8
Conclusions
Four Steps to Making the Most of the ECG
The theme of this book has been that the ECG is just one way of helping with the management of patients. The ECG is not an end in itself, and must always be seen in the context of the patient from whom it was recorded. To make the most of an ECG you need to think in four steps:
DESCRIPTION
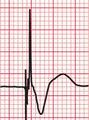
The QRS complexes need to be described in terms of their width and height, and also their shape: whether Q waves are present; whether there is more than one R wave in the QRS complex; and whether there are S waves in the leads where they would be expected. If there are Q waves, are they small and narrow, and are they only seen in the lateral leads, where they may be due to septal depolarization? If there are pathological Q waves, in which leads are they present and do they suggest a possible inferior or anterior myocardial infarction? The cardiac axis should be defined.
INTERPRETATION
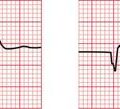
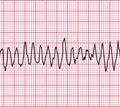
In a patient with breathlessness, right axis deviation, a dominant R wave in lead V1 or T wave inversion in leads V1− V3 may indicate multiple pulmonary emboli or idiopathic pulmonary hypertension. A deep S wave in lead V6 may be due to chronic lung disease or to a pulmonary embolus. In patients complaining of attacks of dizziness, a finding such as first degree block, of little significance in a healthy subject, might indicate transient episodes of higher degrees of block causing a symptomatic bradycardia. A prolonged QT interval might point to episodes of torsade de pointes ventricular tachycardia.
TREATMENT
Without an understanding of the ECG, devices such as pacemakers and implanted cardioverter defibrillators (ICDs) could not have been invented. These devices, and the techniques that use them, such as dual chamber pacing and cardiac resynchronization therapy, are the province of the specialist. But as the devices and techniques become increasingly prevalent, they will be encountered more and more by general practitioners and specialists in non-cardiac disciplines. For example, patients with these devices tend to be elderly, and it is the elderly who most frequently experience multiple medical problems – so non-cardiac specialists are bound to come across patients who have problems, but who also have a modern electrical device that is working perfectly normally.