Chapter 23 Computer Assistive Devices and Environmental Controls
Defining Assistive Technology
The term assistive technology is fairly new, although history records the use of tools to enable people with disabilities to walk, eat, and see as far back as the sixth or seventh century BC.14,17 Public Law 100-40725 defines AT as “any item, piece of equipment or product system whether acquired commercially off the shelf, modified, or customized that is used to increase or improve functional capabilities of individuals with disabilities.” This definition also includes a second component defining AT services as “any service that directly assists an individual with a disability in the selection, acquisition or use of an AT device.” Public Law 100-407 specifies the following:
Since 1988, this definition has also been used in other federal legislation authorizing services or supports for persons with disabilities. The Individuals with Disabilities Education Act3 (IDEA) and Reauthorization of the Rehabilitation Act24 are both examples of legislation that further codifies Public Law 100-407.
History, Legislation, and Utilization of Assistive Technology
Education: The Individuals with Disabilities Education Act
IDEA originated in 1997 and was reauthorized most recently as Public Law 108-446 by the 108th Congress. IDEA strengthens academic expectations and accountability for the nation’s 5.8 million children with disabilities. One important impact of IDEA legislation is that it specifies that AT devices and services be provided to children from birth to 21 years of age to facilitate education in a regular classroom if such devices and services are required as part of the student’s special education, related services, or supplementary aids and services (Code of Federal Regulations, Title 34, Sections 300.308) (Box 23-1). For students with disabilities, AT supports their acquisition of a free and appropriate public education. All individualized education plans developed for children needing special education services must indicate that AT has been considered as a way “to provide meaningful access to the general curriculum.”27 AT devices and services included as a component of an individualized education plan must also be provided at no cost to the student or parents. The school, however, can use other public and private funding sources that are available to fund the AT (34 CFR).
BOX 23-1 Summary of the Individuals with Disabilities Education Act Assistive Technology Requirements
Part C of IDEA also includes children before they start school. It covers the needs of children as soon as their developmental differences are noted. It intends that infants and toddlers receive services in the home or in other places, such as preschool settings, where possible. The services provided for these children are described in individualized family service plans. Individualized family service plans include parents, extended family, and early childhood interventionists and other related services personnel in planning and identifying goals and necessary services. IDEA also recognizes that coordination is needed to help families and children with the transition from infant and toddler programs to preschool programs. As a result, students with disabilities are being educated in preschool settings along with typically developing children in an effort to help all children reach the same developmental milestones.
The Americans with Disabilities Act and the Reauthorization of the Rehabilitation Act
The American Rehabilitation Act with Disabilities Act (ADA) was originally passed in 1990, and clarified the civil rights of persons with disabilities and specified equal access to public places, employment, transportation, and telecommunications. The ADA built on the foundation of the Rehabilitation Act of 1973 (updated in 2003 as the Reauthorization of the Rehabilitation Act) in recognizing the role of employment in enabling individuals with disabilities to become economically self-sufficient and integrated into communities. The ADA was amended in 2008, and these amendments became effective January 1, 2009. The amended ADA retains the original Act’s basic definition of “disability” as an impairment that substantially limits one or more major life activities, a record of such an impairment, or being regarded as having such an impairment.38,39 However, it changes the way that these statutory terms should be interpreted in several ways. Most significantly, the amended Act does the following:
Vocational rehabilitation services are often the key to enabling employment for adults with disabilities. The Rehabilitation Act mandates that AT devices and services should be considered and provided as a means to acquire vocational training, as well as to enter into and maintain employment. It also requires that AT be considered during the development and implementation of the Individualized Written Rehabilitation Plan, the document that guides a person’s vocational rehabilitation process. For example, if an individual has limited sight and needs to fill out paperwork to determine eligibility for vocational rehabilitation services, assistive devices to facilitate reading must be provided at that time. In recent years the Offices of Vocational Rehabilitation have become an important source of funding for AT devices and services to support employment for adults with disabilities.37
Assistive Technology and the International Classification of Functioning
The term disability is not always precise and quantifiable. The concept of disability is not even agreed on by persons who self-identify as having a disability, by professionals who study disability, or by the general public.23 This lack of agreement creates an obstacle to the study of disability and to the fair and effective administration of programs and policies intended for people with disabilities.4–818 With this issue in mind, the World Health Organization (WHO) developed a global common health language, one that includes physical, mental, and social well-being. The International Classification of Impairment, Disabilities, and Handicaps was first published by the WHO in 1980 as a tool for classification of the “consequences of disease.” The newest version, International Classification of Functioning, Disability and Health (ICF), moves away from a “consequence of disease” classification (1980 version) to a more positive “components of health” classification. This latest version provides a common framework and language for the description of health and health-related domains and uses the following language:
The ICF and its language help professionals define the need for health care and related services, such as the provision of AT. It recognizes that physical, mental, social, economic, or environmental interventions can improve lives and levels of functioning for persons with diseases. These might include medical, rehabilitation, psychosocial, or other person-based interventions.41 It also characterizes physical, mental, social, economic or environmental interventions that will improve lives and levels of functioning. Because AT has the potential to improve daily activities and participation in social and physical environments and thus improve the quality of life of individuals with disabilities, it clearly fits within the ICF. The WHO common health language is used throughout this chapter to discuss the potential impact of appropriate AT.
Overview of Assistive Technology Devices
The Human-Technology Interface
Individuals with impairments that affect their interaction with items in their environment need special consideration in the design, function, or placement of the devices they want or need to use. It is essential for many individuals to first be seated or positioned by using orthotic or ergonomic seating and positioning interventions, so they can optimally use their residual abilities17 (see Chapter 17).
Indirect Selection
Switches come in many styles and are selected based on the body part that will be activating them (e.g., elbow or chin) and the task or setting for using them (e.g., watching television in bed or using a communication device while eating). A switch can be as simple as a “wobble” switch that is activated by a gross motor movement such as hitting the switch with the head (Figure 23-1), hand, arm, leg, or knee. Other switches are activated by tongue touch, by sipping and puffing on a straw, or through very fine movements such as an eye blink or a single muscle twitch. Regardless, switch use and timing accuracy can be very difficult for new users and must be taught. One common method to teach switch activation and use is to interface a switch with battery-operated toys and games, or home or work appliances to increase motivation and teach the concepts used in indirect selection.
Fairly recent developments include eye-gaze switches, which calibrate intentional eye movement patterns and select targets such as individual keys on an onscreen keyboard. Other new developments include brain wave technology (Eye and Muscle Operated Switch [EMOS]) that responds to excitation of alpha waves to trigger a selection.
Displays
These human-technology interface concepts apply to all forms of AT, whether it is being used for seating, mobility, communication, computer operation, or control of the environment. Good assessment skills and a focus on clients and their goals and needs are essential for human-technology interface success and prevention of assistive devices abandonment.33
Assistive Technology for Communication Disorders
Vocal communication allows humans to interact, form relationships, and direct the events of their lives to enable choice and participation. Human communication is based on having both receptive and expressive language abilities and the physical capacity to reliably produce intelligible speech sounds. Communication impairment can result from congenital conditions such as mental retardation, cerebral palsy, developmental verbal apraxia, and developmental language disorders. Other impairments can be acquired through traumatic brain injury, stroke, multiple sclerosis, amyotrophic lateral sclerosis, tetraplegia, ventilator dependence, and laryngectomy resulting from cancer.3 AT devices that meet the needs of persons with many types of speech and language impairment are commonly called augmentative and alternative communication (AAC) devices, because they can either support or substitute for expressive language impairments. More recently the term speech-generating device has entered into the medical vocabulary to differentiate AAC devices from basic computer devices, especially when seeking third-party funding such as that from Medicaid and Medicare.8
Some individuals are completely unable to speak or have such severe expressive difficulties that only those very familiar with them are able to communicate effectively with them. Many devices are available for these individuals, ranging from simple, low-tech picture books to high-end, sophisticated electronic devices with digitally recorded or synthetic text-to-speech output capable of producing complex language interactions (Figure 23-2).
Although AAC devices are extremely useful to nonspeaking individuals, they do not replace natural communication. AAC device use should be encouraged along with all other available communication modalities such as gestures, vocalizations, sign language, and eye gaze.28
There are no firm cognitive, physical, or developmental prerequisites for using an AAC device. Instead, comprehensive evaluation techniques are used to match the individual’s abilities and communication needs with the appropriate AAC technologies. A qualified team of clinicians performs this evaluation, with input from the individual, family members, teachers, employers, and others. Because speaking is considered to be a critical human function, many parents and family members wait to seek out AAC devices in the hope that natural speech will develop. Research shows, however, that using an AAC device can actually support verbal language development, and can, in fact, increase the potential for natural speech to develop.3 Children and adults with severe communication impairments can benefit socially, emotionally, academically, and vocationally from using a device that allows them to communicate their thoughts, learn and share ideas, and participate in life activities.2
Nonelectronic Systems
Adults with progressive diseases such as amyotrophic lateral sclerosis or multiple sclerosis can also choose to use low-tech picture or alphabet boards as a supplement to verbal communication when they are fatigued, or as their ability to verbally communicate decreases. Many of these adults choose to use both low- and high-tech communication systems depending on their environment and their comfort level with technology.9
Electronic Voice Output Systems: Digital Speech
Devices such as One Step, Step by Step, and Big Mac (Figure 23-3) are simple and relatively inexpensive, and are designed to communicate quick, simple messages such as “hi,” “let’s play,” or “leave me alone.” These technologies are often used by very young children who are beginning communicators, or by those who have significant cognitive impairments. They are not appropriate for individuals needing or wanting to communicate complex thoughts and feelings.12
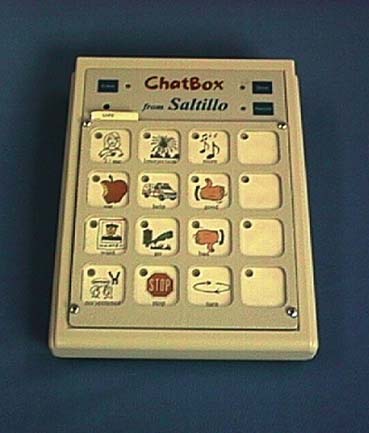
Complex digitized devices store several minutes of recorded voice that is usually associated with representative pictures or icons on a keyboard. These devices are often used by people who are not yet literate, have developmental disabilities, or simply wish to have a simple device to use when going to the store or out to eat. Examples are the SuperTalker, the ChatBox (Figure 23-4), and the Springboard.
Portable Amplification Systems
For people who speak quietly because of low breath support or other difficulties with phonation, portable amplification systems that function like a sound system in a large lecture hall are available. The Speech Enhancer processes speech sounds for people with dysarthria and enables improved recognition by others. Users wear a headset with a microphone attached to a portable device, and their clarified voice is projected via speakers attached to the unit.
Assistive Technology for Mobility Impairments
Upper Body Mobility Devices
Alternate computer keyboards come in many shapes and sizes. Expanded keyboards such as the Intellikeys (Figure 23-5) provide a larger target or key surrounded by inactive space than is found in a standard keyboard. Options such as delayed activation response help individuals who have difficulty with pointing accuracy or removing a finger after activating a key. Individuals unfamiliar with a standard QWERTY keyboard layout have the option for alphabetical layout. This is often helpful for young children who are developing literacy skills, as well as for adults with cognitive or visual impairments.
Lower Body Mobility Devices
Individuals with spinal cord injury, spina bifida or cerebral palsy often have lower body mobility impairments. AT solutions can include crutches, a rolling walker, a powered scooter, or a manual or powered wheelchair (see Chapter 17). Simple environmental modifications or adaptations, such as installing a ramp instead of stairs, raising the height of a desk, or widening doorways, can be critical facilitators for these individuals and might be all that is needed. For other activities or to increase participation, adding automobile hand controls, adapting saddles for horseback riding, or using sit-down forms of downhill skiing is possible (Figure 23-6).
Assistive Technology for Ergonomics and Prevention of Secondary Injuries
Many of the AT devices described in this chapter (i.e., alternate and specially designed ergonomic keyboards, VR software, and other technologies designed to minimize keystrokes) can also provide useful solutions for individuals with RSIs. There are also Internet-based resources that target ergonomic issues, such as those found in Table 23-1.
ANSI, Almerican National Standards Institute; BHMA, Builders Hardware Manufacturers Association; FAQs, frequently asked questions; NASA, National Aeronautics and Space Administration; NIOSH, National Institute for Occupational Safety and Health; OSHA, Occupational Safety and Health Administration.
Electronic Aids to Daily Living
ECU devices had the same general goal, but the name failed to reflect the goal, particularly to funding agencies. EADLs expand ADL equipment to include equipment that happens to use batteries or plug into the wall, but still shares the same goal—increasing independence in tasks of daily living.
Assistive Technology for Hearing Impairments
Cochlear Implants
When the hearing system is impaired at the level of the middle ear or the cochlea, a highly specialized form of AT is used to create an alternate means of stimulating the auditory nerve. This technology is implanted surgically with an electrode array placed within or around the cochlear structure. The external portion, a microphone, relays speech and environmental sound to the implanted portion, which is programmed to process, synchronize, and stimulate electrodes appropriately. This system requires a battery pack worn on the body or behind the ear.8 It also requires an experienced audiologist to teach the individual to use the acoustic cues produced by the cochlear implant as a substitute for natural hearing.
Assistive Technology for Visual Impairments
Low-Tech Visual Aids
A variety of AT devices and strategies can help individuals with visual impairments become more mobile; perform daily activities, such as reading, writing, and personal care; and participate in recreational activities. Among low-tech solutions are simple handheld magnifiers, the use of large print, and mobility devices for safe and efficient travel (e.g., a white cane; Figure 23-7). High-contrast tape or markers can also be used to indicate hazards, what an item is, or where it is located.
Books on tape are another resource for individuals with severe visual impairments. In addition to commercially available tapes for sale and at public libraries, special libraries provide print materials in alternate formats for persons with visual, physical, and learning impairments. Borrowers can arrange to have textbooks and other materials translated into alternate formats. For more information, contact the American Federation for the Blind or the National Library Service for the Blind and Physically Handicapped (http://www.loc.gov/nls/) (Box 23-2).
BOX 23-2 Resources for Persons With Low Vision or Blindness
High-Tech Visual Aids
Numerous high-tech solutions exist for persons with visual impairments. Computers outfitted with a speech synthesizer and specialized software, such as Jaws or WindowEyes, allow navigation of the desktop, operating system, applications, and documents, as well as the entire Internet. Any digital text can be heard aloud by the person using this software. For text that is printed, such as menus, memos, and letters, using a technology called optical character recognition allows a page scanner and software to convert print into digital form. It can then be listened to through the computer’s speech synthesizer or converted to Braille or large print.
For individuals with some degree of visual ability, screen magnification software such as Zoomtext (Figure 23-8) or MAGic enables the user to choose the amount (2 to 20 times) and type of magnification preferred for optimal computer access. Many magnification applications combine enlargement with speech synthesis or text to speech.
Assistive Technology for Cognitive and Learning Disabilities
Cognitive disabilities include disorders such as traumatic brain injury, mental retardation, developmental disabilities, autism, Alzheimer disease, learning disability, fragile X syndrome, and other disorders, both developmental and acquired. Most individuals in this group have not had the benefit of using AT devices because relatively few products have been specifically developed for intellectual impairments. In addition, families, teachers, and others providing support services for individuals with cognitive impairments have generally not been aware of the potential usefulness of AT.40
In 2004 the U.S. Department of Education, National Institute on Disability Research and Rehabilitation, recognizing the need to increase AT development for persons with cognitive disabilities by funding, funded the nation’s first Rehabilitation Engineering Research Center for the Advancement of Cognitive Technologies (RERC-ACT; www.rerc-act.org). The RERC-ACT is developing a wide range of new ATs designed to facilitate vocational and literacy skills, service provision, and enhanced caregiving supports for persons with significant cognitive impairments.
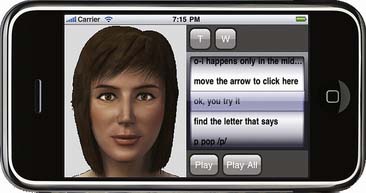
One of the newer developments from the RERC-ACT is the use of intelligent agents to interactively help people with everyday tasks in education, health care, and workforce training. The systems are designed to assess, instruct, or assist new readers and learners, as well as people who have speech, language, reading, or cognitive difficulties. The intelligent or “animated” agent is available on desktop or mobile computing devices. It is being used to assist persons with cognitive disabilities to learn new job tasks or to prompt them through various steps within a task, or both (Figure 23-9).
Other RERC-ACT work includes the development of “batteryless” micropower sensors. Access to low levels of power and the elimination of batteries in sensor technologies for persons with cognitive and physical disabilities enable additional prompts or inputs based on time, weight, location awareness, and other context-aware sensoring capabilities. This technology enables developers to use context-aware sensors in a multitude of environments and other ATs to facilitate the safety, capacity, and well-being of persons with cognitive disabilities. This new field of “cognitive technologies” promises numerous advances during the next decade.
Prompting Technologies
Recent mainstream technology developments include handheld personal digital assistants. AbleLink Technologies, Inc. have used this technology and developed software applications (PocketCoach; Figure 23-10) that provide auditory prompts for individuals with cognitive disabilities. This software can be set up to prompt an individual through each step of a task as simple as mopping a floor, or a task as complex as solving a math problem. The latest version of this software combines both voice prompts with visual prompts (Visual Assistant). The individual setting up the system for a user can simply take digital pictures with the accompanying camera and combine them with digitally recorded voice prompts to further facilitate memory and cognition.
Selecting Appropriate Assistive Technologies
Abandonment
Practitioners are sometimes surprised to learn that not everyone with a disability enjoys using technology, however useful it might appear. Depending on the type of technology, nonuse or abandonment can be as low as 8% or as high as 75%. On average, one third of more optional assistive technologies are abandoned, most within the first 3 months.23
Research has not yet been done to determine the number of individuals who are unhappy with their devices, but who must continue to use them because they cannot abandon them without severe consequences.22,29–31 For example, an individual who has just received a new wheelchair that does not meet expectations simply cannot stop using the chair, but must wait until third-party funding becomes available again (typically several years). Alternatively, the individual must engage in potentially difficult and unproductive discussions with the vendor, who has more than likely provided the chair as it was prescribed by the assessment team.
Research does tell us that the main reason individuals with disabilities choose not to use assistive devices is because practitioners failed to consider their opinions and preferences during the process of selecting the device. In other words, the person with a disability was not included as an active member of the team during the evaluation process.10,11,22,27
Phase 1 of the Assessment Process
Knowledge within the field of AT continues to expand and change, sometimes on a daily basis. This directly affects whether the AT device recommended by the assessment team will be used or abandoned by the consumer.15,19 As a result of rapidly changing information, the evaluation process continues to be refined. Many researchers are working to develop standardized AT measurement tools,∗ but the fact remains that few resources are available to guide practitioners who have not received formalized training in AT assessment.
As mentioned earlier in this chapter, the most common reason AT is abandoned is because the needs and preferences of the consumer are not taken into account during the evaluation process. Other reasons cited for abandonment of devices include the following22:
At the initial meeting, team members spend some time getting to know the individual. Using methods described by Cook and Hussey8 and Galvin and Scherer,10 the team identifies the life roles of the consumer (e.g., student, brother, or musician) and the specific activities engaged in by the individual to fulfill that life role. For example, if a young man is a “brother,” that means he might play hide and seek with a sibling, squabble over toys, or otherwise engage in brotherly activities. If he is a musician, then he might want or need to have access to musical instruments, sheet music, or simply a radio.
Next, the team identifies any problems that might occur during the individual’s daily activities. For example, the musician might not have enough hand control to manage recording equipment, or could experience visual or cognitive difficulties with sheet music. The team asks specific questions about where and when these difficulties occur (activity limitations). Perhaps problems occur when the individual is tired or not properly positioned, or when trying to communicate with others. The individual is also asked to describe instances of success with these activities and to discuss what made them successful (prior history with and without technology). By now the team is usually able to recognize patterns of success and failure from the individual’s perspective as common limitations across environments emerge.
Phase 2 of the Assistive Technology Assessment
AT professionals, in consultation with the physician, should also anticipate future needs (e.g., physical and cognitive maturation), and final decisions should consider both the expected performance and durability of the device.31
Writing the Report
It is also extremely important that all components of the AT device be included in the list of recommended equipment (e.g., cables, ancillary peripherals, and consumable supplies). In many instances devices are recommended for purchase as a “system.” As a result, acquisition can be delayed for months because an item was not included in the initial list. An estimate of the amount of time, cost, and source of training should also be included at this point. Purchasing AT devices without paying for the AT services needed to learn how to use and integrate the devices into identified life activities will result in low use or abandonment.29–31
Physician Responsibilities
Prescribing the Technologies
The American Medical Association36 recommends the following items be considered when prescribing AT and certifying medical necessity: The physician must provide evidence of individual medical necessity for the specific AT being prescribed and be prepared to talk with insurance company representatives about the medical necessity of complex assistive technologies (e.g., power wheelchairs and AAC devices). Reviewing a comprehensive assessment report from the AT assessment team should supply all the needed information.
Documentation in the Medical Record
Funding Assistive Technology
Funding for AT is also available from other federal and state government entities, such as the Veterans Administration, State Vocational Rehabilitation Agencies, State Independent Living Rehabilitation Centers, and State Department of Education Services. Local school districts might also fund education-related AT for children.13
Funding is generally available for AT, but persistence and advocacy by the AT provider are required for success.32,35 The AT provider must also keep abreast of the requirements of various funding sources, to direct the client to appropriate organizations. Private funding is often available through subsidized loan programs, churches, charitable organizations, and disability-related nonprofit groups. Often funding from several sources is needed to reduce personal out-of-pocket costs. It is important that the presumed availability of funding not drive the evaluation process and limit the options that are considered for an individual. When the need and justification for a particular AT solution are clear, it becomes much easier to locate a source of funding and make the case for purchase of the AT device or service.
Beukelman and Mirenda3 identify five steps in developing a funding strategy:
1. [Anonymous]. The Rehabilitation Act of 1973, as amended. 1973.
2. Ball L, Beukelman D, Patee G: Augmentative and alternative communication clinical decision making for persons with ALS, Augment Altern commun. 2002:7–12.
3. Beukelman D.R., Mirenda P. Augmentative and alternative communication: management of severe communication disorders in children and adults, ed 2. Baltimore: Paul H Brookes; 1998.
4. Blake D.J., Bodine C. An overview of assistive technology for persons with multiple sclerosis. J Rehabil Res Dev. 2002;39:299-312.
5. Bodine C., Beukelman D.R. Prediction of future speech performance among potential users of AAC systems: a survey. Augment Altern Commun. 1991;7:100-111.
6. Bromley BE: Assistive technology assessment: a comparative analysis of five models. Proc CSUN 2001.
7. Chatman A., Hyams S., Neel J., et al. The Patient-Specific Functional Scale: measurement properties in patients with knee dysfunction. Phys Ther. 1997;77:820-829.
8. Cook A.M., Hussey S.M. Assistive technologies: principles and practice, ed 2. St Louis: Mosby; 2002.
9. De Ruyter F., Kennedy M.R., Doyle M. Augmentative communication and stroke rehabilitation: who is doing what and do the data tell the whole story?. Boston: Third Annual National Stroke Rehabilitation Conference; May 10-11,1990.
10. Galvin J.C., Scherer M. Evaluating, selecting, and using appropriate assistive technology. Gaithersburg: Aspen; 1996.
11. Gray D.B., Quatrano L.A., Lieberman M. Designing and using assistive technology: the human perspective. Baltimore: Paul H Brookes; 1998.
12. Grove N. Augmentative and alternative communication: management of severe communication disorders in children and adults. J Intellect Disabil Res. 1994;38:219-220.
13. Hager R.M. Funding of assistive technology: state vocational rehabilitation agencies and their obligation to maximize employment. Buffalo: Neighborhood Legal Services; 1999.
14. James P., Thorpre N. Ancient inventions. New York: Ballentine Books; 1994.
15. Jutai J. Quality of life impact of assistive technology. Rehabil Eng. 1999;14:2-7.
16. King T.W. Assistive technology: essential human factors. Needham Heights: Allyn & Bacon; 1999.
17. Klund J. A crash course on alternative access. Technol Spec Interest Sect Q. 2001:1-3.
18. La Plante M.P. The demographics of disability. Milbank Q. 1991;69:55-77.
19. Nagi S. Some conceptual issues in disability and rehabilitation. In: Sussman M., editor. Sociology and rehabilitation. Washington DC: American Sociological Association, 1965.
20. Patterson D.J., Liao L., Fox D., et al. Inferring high-level behavior from low-level sensors. In: McCarthy A.D., Kautz H., et al, editors. UBICOMP 2003: the Fifth International Conference on Ubiquitous Computing. New York: Springer-Verlag, 2003.
21. Pentland A: Machine understanding of human action. In 7th International Forum on Frontier of Telecom Technology November, 1995. Available at: http:\\www.white.media.mit.edu/vismod/demos/ive/. Accessed August 8, 2010.
22. Phillips B., Zhao H. Predictors of assistive technology abandonment. Assist Technol. 1993;5:36-45.
23. Pope A.M., Tarlove A.R. Disability in America: toward a national agenda for prevention. Washington, DC: National Academy Press; 1991.
24. Public Law 93-113. Section 508 of the Rehabilitation Act of 1973, as amended 29 USC 794 (d). 1998.
25. Public Law 100-407. Technology Related Assistance for Individuals with Disabilities Act of 1988. Federal Register. August 1991;19:41272.
26. Public Law 108-446. The Individuals with Disabilities Education Act Amendments of 1997.
27. Riermer-Reiss M.L., Wacker Robbyn R. Factors associated with assistive technology discontinuance among individuals with disabilities. J Rehabil 66. 2000:44-49.
28. Romski M.A., Sevcik R.A. Language learning through augmented means: the process and its products. Baltimore: Paul H Brookes; 1993.
29. Scherer M: Assistive technology use, avoidance and abandonment: what we know so far. Proceedings of the 6th Annual Technology and Person with Disability Conference, Los Angeles, 1991.
30. Scherer M. Assistive technology: matching device and consumer for successful rehabilitation. Washington: American Psychological Association; 2002.
31. Scherer M, Coombs FK: Ethical issues in the evaluation and selection of assistive technology. Available at: http://www.gatfl.org/publications/ethical.pdf. Accessed August 8, 2010.
32. Scherer M.J. Living in a state of stuck: how technology impacts the lives of people with disabilities. Cambridge, MA: Brookline Books; 1993.
33. Scherer M.J. Living in the state of stuck: how technology impacts the lives of people with disabilities, ed 3. Cambridge: Brookline Books; 2000.
34. Scherer M.J., Cushman L.A. Measuring subjective quality of life following spinal cord injury: a validation study of the assistive technology device predisposition assessment. Disabil Rehabil. 2001;23:387-393.
35. Scherer M.J., McKee B.G. Assessing predispositions to technology use in special education: music education majors score with the ‘Survey on Technology Use.’. In: RESNA ‘94 Annual Conference. Arlington: Rehabilitation Engineering and Assistive Technology Society of North America; 1994.
36. Schwartzberg J.G., Kakavas V.K., Malkind S. Guidelines for the use of assistive technology evaluation, referral, prescription, ed 2. Chicago: American Medical Association; 1996.
37. The Rehabilitation Act Amendments of 1992 and Assistive Technology. Rehabilitation Engineering and Assistive Technology Society of North America: Assistive Technology Quarterly; 1993.
38. US Congress: Americans with Disabilities Act of 1990.
39. US Congress. Americans with Disabilities (ADA) accessibility guidelines for buildings and facilities. Washington, DC: US Architectural and Transportation Barriers Compliance Board; 1991. 91
40. Wehmeyer M.L., Kelchner K., Richards S. Individual and environmental factors related to the self-determination of adults with mental retardation. J Vocat Rehabil. 1995;5:291-305.
41. World Health Organization. International classification of functioning, disability and health: literature review on environmental factors. Geneva: WHO; 2000.
42. World Health Organization Committee for the International Classification of Functioning. International classification of functioning: ICF checklist. Geneva: WHO; 2002.