CHAPTER 10 Congenital Diaphragmatic Hernia and Eventration of the Diaphragm
Congenital Diaphragmatic Hernia
Step 1: Surgical Anatomy
Step 2: Preoperative Considerations
Diagnosis
Resuscitation
Step 3: Operative Steps
Anesthesia
Positioning
Incision
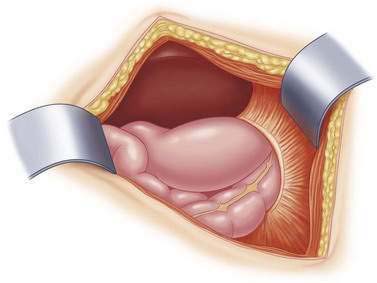
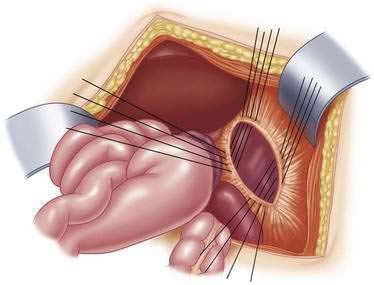
Hernia Reduction
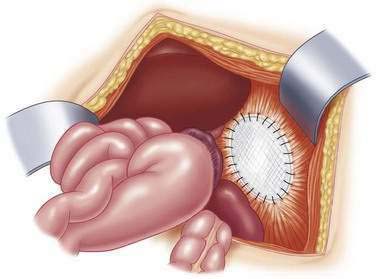
Repair of the Diaphragm
Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Thoracoscopic CDH Repair
Step 2: Preoperative Considerations
Step 3: Operative Steps
Positioning
Reduction of Viscera and Repair of Defect
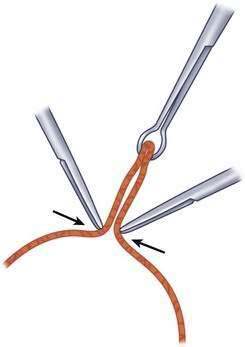
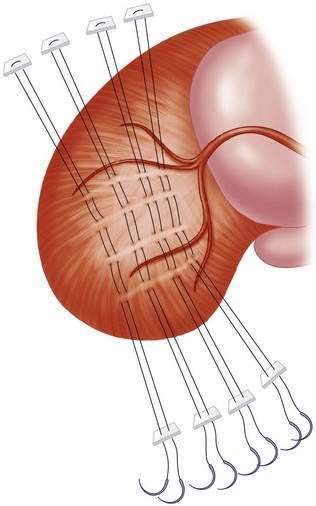
Optional Pericostal Sutures
Eventration of the Diaphragm
Step 1: Surgical Anatomy
Step 2: Preoperative Considerations
Diagnosis
 A right-sided eventration is suspected when the ipsilateral hemidiaphragm is greater than two rib levels higher than the left.
A right-sided eventration is suspected when the ipsilateral hemidiaphragm is greater than two rib levels higher than the left. A left sided eventration is entertained when the left hemidiaphragm is one rib level above the right diaphragm.
A left sided eventration is entertained when the left hemidiaphragm is one rib level above the right diaphragm.Associated Anomalies
Step 3: Operative Steps
Incision
Repair of the Eventration
Boloker J, Bateman DA, Wung JT, et al. Congenital diaphragmatic hernia in 120 infants treated consecutively with permissive hypercapnia/spontaneous respiration/elective repair. J Pediatr Surg. 2002;37:357-366.
Hines MH. Video-assisted diaphragm plication in children. Ann Thorac Surg. 2003;76:234-236.
Lally KP, Harting MT. Surgical management of neonates with congenital diaphragmatic hernia. Semin Pediatr Surg. 2007;16:109-114.
Lally KP, Lally PA, Van Meurs KP, et al. Treatment evolution in high-risk congenital diaphragmatic hernia: ten years’ experience with diaphragmatic agenesis. Ann Surg. 2006;244:505-513.
Stolar CJH, Dillon PW. Congenital Diaphragmatic Hernia and Eventration. In: Grosfeld JL, O’Neill JAJr, Fonkalsrud EW, Coran AG, editors. Pediatric Surgery. 6th ed. Philadelphia: Mosby Elsevier; 2006:931-954.
West SD, Wilson JM. Follow up of infants with congenital diaphragmatic hernia. Semin Perinatol. 2005;29:129-133.
Yang EY, Allmendinger N, Johnson SM, et al. Neonatal thoracoscopic repair of congenital diaphragmatic hernia: selection criteria for successful outcome. J Pediatr Surg. 2005;40:1369-1375.
Yazici M, Karaca I, Arikan A, et al. Congenital eventration of the diaphragm in children: 25 years’ experience in three pediatric surgery centers. Eur J Pediatr Surg. 2003;13:298-301.