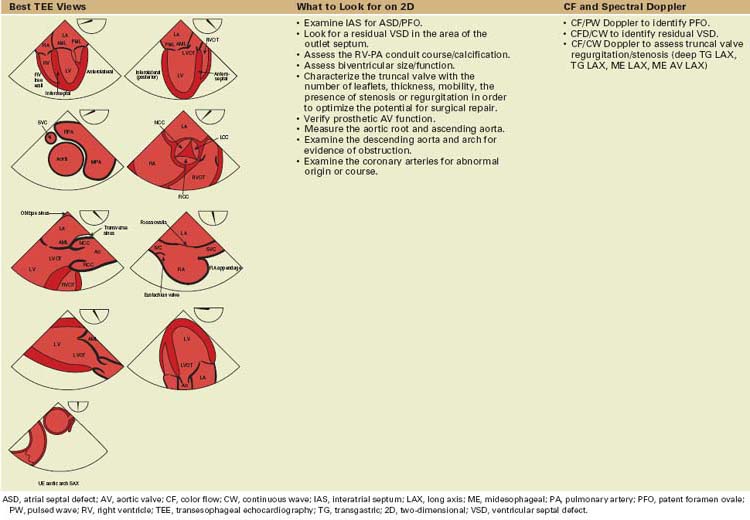
Key Points
Surgical and Interventional Management
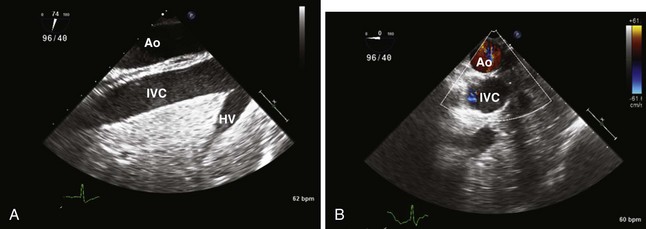
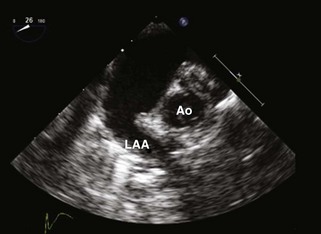
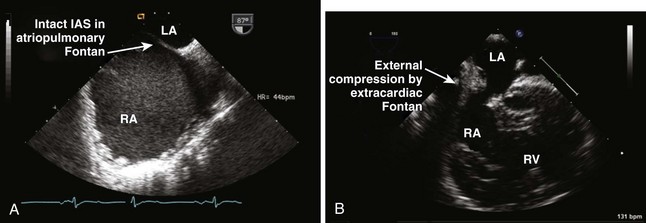
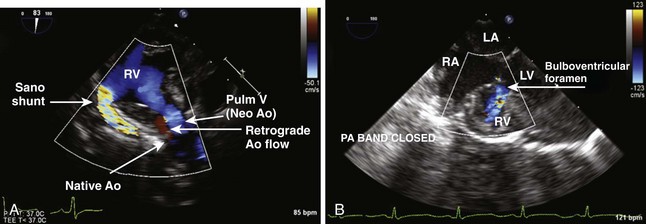
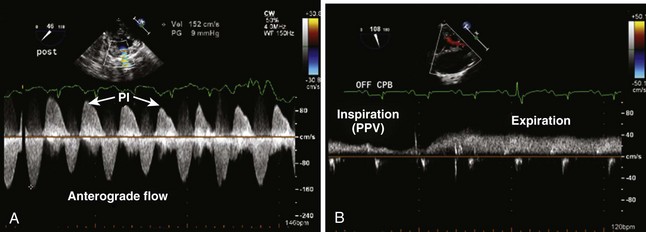
Single Ventricle
Key Points
TABLE 8-12 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING PATIENTS WITH SINGLE VENTRICLES
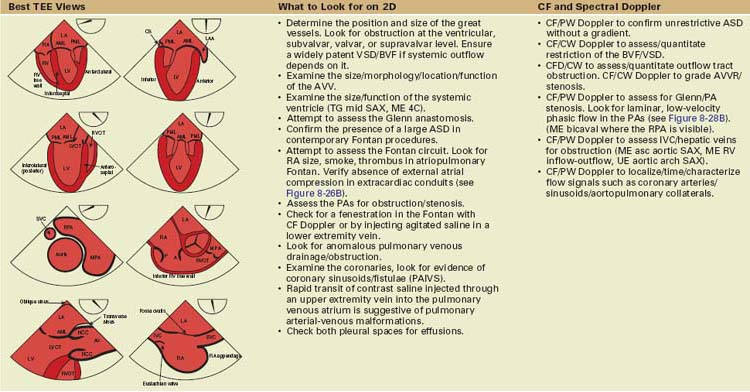
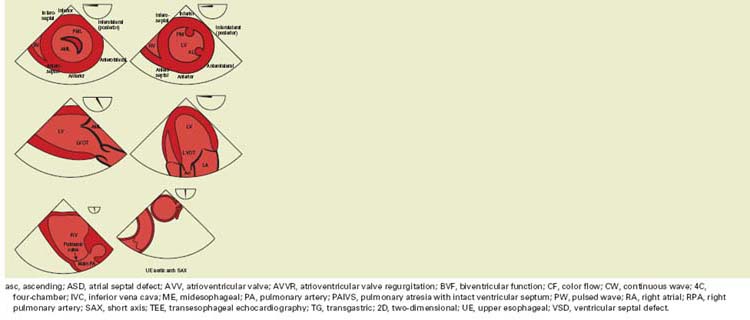
TABLE 8-13 SURGICAL AND INTERVENTIONAL MANAGEMENT FOR STAGE 1
| Defect | Surgical Options for Stage 1 | Additional Points |
|---|---|---|
| HLHS |
AVC, atrioventricular canal; BT, Blalock-Taussig; BVF, biventricular function; DILV, double-inlet left ventricle; DKS, Damus-Kaye-Stansel; HLHS, hypertrophic left heart syndrome; IVC, inferior vena cava; PA, pulmonary artery; PulmV, pulmonary valve; RV, right ventricle; RVDCA, right ventricle-dependent coronary artery; SV, single ventricle.
Stage 3
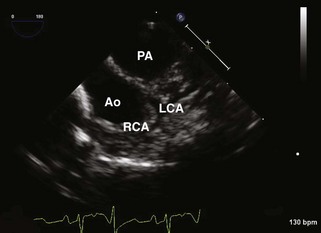
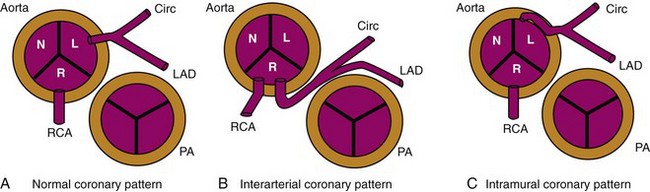
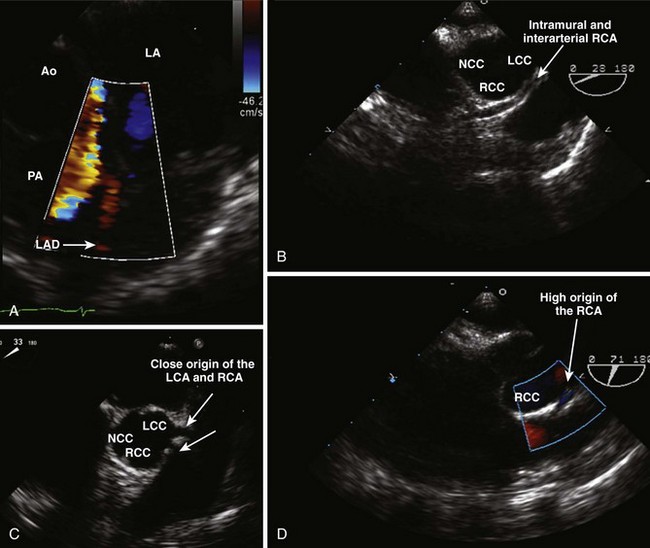
Coronary Artery Abnormalities
Key Points
Anomalous Origin of the Coronary Artery from the Aorta
Anomalous Origin of the Left Coronary Artery from the Pulmonary Artery
Coronary Artery Fistula
Basic Echocardiographic Principles When Imaging Coronary Arteries (Table 8-14)
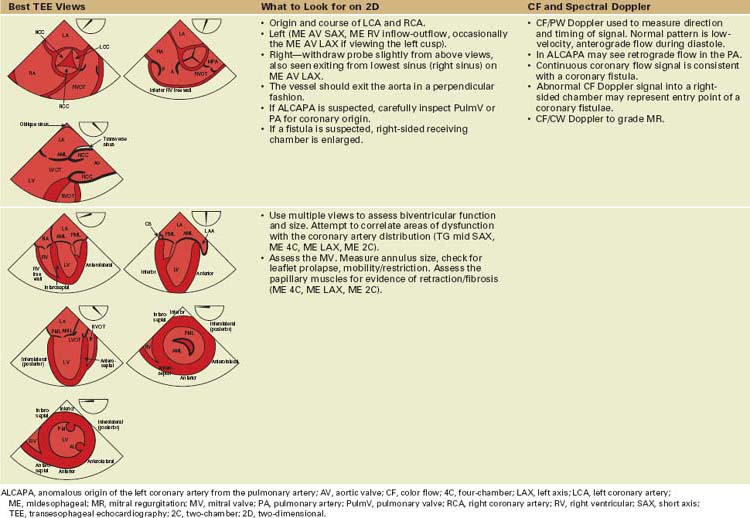
TABLE 8-14 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING FOR CONGENITAL CORONARY ARTERY ANOMALIES (see Figure 8-30)
Principles of Surgical/Interventional Management
Congenital Valvular Heart Disease
Tricuspid Valve
Key Points
Ebstein’s Anomaly (Table 8-15)
TABLE 8-15 BASIC ECHOCARDIOGRAPHIC FEATURES WHEN IMAGING UNREPAIRED OR PREVIOUSLY REPAIRED EBSTEIN’S ANOMALY
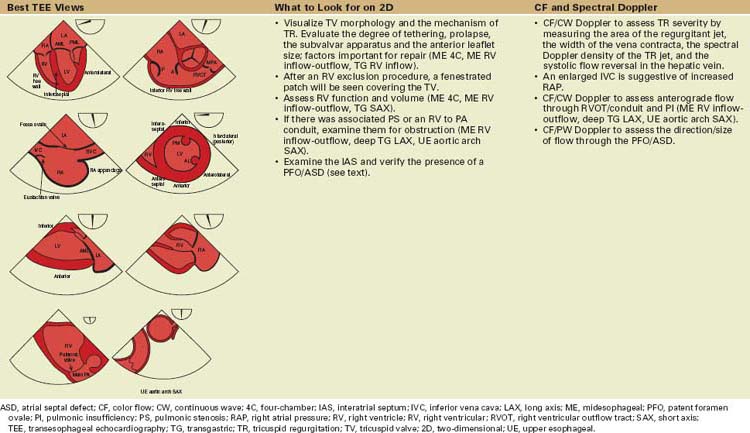
Surgical/Interventional Management (Table 8-16)
TABLE 8-16 DETAILS OF THE SURGICAL REPAIR IN PATIENTS WITH EBSTEIN’S ANOMALY
| Procedure | Key Facts |
|---|---|
| Valve repair |
ASD, atrial septal defect; IVC, inferior vena cava; LV, left ventricular; PA, pulmonary artery; PI, pulmonic insufficiency; PV, pulmonary vein; RV, right ventricle; RV, right ventricular; SV, single ventricle; SVC, superior vena cava; TV, tricuspid valve; TVR, tricuspid valve repair.
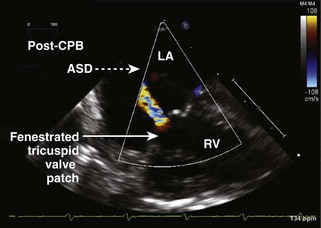
Postoperative TEE Assessment after Primary or Revision Surgery for Ebstein’s Anomaly
Pulmonary Valve
Key Points
Surgical and Interventional Management
Basic Echocardiographic Features When Imaging Pulmonary Valve or Conduit Abnormalities
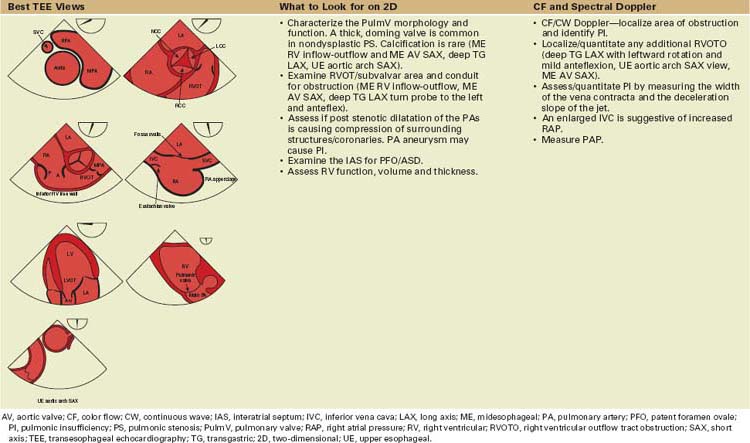
TABLE 8-17 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING PATIENTS WITH PULMONARY VALVE DISEASE
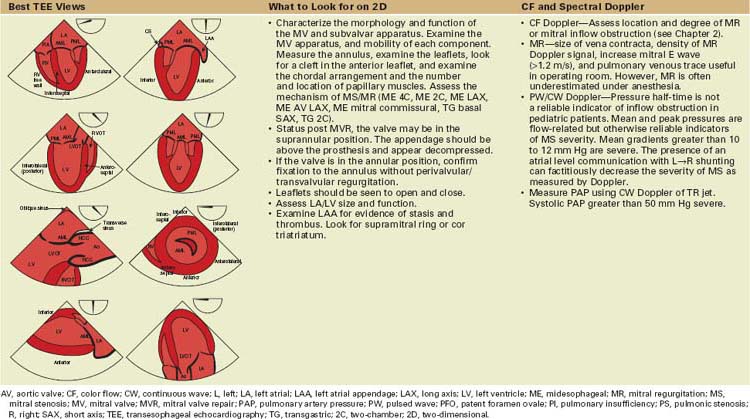
Mitral Valve (Table 8-18)
TABLE 8-18 BASIC ECHOCARDIOGRAPHIC FEATURES WHEN IMAGING THE PATIENT WITH A REPAIRED/REPLACED OR UNREPAIRED MITRAL VALVE
Key Points
Surgical and Interventional Management on the Mitral Valve
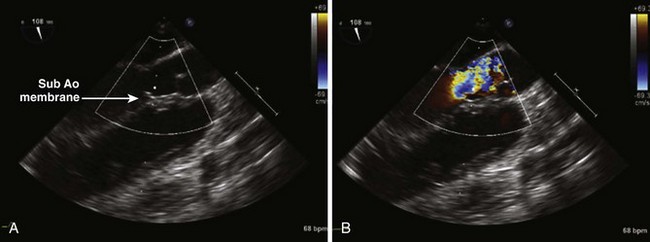
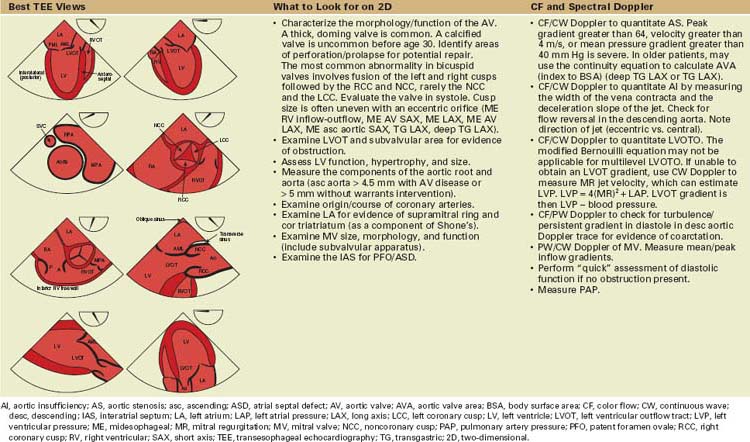
Aortic Valve/Left Ventricular Outflow Tract Abnormalities (Table 8-19)
TABLE 8-19 BASIC ECHOCARDIOGRAPHIC PRINCIPLES WHEN IMAGING THE LEFT VENTRICULAR OUTFLOW TRACT AND AORTIC VALVE
Key Points
Aortic Valve
Left Ventricular Outflow Tract
Aorta
Surgical/Interventional Management
Postoperative TEE Assessment after AV or LVOT Surgery
1 Operative Techniques in Thoracic and Cardiovascular Surgery. Philadelphia: Elsevier Inc.
2 Seminars in Thoracic and Cardiovascular Surgery series. Pediatric Cardiac Surgery Annual. Philadelphia: Elsevier Inc.
3 Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e1-e121. Epub 2008;November 14
Important resource. Overall management of the complex adult with congenital cardiac disease.
4 Russell I, Rouine-Rapp K, Stratmann G, Miller-Hance WC. Congenital heart disease in the adult: A review with internet-accessible transesophageal echocardiographic images. Anesth Analg. 2006;102:694-723.
5 Lai W, Mertens L, Cohen M, Geva T, editors. Echocardiography for Pediatric and Congenital Heart Disease. Boston: Wiley-Blackwell, 2009.