Congenital Heart Disease
Liliana Cohen and Daniel M. Shindler
Terminology and Associations
Where one congenital malformation can occur, others can occur.
So do a complete stepwise exam on everyone!!!
One congenital abnormality does not preclude another.
As a matter of fact, there are associations:
Atrial septal defect—pulmonic stenosis
Bicuspid aortic valve—coarctation of the aorta
Ebstein’s anomaly of the tricuspid valve—atrial septal defect.
You say pairs of associations are boring?
1. Pulmonic stenosis—use transgastric and high esophageal views to image the pulmonic valve, determine thickness and look for doming (indicative of fused commissures).
2. Right ventricular outflow obstruction—mid esophagus 90 degree views and transgastric views (when you get good).
3. Ventricular septal defect—120 degree mid esophagus, rotate your wrist until you find it.
You should know the difference between overriding and straddling:
On the echo of tetralogy: the aorta “hovers over” the ventricular septum. That is called overriding.
In atrio-ventricular canal defects an abnormal tricuspid valve “floats” over the ventricular septum AND may have chordal attachments to BOTH sides of the ventricular septum (like the legs of the rider on a horse – it straddles the septum). The presence of straddling needs to be sought during the TEE because it affects surgical repairability.
History
Before you start scanning, there is no shame in CHEATING. Talk to the patient and get the history.
Who did the operation (surgeon and institution)?
Where is the scar—sternum or side of chest (ductus or coarctation repair)?
But wait, there is more: the coronary arteries need to be moved back too.
Physical Findings and Labs
It’s gonna be bad if there is cyanosis, clubbing, or polycythemia!
Are the lungs clear or congested on that chest X-ray (that you never look at)?
More Names of Operations
If you got a little befuddled by the name of an operation, here are more:
Anything “Rastelli”—look for a conduit (or at least a patch).
Sometimes the name order is changed if Dr. Kaye’s or Dr. Stansel’s people are operating.
Using Descriptive Echocardiographic Lingo in Transposition
Here are some suggestions for communicating with the grumpy person holding the scalpel on the other side of the plastic curtain.
Transposition of the great vessels gets confusing real quick if you insist on using certain terms.
Don’t say “right” ventricle—describe the ventricle instead.
Don’t say pulmonary artery—say: the great vessel that bifurcates and has no coronary ostia.
Ventricular Septal Defect
The most common restrictive ventricular septal defect is the perimembranous defect.
So… always look for high-velocity systolic jets in the right ventricular cavity.
The Natural History May Fool You
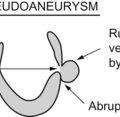
The lack of support in the area of the subaortic ventricular septal defect may enlarge (or as President Bush would say: “aneurysmificate”) the right sinus of valsalva.
Sinus of Valsalva aneurysms may rupture into the right ventricle.
Surgery to close a ruptured sinus of Valsalva aneurym may be misguided by the echocardiographer who misses a persistent ventricular septal defect that started the whole thing. The vsd signal is masked by the rip-roaring systolic and diastolic Doppler signal from the ruptured sinus of Valsalva aneurysm.
You tell the surgeon to close the ruptured sinus of Valsalva aneurysm, but you find a persistent subaortic ventricular septal defect AFTER they come off the pump and are ready to close the chest (rip-roaring systolic and diastolic Doppler signal is not there to fool you anymore).
Atrial Septal Defects
Atrial septal defects may remain undiagnosed until adulthood. The murmur is subtle and can be missed. Yes, yes, fixed splitting of the second heart sound is a valuable clue.
Pulmonary Valve Stenosis
The physical exam of severe pulmonic stenosis includes a harsh, loud, widely disseminated murmur. It sounds like you are clearing your throat. Doppler examination parallel to the stenotic jet (harder to do than it would seem from the high esophagus) gives the gradient. Look at the pulmonic valve carefully before they start cutting the patient for a Ross procedure. Right ventricular hypertrophy is also a clue to an abnormality causing pressure overload.
Bicuspid Aortic Valve
Always look for associated coarctation. Aortic dissection should also be kept in mind.
All stenotic valves with fused commissures exhibit a doming “hockey stick” appearance.
Patent Ductus Arteriosus
You know this one since cardiac embryology.
But how many have you diagnosed?
Young hypertensives need TEE scrutiny of the aortic isthmus for coarctation.
Ebstein’s Abnormality of the Tricuspid Valve
Mrs. Ebstein’s boy (the doctor) came up with this one—a while back in the sixties (1866).
Questions
1. Which of these congenital abnormalities is most likely to result in a dilated right ventricle?
D Transposition of the great vessels (D-TGA)
E Anatomically corrected transposition of the great vessels (L-TGA)
2. Which association is uncommon?
A Pulmonic stenosis—atrial septal defect
B Pulmonic stenosis—ventricular septal defect
C Bicuspid aortic valve—coarctation of the aorta
3. Sinus of Valsalva aneurysm ruptures into the:
4. All the following require TEE evaluation of cardiac veins EXCEPT:
5. The following can be present AFTER “definitive” tetralogy repair EXCEPT:
6. AV canal defects are associated with the following EXCEPT:
7. The following eponyms go with transposition EXCEPT:
8. Least likely to permanently improve symptoms of hypertrophic cardiomyopathy:
9. Atrio-ventricular discordance with ventriculo-arterial discordance indicates:
10. Single papillary muscle in the left ventricle is associated with:
Answers
1. Atrial septal defect results in dilatation of the right cardiac chambers because of the right-side volume overload. Pulmonic valve stenosis results in right ventricular hypertrophy because of the pressure overload. Ventricular septal defect results in left ventricular volume overload (oh, don’t ask why). Transposition of the great vessels (D-TGA) needs to be repaired for survival, and will result in dilatation of the systemic ventricle (anatomic right) with the now abandoned Mustard repair. If D-TGA is repaired with the arterial switch procedure, the right ventricle will be unaffected. Anatomically corrected transposition of the great vessels (L-TGA) results in dilatation of the systemic (anatomic right) ventricle.
How do you confuse an echocardiographer? Show him two shovels and ask him to take his pick.
2. The longest one with the italics: E
3. Always pick C. You should Google E. D is like the Tooth Fairy, Santa, and a cardiac surgeon with a sense of humor (non-existent).
4. E. Snowman cardiac shadow: the head of snowman is the superior mediastinal shadow delineated by the SVC on the right, vertical vein on left side and left brachicephalic vein superiorly. Body of snowman is the heart. Snowstorm is brought to you courtesy of pulmonary congestion.
Scimitar (shamelessly self-promoted): http://rwjms1.umdnj.edu/shindler/scimitar.html
5. C. They usually do a good job closing the VSD. Thank God for small favors.