15
Concepts of Joint Mobilization
Robert C. Manske and Justin Rohrberg
1. Discuss the general and applied concepts of peripheral joint mobilization.
2. Define terms and principles of peripheral joint mobilization.
3. Define and describe the convex–concave rule.
4. Define the five grades of mobilization.
5. Identify and describe terms of joint end-feel.
6. Define and describe capsular and noncapsular patterns.
7. Identify common indications and contraindications for mobilization.
8. Discuss the clinical basics and applications of peripheral joint mobilization.
9. Identify and discuss the role of the physical therapist assistant in assisting the physical therapist with the delivery of peripheral joint mobilization.
FUNDAMENTAL PRINCIPLES OF MOBILIZATION
A healthy joint is one that moves without limitation. In synovial joints, movement stimulates biological activity by moving synovial fluid to areas of avascular articular cartilage. Additionally, strength and resiliency of capsular tissue and periarticular tissue is maintained via joint movement. Immobilization causes a host of negative consequences such as fatty infiltration, articular adhesions, and physiologic changes to the strength and tolerance of ligaments, tendons, and capsular tissue. The term mobilization refers to an attempt to restore joint motion or mobility, or decrease pain associated with joint structures using manual, passive accessory-joint movement.4,21
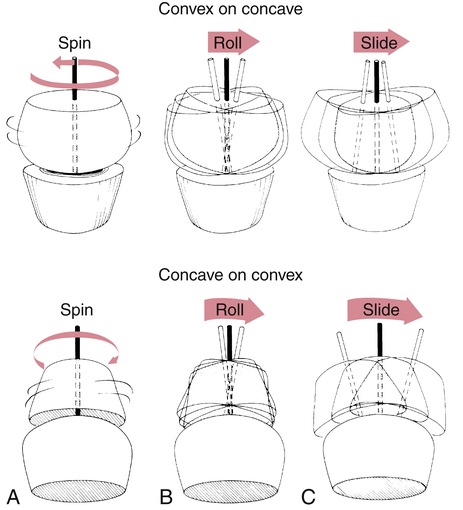
Joint mobilizations are passive, skilled manual therapy techniques applied to joints and related soft tissues at varying speeds and amplitudes using physiologic or accessory motions for therapeutic purposes.1 Range of motion (ROM) involves physiologic movements which are active/passive motions at a given joint through one of the traditional cardinal planes of flexion, extension, abduction, adduction, or internal and external rotation. Physiologic movements are sometimes called osteokinematic, classical, or traditional movements because they are movements of the actual bones of a given joint system. These motions can be visualized by the naked eye and are commonly measured by goniometric assessment. Osteokinematic motions occur in the cardinal planes of movement such as frontal, sagittal, and transverse. Hip, knee, and shoulder flexion movements are examples of osteokinematic movements. These are all movements that can occur under volitional control. Arthrokinematic movements are those that occur at the bone ends, without regard to the movement. These movements are not under volitional control. These types of movements are known as accessory movements involving motions specific to articulating joint surfaces.4,21 These accessory joint motions are referred to as glide or slide, spin, and roll.4,14 Because these are passive movements at the actual joint level, they are sometimes referred to as arthrokinematic motions. Accessory and physiologic joint motions occur together during active ROM. If full accessory motion does not occur, there will be a limitation in normal physiological cardinal plane movements. However, accessory joint motion cannot be selectively recruited, meaning that a patient cannot selectively perform joint roll, glide, or spin independently on their own.4 The application of accessory joint motion is defined as “joint play” or “motion that occurs within the joint as a response to an outside force but not as a result of voluntary movement.”4
JOINT CONGRUENCY AND POSITION
The concept of joint congruency and the terms close-packed and loose-packed, referring to joint position, are pertinent to the discussion of various grades of mobilization. Congruence refers to articular position with regard to concave and convex joint surfaces. A joint is congruent when both articulating surfaces are in contact throughout the total surface area of the joint.4,14 However, the study of arthrokinematics (joint movement) states that joints are rarely in total congruence. As joints move, the accessory motions of glide or slide, spin, and roll alter total joint congruence.
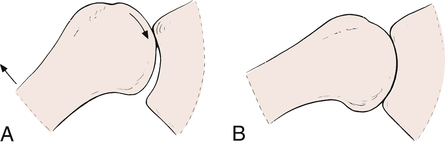
MacConaill and Basmajian14 have described close-packed positions as the most congruent positions of a joint,4,14 where the joint articular surfaces are aligned and the capsule and ligaments are taut and joint volume is minimal (Fig. 15-1). Generally, a close-packed position is used for testing the integrity and stability of ligaments and capsular structures. However, the close-packed position described by MacConaill and Basmajian14 is not used for mobilization techniques. The close-packed position is one of stability. When the elbow and knee are fully extended, the ligaments and joint capsule are taut, allowing no freedom of movement. Therefore the knee and elbow in extension serve as two excellent examples of joints in the close-packed position.
Any joint position other than the close-packed position is a loose-packed position. The position in which the joint capsule and ligaments are most relaxed, loose, and allow the maximum amount of joint play is referred to as the joint’s resting position.4 When the knee joint is flexed to 30°, the intracapsular space is increased and supporting ligaments become more relaxed. The loose-packed position is ideal for applying joint mobilization techniques, but painful, stiff, and dysfunctional joints are rarely in ideal resting positions for the application of joint mobilization. Table 15-1 lists resting and close-packed positions of major joints in the human body.16 If a joint has a limitation of arthrokinematic movement in which the close-packed position cannot be achieved, ground reaction forces and gravitational forces are not distributed through the joint in an optimal manner, thus additional stress and work has to be taken up by the periarticular muscles. If this dysfunctional movement pattern continues, a condition of muscle overuse can ensue.
Table 15-1
Resting (Loose) and Closed-Packed Position of Joints
| Joint | Resting Position | Closed-Packed Position |
| Facet (spine) | Midway between flexion and extension | Extension |
| Temporomandibular | Mouth slightly open (freeway space) | Clenched teeth |
| Glenohumeral | 55° abduction, 30° horizontal adduction | Abduction and lateral rotation |
| Acromioclavicular | Arm resting by side in normal physiologic position | Arm abducted to 90° |
| Sternoclavicular | Arm resting by side in normal physiologic position | Maximum shoulder elevation |
| Ulnohumeral (elbow) | 70° flexion, 10° supination | Extension |
| Radiohumeral | Full extension, full supination | Elbow flexed 90°, forearm supinated 5° |
| Proximal radioulnar | 70° flexion, 35° supination | 5° supination |
| Distal radioulnar | 10° supination | 5° supination |
| Radiocarpal (wrist) | Neutral with slight ulnar deviation | Extension with radial deviation |
| Carpometacarpal | Midway between abduction-adduction and flexion-extension | |
| Metacarpophalangeal (all) | Slight flexion | |
| Metacarpophalangeal (fingers) | Full flexion | |
| Metacarpophalangeal (thumb) | Full opposition | |
| Interphalangeal | Slight flexion | Full extension |
| Hip | 30° flexion, 30° abduction, slight lateral rotation | Full extension, medial rotation |
| Knee | 25° flexion | Full extension, lateral rotation of tibia |
| Talocrural (ankle) | 10° plantarflexion, midway between maximum inversion and eversion | Maximum dorsiflexion |
| Subtalar | Midway between extremes of range of motion | Supination |
| Midtarsal | Midway between extremes of range of motion | Supination |
| Tarsometatarsal | Midway between extremes of range of motion | Supination |
| Metatarsophalangeal | Neutral | Full extension |
| Interphalangeal | Slight flexion | Full extension |
From Magee DJ: Orthopedic physical assessment, ed 5, St Louis, 2008, Saunders.
CONVEX–CONCAVE RULE
Anatomically, all articular surfaces are either convex or concave,4,21 although the surfaces of some joints are not overtly of either shape. In these cases, fibrocartilage enhances and modifies the contour of the joint surfaces. On the convex joint surface, more cartilage is found at the center of the surface; on a concave joint surface, more cartilage is found at the periphery.4
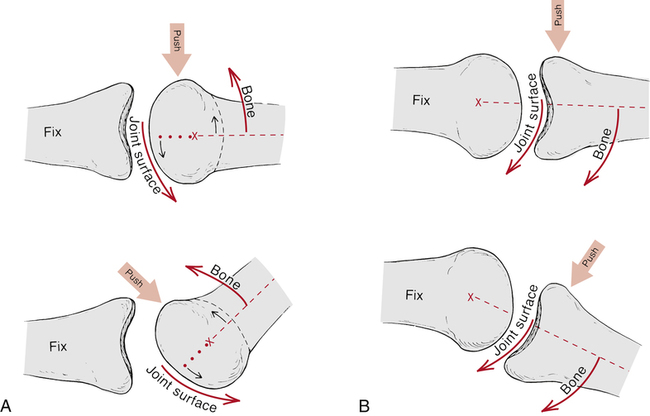
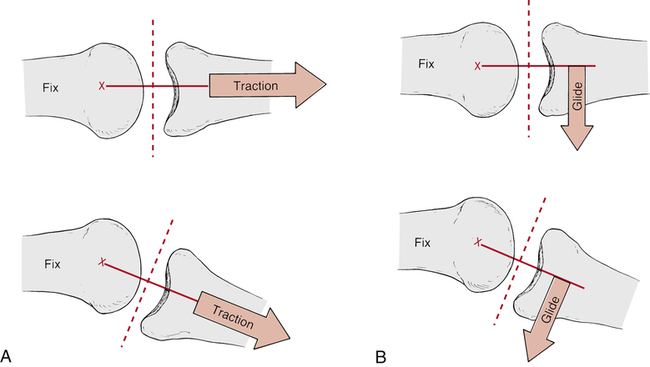
The convex–concave rule specifically states, “When the concave surface is stationary and the convex surface is moving, the gliding movement in the joint occurs in a direction opposite to the bone movement.”4 Conversely, if the convex surface is fixed while the concave surface is mobile, the gliding motion occurs in the same direction as the bone movement.4 This occurs because the convex bone surface always maintains an axis of rotation during joint motion (Fig. 15-2). The concept of accessory joint motions (glide or slide, spin, and roll), as they apply to joint congruency and the convex–concave rule, is clearly illustrated by MacConaill’s classification of accessory movements (Fig. 15-3).
MOBILIZATION GRADES
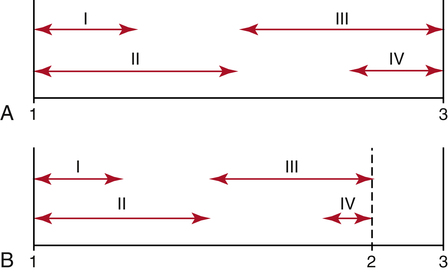
Maitland17 describes five grades of physiologic and accessory joint motions used in mobilization (Fig. 15-4). The terms velocity, oscillation, and amplitude of movement describe the degree of force and rate of motion used during any of the grades of mobilization, as follows:
 Grade I mobilization: A small oscillation or small amplitude joint motion that occurs only at the beginning of the available ROM.
Grade I mobilization: A small oscillation or small amplitude joint motion that occurs only at the beginning of the available ROM.
 Grade II mobilization: A larger amplitude motion occurring from the beginning of the ROM to near midrange.
Grade II mobilization: A larger amplitude motion occurring from the beginning of the ROM to near midrange.
 Grade III mobilization: A large amplitude motion that occurs from midrange of motion to the end of the available range.
Grade III mobilization: A large amplitude motion that occurs from midrange of motion to the end of the available range.
 Grade IV mobilization: A small oscillation or amplitude of motion that occurs at the very end range of the available joint motion.
Grade IV mobilization: A small oscillation or amplitude of motion that occurs at the very end range of the available joint motion.
 Grade V mobilization: “A high velocity thrust of small amplitude at the end of the available ROM.”4 This grade is not applied to mobilization techniques used by PTAs and is not addressed in this text.
Grade V mobilization: “A high velocity thrust of small amplitude at the end of the available ROM.”4 This grade is not applied to mobilization techniques used by PTAs and is not addressed in this text.
In general terms, a grade I or II small amplitude oscillation is used to treat pain or when joint motion produces pain.4,21 Therefore mobilization in grades III and IV are used to treat joint restrictions.4,21
Translational movements during joint mobilization techniques can be performed in one of two planes. Joint mobilizations can be performed perpendicular or parallel to the treatment plane. The treatment plane is described as a line running perpendicular to, or at a right angle to, a line running from the axis of joint rotation in the convex surface to the center of the concave articular surface.12 A translational joint mobilization technique (glide) is one in which the articulating surface glides along a line parallel to the treatment plane.
Traction also is used as a manual therapy technique either by itself or along with various mobilization techniques (Fig. 15-5). A traction technique is a joint mobilization technique that translates one articular surface in a perpendicular direction away from the treatment plane. Traction can be classified in grades or stages.12,17 Generally, grade I or stage I traction is used for relief of pain and to minimize compressive joint forces during mobilization. The term piccolo traction describes a stage I traction technique. The force used to deliver grade I traction is not enough to actually separate the joint surfaces, but rather only neutralizes joint pressure.4
JOINT END-FEEL
There are various qualities of joint tightness or “play” during the application of passive joint movements. Three types of end-feel have been defined in normal, nonpathologic joints.7,16 Bone to bone end-feel refers to a sudden, hard, nonyielding sensation felt at the end ROM. Generally, the end-feel is not painful. Terminal elbow extension in which the olecranon process contacts the olecranon fossa provides an example of a sudden bone-to-bone end-feel.
Another normal end-feel is soft-tissue approximation. This type of joint end-feel is characterized by a “yielding compression” typically encountered with knee or elbow flexion.16 The end-feel that occurs with soft tissue approximation results from muscular tissue compression during joint flexion. The hamstring and calf muscles buttress and compress against each other during knee flexion, delivering a soft-tissue approximation end-feel.
The third normal joint end-feel is described as a hard or springy-tissue stretch. The characteristic feature of this end-feel is “elastic resistance” or “rising tension.”16 This type of end-feel is the most common normal feel at the end range of joints. Terminal knee extension and wrist flexion provide a springy stretch that defines tissue stretch.
The PTA must experience normal joint end-feel and be able to accurately identify distinguishing characteristics between bone-to-bone end-feel, soft-tissue approximation, and tissue stretch.7 The PTA performing mobilization will undoubtedly encounter abnormal joint end-feel, and its precise identification requires considerable didactic and hands-on experience.7
The first type of abnormal end-feel is muscle spasm. The major component is pain accompanied by a sudden halt of movement that prevents full ROM.4,7,16
Another abnormal end-feel is described as loose end-feel.4 Its primary feature is joint hypermobility, with no resistance typically felt at the end ROM that signifies extraordinary joint looseness.
A capsular end-feel16 is analogous to a normal tissue stretch, but the elastic resistance is encountered before the normal ROM. This end-feel is related to a capsular restriction.16
Table 15-2 lists various normal and pathologic end-feels and examples of each.2
Table 15-2
Normal and Pathologic End-Feels
| End-Feel | Description and Example | |
| Normal | Capsular | Firm, forcing the shoulder into full external rotation |
| Bony | Abrupt, moving the elbow into full extension | |
| Soft-tissue approximation | Soft; flexing the normal knee or elbow | |
| Muscular | Rubbery; tension of tight hamstrings | |
| Pathologic | Adhesions and scarring | Sudden; sharp arrest in one direction |
| Muscle spasm | Rebound; usually accompanies pain felt at the end of restriction | |
| Loose | Ligamentous laxity; a hypermobile joint | |
| Boggy | Soft, mushy; joint effusion | |
| Internal derangement | Springy; mechanical block such as a torn meniscus | |
| Empty | No resistance to motion | |
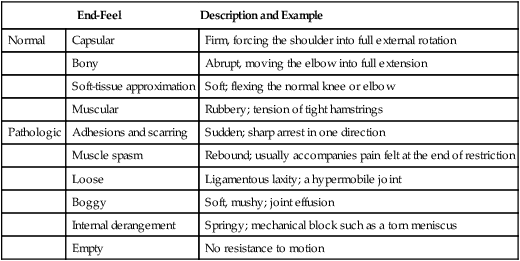
From Andrews J, Harrelson G, Wilk K: Physical rehabilitation of the injured athlete, ed 3, St Louis, 2004, Saunders; source material from Cyriax JH: Textbook of orthopedic medicine, vol 1, ed 6. Baltimore, 1975, Williams & Wilkins.
CAPSULAR AND NONCAPSULAR PATTERNS
The PTA must be aware that certain limitations of motion can be caused by lesions specific to the capsule or synovial tissues of a joint. All joints controlled by muscle activity possess a characteristic “capsular pattern of proportional limitation.”16 Each joint has its own capsular pattern, which is generally universal among all. For example, in the shoulder joint, the capsular pattern “involves external rotation as the most limited movement, abduction as less limited, internal rotation still less limited, and flexion as the least limited movement.”4,7 Any “characteristic pattern of limitation” is called a capsular pattern.
If a lesion causes a restriction of movement that does not correspond to a characteristic, predetermined capsular pattern, it is called a noncapsular pattern.4,16 Cyriax7 has identified three possible causes of noncapsular pattern restrictions:
1. Ligamentous adhesions: Frequently cause pain and limitation of motion. A noncapsular pattern exists when injury to the capsule or accessory ligaments causes a restriction in one direction, although other motions remain unaffected and pain free.
2. Internal derangements: A displaced or loose cartilaginous or bony fragment within the joint. The limitation of movement will depend on where the fragment is located and how large it is. If the medial meniscus becomes wedged in the joint, knee extension is affected although flexion remains normal.
3. Extraarticular lesions: Adhesions resulting from injury outside the joint. Muscular adhesions or acutely inflamed structures are examples. Causes of this can be bursitis, muscle strains, neural tissue irritation, and so on.
Table 15-3 lists joint restrictions from noncapsular patterns.2
Table 15-3
Joint Restrictions from Noncapsular Pattern
| Type | Description |
| Ligament adhesions | These occur when adhesions form around a ligament after an injury and may cause pain or a restriction of mobility. Some movements will be painful, some are slightly limited, and some are pain free. |
| Internal derangement | Restriction in joint mobility is the result of a loose fragment within the joint. The onset is sudden, pain is localized, and movements that engage against the block are limited, whereas all others are free. |
| Extraarticular limitation | Loss in joint mobility results from adhesions in structures outside the joint. Movements that stress the adhesions will be limited and painful. |
From Andrews J, Harrelson G, Wilk K: Physical rehabilitation of the injured athlete, ed 3, St Louis, 2004, Saunders.
INDICATIONS AND CONTRAINDICATIONS FOR MOBILIZATION
Patient safety should always be considered when applying joint mobilization or manipulation techniques. Cautions or contraindications for joint mobilization and manipulation are listed in Table 15-4 and Box 15-1.15 Extreme caution must be employed before applying mobilization techniques in the early stages after trauma or surgery or during times of immobilization. Although pain is an indication for the use of mobilization, care must be taken to avoid retarding or impairing the sequence of tissue healing during the acute inflammatory phase.
Table 15-4
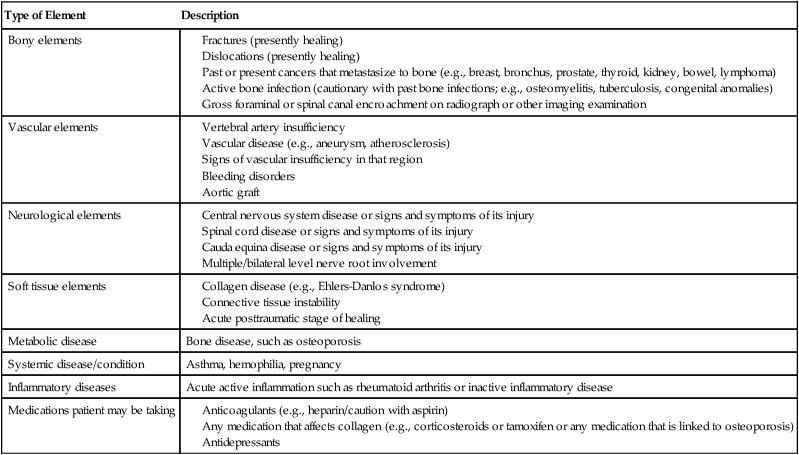
From Maffey LL: Arthrokinematics and mobilization of musculoskeletal tissue: the principles. In Magee DJ, Zachazewski JE, Quillen WS, editors: Scientific foundations and principles of practice in musculoskeletal rehabilitation, St Louis, 2007, Saunders.
Pain and joint restrictions are rarely separated completely. In many instances of severe joint limitations there may be only mild complaints of pain. Conversely, there may be little or no joint restriction but significant pain. Naturally there are varying degrees of pain and joint limitations occurring as either major or minor components. Therefore pain is a relative indication for joint mobilization, depending on which stage of tissue healing is present. If an injury is acute or a patient is recovering immediately after a surgical procedure, mobilization may not be indicated because it is best not to disturb the immature scar. Healing that proceeds in an organized fashion encourages mature collagen formation. When injured tissues have progressed from the acute, intense inflammatory phase to fibroplasia and scar maturation, mobilization is warranted to stress and remodel the scar.21
There are a few relative and absolute contraindications to the application of joint mobilization. Extreme caution is needed when considering mobilization in cases of osteoporosis, rheumatoid arthritis, joint hypermobility, and the presence of neurologic symptoms; all are therefore considered relative contraindications.4,21 In cases of spinal mobilization, pregnancy and spondylolisthesis are relative contraindications. Some absolute contraindications include bone diseases of the area treated, malignancy of the area treated, acute inflammatory and infectious arthritis, central nervous system (CNS) disorders, and vascular disorders of the vertebral artery.4,21
CLINICAL APPLICATION OF JOINT MOBILIZATION
Safe and effective joint mobilization requires the patient to be placed in a very comfortable position and the specific joint to be mobilized to be placed in a maximal resting or loose-packed position.14 Before mobilization is applied, patient compliance and relaxation can be facilitated by the judicious use of moist heat, ultrasound, transcutaneous electrical nerve stimulation (TENS), electrical muscle stimulation, ice, exercise, and the timely use of any physician-prescribed analgesics or muscle relaxant medications. If pain is the predominant feature of the joint to be mobilized, grade I and II mobilization can be employed safely.
Oscillations help modulate or minimize pain when using grade I and II mobilization. Manually applied joint oscillations occur at a rate of 1 to 3 per second, or 60 to 180 per minute.4,17 Typically, a mobilization grade technique is applied for 20 to 60 seconds only four or five times. This is recommended for the treatment of painful conditions on a daily basis or until pain is reduced. These smaller amplitude mobilization techniques are used to stimulate mechanoreceptors within the joint that can limit pain perception transmission at the spinal cord or brainstem level through a hypoalgesic response mediated by the noradrenergic descending pain pathways from the periaqueductal gray area.22
A program of mobilization is carried out two to three times per week for the treatment of joint restrictions.4 Piccolo or stage I traction can be used simultaneously with grade I or II mobilization or by itself to reduce pain and neutralize joint pressure. When the limitation of joint motion is greater than the complaints of pain, grade III and IV mobilization can be used to help stretch the capsule and soft tissues around the joint.
The pathologic condition of the joint to be mobilized must be thoroughly understood before applying any mobilization technique. For example, it is critical to avoid stressing the anterior capsule of the shoulder after an anterior dislocation, although mobilization to improve shoulder abduction may be warranted.21
MOBILIZATION EVIDENCE
There are mixed reviews in the ankle. Lin and colleagues13 recently reported that incorporation of large amplitude grade III anterior-posterior glides to the talus for 4 weeks did not enhance their outcomes at 24 weeks following ankle fractures. This is in direct contradiction to Green and coworkers8 who used an experimental group given anteroposterior joint mobilizations to the talus following an acute ankle sprain and a control group that was treated with rest, ice, compression, and elevation (RICE). Following the intervention period the experimental group required fewer treatments, had greater improvements in ROM at the ankle, and greater increases in stride speed, indicating that the addition of joint mobilizations had a positive impact on outcomes.
In the hip, Hoeksma and associates10 proved in a single-blind, RCT of 109 patients with osteoarthritic hips that manual therapy resulted in 81% success rates for the experimental group as compared with only 50% in the control group. The experimental group demonstrated better outcomes in regard to pain, stiffness, hip function, and ROM following 5 weeks (9 sessions) of manual therapy treatments of hip joint distraction followed by a hip traction manipulation. These beneficial changes remained even after 29 weeks.
In the shoulder, Senbursa and colleagues19 used a RCT to compare effectiveness of two treatments for shoulder impingement—soft tissue and joint mobilization or independent exercise program. Thirty patients with impingement were randomized into one of the treatment approaches and followed for 3 months. The manual therapy group received a prescription of 12 sessions of joint mobilization. The experimental group demonstrated significant decreases in pain and increases in ROM. Conroy and Hayes6 examined the usefulness of joint mobilizations on 14 patients with impingement syndrome. Random assignment was to an exercise program alone or an exercise program with joint mobilizations. The results were mixed, with the mobilization group demonstrating less 24-hour pain, and less pain with a subacromial compression test, but no differences in ROM and function.
Bang and Deyle3 assessed the comparison of supervised exercise versus supervised exercise combined with manual therapy to the upper quarter in those with impingement syndrome. The manual therapy approach they used consisted mainly of grade I to V oscillatory caudal glides of the glenohumeral joint in varying degrees of flexion and abduction. Bang and Deyle3 found significant improvement in pain reduction, function, and strength in those that received manual therapy in addition to supervised exercises. More recently, Manske and colleagues18 used an RCT of stretching versus stretching plus posterior shoulder capsular mobilizations to assess for efficacy in treating a tight posterior shoulder. The main outcome measure was internal rotation motion loss. Using 39 randomly assigned subjects with at least a 10° loss of internal rotation, it was found that the addition of posterior shoulder joint mobilization to a stretching program resulted in trends towards increased motion.
A Cochrane review performed by Gross and colleagues9 assessed mobilization and manipulation in patients with mechanical neck disorders. Outcomes were based on pain relief, functional improvement, or overall disability improvement. Studies including single session and multiple session manipulative therapy. Some in the presence of other treatment modalities showed little to no benefit for patients with acute, subacute, and chronic neck disorders. Mobilization alone was found to have similar results based on four randomized controlled trials in which mobilization was tested against cold pack, TENS, and ultrasound, among others. Mobilization and manipulation combined in a treatment approach also found little evidence to support their use for pain relief and improvement in function. Mobilization and manipulation with the addition of exercise was found to have positive results for the three outcome criteria. Though this is encouraging for those patients suffering with acute to chronic pain in the cervical spine, the authors also noted studies that compared manipulation plus exercise to exercise alone with little difference noted between these groups.
A review of literature done by Hurwitz and associates11 looked at studies examining the use of mobilization and manipulation in the management of neck pain and headaches. Neck pain was broken down into acute, and subacute or chronic neck pain. In the studies reviewed, the authors found that mobilization provided some statistically significant decreases in pain when compared with other treatment options. Manipulation of the cervical spine in patients experiencing subacute and chronic neck pain as well as tension-induced headaches showed subjective improvements compared with other therapies, however; the authors also noted the risks involved with cervical manipulation. These risks included paralysis and even death, with rates of injury occurring in 5 to 10 per 10 million manipulations.
In a study investigating the safety of mobilization to the thoracic spine, Sran and coworkers20 used 12 cadavers to determine the in vitro effects of spinal mobilization to the sixth thoracic vertebra. Loading of the spinous process of T6 was performed using mechanical compression to the point of failure. The average amount of force to failure in the cadaver models was 479 ± 162 newtons (N). These results varied significantly when compared to the in vivo effects of mobilization, where two physiotherapists applied an average load of 145 ± 38 N. The amount of force then applied in this study showed that posterior to anterior mobilization when applied with care has a fairly significant margin of error before fracture occurs. The authors summarized the findings to be clinically relevant in cases where the patient needing mobilization, at least in the thoracic spine, may have bone density issues leading to use of decreased force of mobilization or mobilization being contraindicated.
Management of low back pain is difficult and a very common problem in the patient population of the PT or PTA. The use of manipulation or mobilization to address the dysfunction associated with the low back is becoming increasingly popular. A systematic review of literature provided by Bronfort and colleagues5 showed that manipulation and mobilization of the spine did have some evidence to support its use in the management of acute and chronic low back pain. In acute episodes the authors were able to conclude manipulation was better suited to relieve pain than other treatment techniques, including mobilization and diathermy. For chronic low back pain the authors were able to conclude that manipulation with the addition of strengthening exercises had evidence to support its use in the reduction of pain and disability.
GLOSSARY
Arthrokinematics Study of motion within the joints. Description of joint typography.
Compression Occurs when two forces or loads are applied toward each other.
Manipulation Passive intervention motion of high velocity at end ranges of available joint motion.
Tension Occurs when two forces are applied in opposite directions.