2
Conduction and its problems
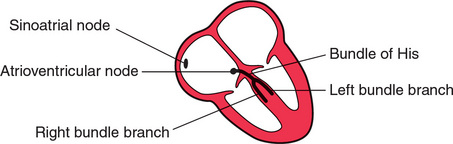
We have already seen that electrical depolarization normally begins in the sinoatrial (SA) node, and that a wave of depolarization spreads outwards through the atrial muscle to the atrioventricular (AV) node, and thence down the His bundle and its branches to the ventricles. The conduction of this wave front can be delayed or blocked at any point. However, conduction problems are simple to analyse, provided you keep the wiring diagram of the heart constantly in mind ( Fig. 2.1).
CONDUCTION PROBLEMS IN THE AV NODE AND HIS BUNDLE
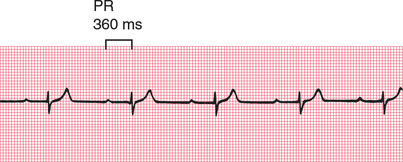
The time taken for the spread of depolarization from the SA node to the ventricular muscle is shown by the PR interval (see Ch. 1), and is not normally greater than 220 ms (six small squares).
FIRST DEGREE HEART BLOCK
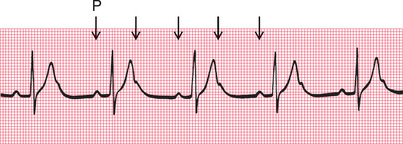
If each wave of depolarization that originates in the SA node is conducted to the ventricles, but there is delay somewhere along the conduction pathway, then the PR interval is prolonged. This is called ‘first degree heart block’ ( Fig. 2.2).
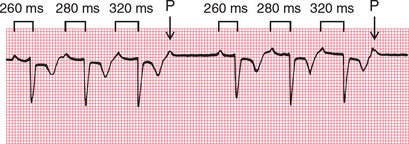
SECOND DEGREE HEART BLOCK
Sometimes excitation completely fails to pass through the AV node or the bundle of His. When this occurs intermittently, ‘second degree heart block’ is said to exist. There are three variations of this:
1. There may be progressive lengthening of the PR interval and then failure of conduction of an atrial beat, followed by a conducted beat with a shorter PR interval and then a repetition of this cycle. This is the ‘Wenckebach’ or ‘Mobitz type 1’ phenomenon ( Fig. 2.3).
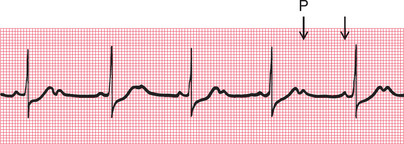
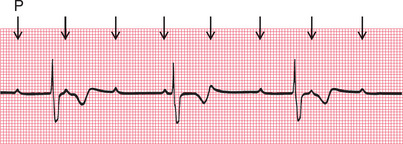
2. Most beats are conducted with a constant PR interval, but occasionally there is atrial depolarization without a subsequent ventricular depolarization. This is called the ‘Mobitz type 2’ phenomenon ( Fig. 2.4).
3. There may be alternate conducted and nonconducted atrial beats (or one conducted atrial beat and then two or three nonconducted beats), giving twice (or three or four times) as many P waves as QRS complexes. This is called ‘2:1’ (‘two to one’), ‘3:1’ (‘three to one’) or ‘4:1’ (‘four to one’) conduction ( Fig. 2.5).
It is important to remember that, as with any other rhythm, a P wave may only show itself as a distortion of a T wave ( Fig. 2.6).
The underlying causes of second degree heart block are the same as those of first degree block. The Wenckebach phenomenon is usually benign, but Mobitz type 2 block and 2:1, 3:1 or 4:1 block may herald ‘complete,’ or ‘third degree’, heart block.
THIRD DEGREE HEART BLOCK
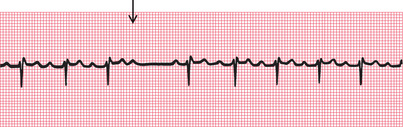
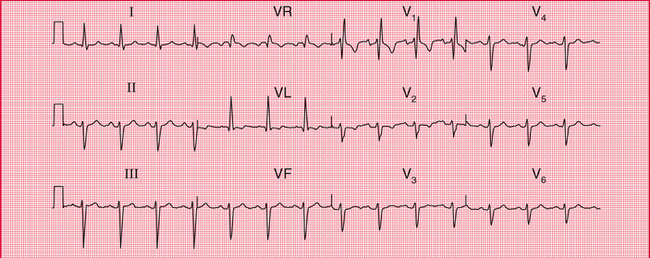
Complete heart block (third degree block) is said to occur when atrial contraction is normal but no beats are conducted to the ventricles ( Fig. 2.7). When this occurs the ventricles are excited by a slow ‘escape mechanism’ (see Ch. 3), from a depolarizing focus within the ventricular muscle.
Complete block is not always immediately obvious in a 12-lead ECG, where there may be only a few QRS complexes per lead (e.g. see Fig. 2.8). You have to look at the PR interval in all the leads to see that there is no consistency.
CONDUCTION PROBLEMS IN THE RIGHT AND LEFT BUNDLE BRANCHES – BUNDLE BRANCH BLOCK
If the depolarization wave reaches the interventricular septum normally, the interval between the beginning of the P wave and the first deflection in the QRS complex (the PR interval) will be normal. However, if there is abnormal conduction through either the right or left bundle branches (‘bundle branch block’) there will be a delay in the depolarization of part of the ventricular muscle. The extra time taken for depolarization of the whole of the ventricular muscle causes widening of the QRS complex.
A wide QRS complex can therefore indicate bundle branch block, but widening also occurs if depolarization begins within the ventricular muscle itself (see Ch. 3). However, remember that in sinus rhythm with bundle branch block, normal P waves are present with a constant PR interval. We shall see that this is not the case with rhythms beginning in the ventricles.
The mechanism underlying the ECG patterns of RBBB and LBBB can be worked out from first principles. Remember (see Ch. 1):
• The septum is normally depolarized from left to right.
• The left ventricle, having the greater muscle mass, exerts more influence on the ECG than does the right ventricle.
• Excitation spreading towards a lead causes an upward deflection within the ECG.
RIGHT BUNDLE BRANCH BLOCK
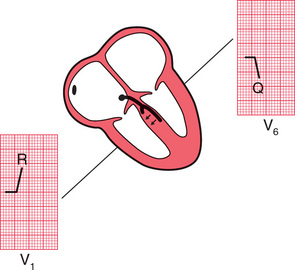
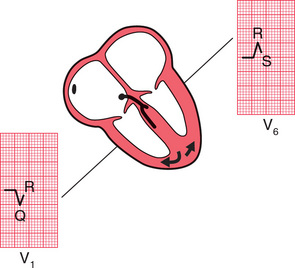
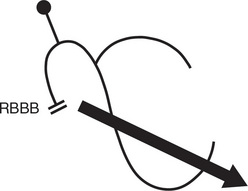
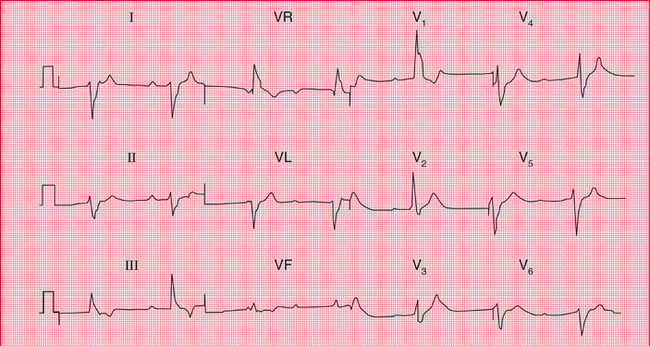
In RBBB, no conduction occurs down the right bundle branch but the septum is depolarized from the left side as usual, causing an R wave in a right ventricular lead (V1) and a small Q wave in a left ventricular lead (V6) ( Fig. 2.9).
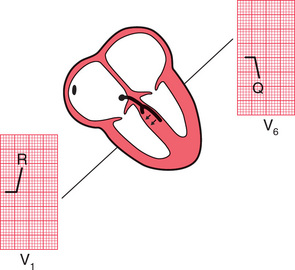
Excitation then spreads to the left ventricle, causing an S wave in lead and an R wave in lead V6 ( Fig. 2.10).
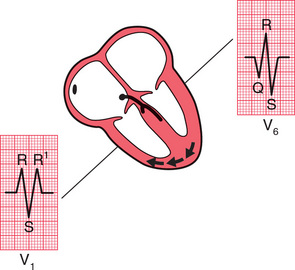
It takes longer than in a normal heart for excitation to reach the right ventricle because of the failure of the normal conducting pathway. The right ventricle therefore depolarizes after the left. This causes a second R wave (R1) in lead Vl5 and a wide and deep S wave, and consequently a wide QRS complex, in lead V6 ( Fig. 2.11).
LEFT BUNDLE BRANCH BLOCK
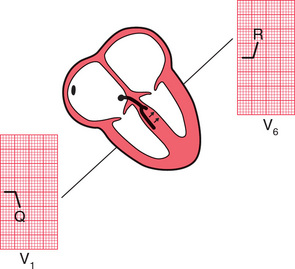
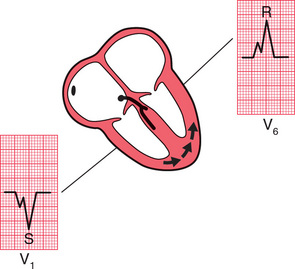
If conduction down the left bundle branch fails, the septum becomes depolarized from right to left, causing a small Q wave in lead V1, and an R wave in lead V6 ( Fig. 2.12).
The right ventricle is depolarized before the left, so despite the smaller muscle mass there is an R wave in lead V1 and an S wave (often appearing only as a notch) in lead V6 ( Fig. 2.13). Remember that any upward deflection, however small, is an R wave, and any downward deflection, however small, following an R wave is called an S wave.
Subsequent depolarization of the left ventricle causes an S wave in lead V1 and another R wave in lead V6 ( Fig. 2.14).
REMINDERS
BUNDLE BRANCH BLOCK
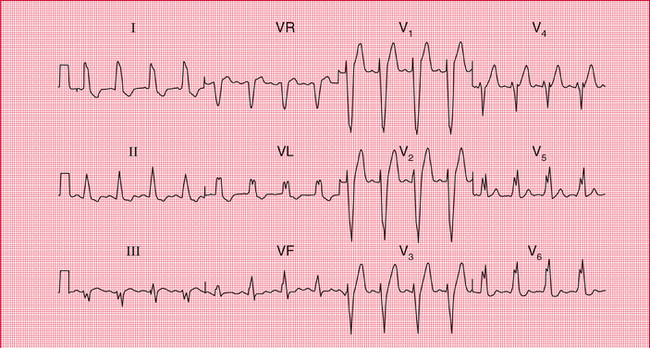
• RBBB is best seen in lead V1 where there is an RSR1 pattern ( Fig. 2.15).
• LBBB is best seen in lead V6, where there is a broad QRS complex with a notched top, which resembles the letter ‘M’ and is therefore known as an ‘M’ pattern ( Fig. 2.16). The complete picture, with a W’ pattern in lead V1, is often not fully developed.
CONDUCTION PROBLEMS IN THE DISTAL PARTS OF THE LEFT BUNDLE BRANCH
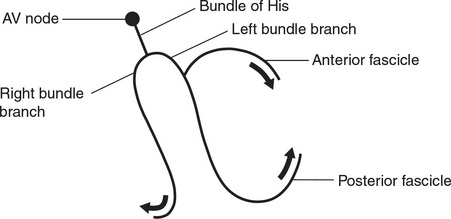
At this point it is worth considering in a little more detail the anatomy of the branches of the His bundle. The right bundle branch has no main divisions, but the left bundle branch has two – the anterior and posterior ‘fascicles’. The depolarization wave therefore spreads into the ventricles by three pathways ( Fig. 2.17).
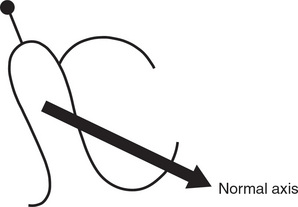
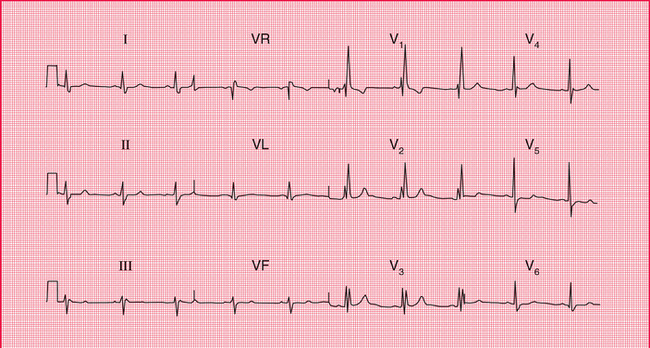
The cardiac axis (see Ch. 1) depends on the average direction of depolarization of the ventricles. Because the left ventricle contains more muscle than the right, it has more influence on the cardiac axis ( Fig. 2.18).
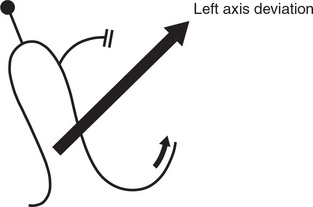
If the anterior fascicle of the left bundle branch fails to conduct, the left ventricle has to be depolarized through the posterior fascicle, and so the cardiac axis rotates upwards ( Fig. 2.19).
Left axis deviation is therefore due to left anterior fascicular block, or ‘left anterior hemiblock’ ( Fig. 2.20).
The posterior fascicle of the left bundle is only rarely selectively blocked, in ‘left posterior hemiblock’, but if this does occur the ECG shows right axis deviation.
When the right bundle branch is blocked, the cardiac axis usually remains normal, because there is normal depolarization of the left ventricle with its large muscle mass ( Fig. 2.21).
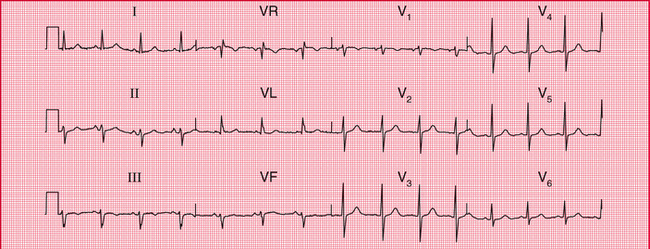
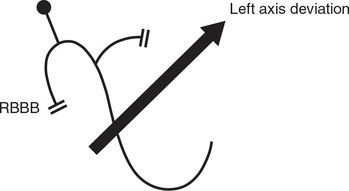
However, if both the right bundle branch and the left anterior fascicle are blocked, the ECG shows RBBB and left axis deviation ( Fig. 2.22). This is sometimes called ‘bifascicular block’, and this ECG pattern obviously indicates widespread damage to the conducting system ( Fig. 2.23).
WHAT TO DO
Always remember that it is the patient who should be treated, not the ECG. Relief of symptoms always comes first. However, some general points can be made about the action that might be taken if the ECG shows conduction abnormalities.
Left axis deviation and right bundle branch block
• Indicates severe conducting tissue disease.
• No specific treatment needed.
• Pacemaker required if the patient has symptoms suggestive of intermittent complete heart block.
REMINDERS
CONDUCTION AND ITS EFFECTS ON THE ECG
• Depolarization normally begins in the SA node, and spreads to the ventricles via the AV node, the His bundle, the right and left branches of the His bundle, and the anterior and posterior fascicles of the left bundle branch.
• A conduction abnormality can develop at any of these points.
• Conduction problems in the AV node and His bundle may be partial (first and second degree block) or complete (third degree block).
• If conduction is normal through the AV node, the His bundle and one of its branches, but is abnormal in the other branch, bundle branch block exists and the QRS complex is wide.
• The ECG pattern of RBBB and LBBB can be worked out if you remember that:
− the septum is depolarized first from left to right
− lead V1 looks at the right ventricle and lead V6 at the left ventricle
− when depolarization spreads towards an electrode the stylus moves upwards.
• If you can’t remember all this, remember that RBBB has an RSR1 pattern in lead V1 while LBBB has a letter ‘M’ pattern in lead V6.
• Block of the anterior division or fascicle of the left bundle branch causes left axis deviation.
 For more conduction problems, see pp. 85-95
For more conduction problems, see pp. 85-95
 For more on treatment of conduction problems with pacemakers, see pp. 187-206
For more on treatment of conduction problems with pacemakers, see pp. 187-206