Chapter 16 Complications of Sacroiliac Joint Injection and Lateral Branch Blocks, Including Water-Cooled Rhizotomy
 Appropriate Accreditation Council for Graduate Medical Education mentored subspecialty training in interventional pain management is vital to ensure patient-centered care.
Appropriate Accreditation Council for Graduate Medical Education mentored subspecialty training in interventional pain management is vital to ensure patient-centered care. Accurate and expertly placed needles in appropriately selected patients are essential to ensure accurate diagnosis and successful treatment.
Accurate and expertly placed needles in appropriately selected patients are essential to ensure accurate diagnosis and successful treatment. The sacroiliac joint is a large structure with rich, variable innervation. Numerous techniques have been described for intraarticular, extraarticular, lateral branch, and RF treatments.
The sacroiliac joint is a large structure with rich, variable innervation. Numerous techniques have been described for intraarticular, extraarticular, lateral branch, and RF treatments. RF treatments are not created equal, and an appreciation for each underscores their different applications and associated risks.
RF treatments are not created equal, and an appreciation for each underscores their different applications and associated risks. Common complications, regardless of RF modality used, include transient increased localized pain and usually self-limiting neuritis.
Common complications, regardless of RF modality used, include transient increased localized pain and usually self-limiting neuritis. Infectious complications are uncommon if appropriate sterile technique and avoidance of multidosing from single-dose vials are used.
Infectious complications are uncommon if appropriate sterile technique and avoidance of multidosing from single-dose vials are used.Introduction
Estimates of sacroiliac joint sources of back and leg pain have been estimated to be between 10% and 38% using compared diagnostic injections, with a false-positive rate estimated between 0% and 53.8%.1–3 Not only have diagnostic provocative tests failed to be accurate,4,5 but there have been numerous efforts to treat sacroiliac joint pain, including intraarticular injections, extraarticular injections, radiofrequency (RF) treatments, fusion, and prolotherapy6–9 with level II-3 evidence for both short- and long-term relief.2
Sacroiliac pain or dysfunction has been implicated in diverse patient populations and associated morbidities, including pediatric low back pain, pregnancy, cancer, infection, ankylosing spondylitis, and inflammatory bowel disease.10–13 Controversy surrounds diagnostic accuracy and technique14–21 because some advocate intraarticular injections but others advocate extraarticular injections or lateral branch blocks before RF treatment. Summarily, interventions are directed to either the afferent nociceptive nerves supplying the joint or the actual joint itself. A corollary can be drawn to zygapophyseal treatments because intraarticular or median branch blocks are used before RF treatment, just as sacroiliac intraarticular injection or lateral branch blocks are performed before using RF. Although widely accepted clinically, this treatment algorithm has recently been questioned.3
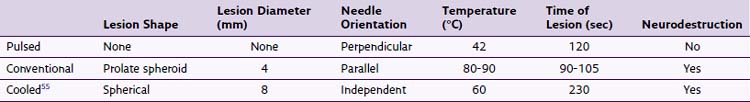
Before proceeding, readers are directed to the chapters that correspond to sacroiliac joint injections; lateral branch blocks; and traditional (see Fig. 15-2), pulsed, and cooled RF treatments (see Fig. 15-5). A brief review of the differences in RF modalities are listed in Table 16-1, and reviewed elsewhere in the text (see Chapter 7). Other modalities to treat sacroiliac joint pain include fusion and prolotherapy,22 this chapter focuses on complications specific to RF neurotomy.
Even after appropriate safeguards and training, significant complications have been described in scattered case reports. Theoretical risks are listed in Box 16-1, and they are typically localized or systemic in nature.
Selected Complications
Meta-analysis of treatment outcomes is difficult because the treatment arm is highly variable regarding RF technique, inconsistent patient selection, outcome endpoints, and definitions of success. Although there is a plethora of literature describing sacroiliac joint interventions, few describe complications.2–4,9,10,13,23–29
Postprocedure Pain or Neuritis
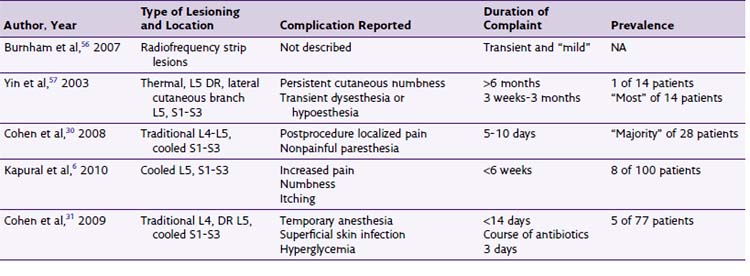
Transient postprocedural pain often follows RF treatments and has been described in numerous studies for lumbar facetogenic interventions; however, few describe sacroiliac lateral branch denervation. Cooled RF and traditional thermal RF have been accompanied by postprocedure local pain (Table 16-2), typically of a transient nature,6,30,31 and Vallejo et al9 reported that no complications arose from pulsed RF treatments of the lateral branches.
No published study has compared the efficacy and complications of cooled versus traditional RF. In an unpublished retrospective analysis of 88 patients at the Cleveland Clinic, there was no statistically significant difference in duration of pain relief, and anecdotally, more patients who underwent cooled RF reported transient postprocedure localized back pain. Kapural et al6 described transient itching, numbness, and pain.
Steroids are injected after denervation to lessen postprocedural pain. This may seem counterintuitive because the goal in thermal rhizotomy is to create a histologically detectable lesion, blocking neural afferent nociception. Dobrogowsi et al32 investigated strategies to reduce the inflammatory pain associated with the lesioning using pentoxifylline or methylprednisolone. In a randomized prospective trial, patients were randomized to 1 mL of intraoperative methylprednisolone, pentoxifylline, or saline. No “severe local tenderness” was reported in either the methylprednisolone group or the pentoxifylline group.32 Other authors33 contend that 3-day dosage of enteral diclofenac is effective in reducing procedural pain after conventional RF neurotomy of lumbar median branches.
False-Positive Results
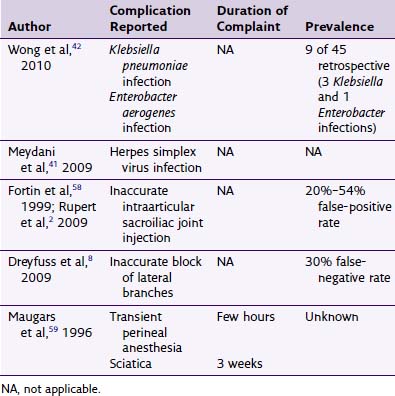
False-positive results have been reported to be 0% to 53% using controlled diagnostic injections or post-block provocative sacroiliac maneuvers.2,4–6,34 These problems may result from numerous factors, including oversedation, large-volume injectate, inaccurate needle placement, or anatomic innate defects in sacroiliac ventral or dorsal capsule. Similarly, false-negative results or treatment failures can result if interosseous or dorsal sacroiliac joint ligaments are not anesthetized because they are known to contribute to these pain complaints. Furthermore, anterior sacroiliac joint innervation is largely ignored as a significant contribution to sacroiliac joint pain.
There have been numerous techniques suggested to enter the sacroiliac joint for arthrography,14–19 to perform lateral branch blocks,5,8,34,35 and for denervation.6,9,11,27,31,36–40 Whatever the method of diagnosing sacroiliac joint pain, accuracy hinges on small-volume injectate and controlled diagnostic comparative blocks, although cost effectiveness has recently come into question.3 Cohen et al3 suggested that the cost of RF treatment without diagnostic injection was almost $9000 cheaper, although indirect results suggest a better treatment outcome with dual diagnostic injections before neurotomy, keeping a keen eye on potential placebo cofounders.
Infections
There are scattered reports of infection for both sacroiliac injection and RF therapy. Some suggest that the thermal nature of RF treatment may decrease the chance of infection.3 Others suggest that steroids may innately increase the infectious potential because they are immunosuppressive.38 Interestingly, only one report of infectious complication after block therapy was found after an exhaustive Medline search with search terms “sacroiliac and infection.” Meydani et al41 report a herpes simplex virus type II outbreak (Fig. 16-1) after sacroiliac injection therapy (Table 16-3), confirmed by unroofing vesicle and DNA analysis.

Fig. 16-1 Herpetic outbreak.
(From Meydani A, Schwartz A, Foye PM, Patel AD: Herpes simplex following intra-articular sacroiliac corticosteroid injection, Acta Dermatoven APA 16(3):135-137, 2009.)
Cohen et al31 described one superficial infection after RF treatment of 77 patients that resolved after a course of oral antibiotics. Single-use vials should always be used for individual patients because this was a major source of contamination in an Enterobacter aerogenes and Klebsiella pneumoniae bacteremia outbreak after sacroiliac joint injection reported in 2008.42
There have been no reported cases of epidural or paraspinal abscess after sacroiliac joint interventions. The only serious infections described in the literature are those of hematogenic septic arthritis remote from sacroiliac joint interventions.43
Bleeding
The incidence of hematoma after sacroiliac joint injection is unknown but is likely less than for spinal or epidural anesthetic procedures, estimated to be one in 222,000 and one in 150,000, respectively.28 In fact, no cases have been reported. However, if epidural hematoma is suspected, it should be promptly investigated and treated. Symptom and sign presentation is dependent on the anatomic location of the bleed, and a high index of suspicion is needed for diagnosis. Early neurosurgical consultation is essential because prognosis requires expeditious evacuation within 8 hours of neurologic deficit presentation.29
Burn Injuries
No burn injuries have been reported with sacroiliac joint denervation; however, the potential can be extrapolated from the facetogenic literature. Burn injuries were the result of equipment malfunction, insulation breaks within the electrodes, unipolar electrosurgical unit return plate, or unknown causes.44–46 Appreciation of circuit differences between grounded and ungrounded systems is encouraged as operating room power supplies are typically isolated, ungrounded systems, where office buildings are typically grounded systems. By design, isolated systems are more difficult to deliver aberrant current. Furthermore, burn severity is related to current density, either greater the current or the smaller the area applied.
Pituitary–Adrenal Axis Suppression
Although numerous studies have demonstrated pituitary–adrenal suppression with epidural or intraarticular administration of glucocorticoids,47–51 none has investigated axis depression from sacroiliac interventions. From the available data, hypothalamic pituitary adrenal axis suppression could be assumed to be depressed for 4 weeks, and insulin sensitivity may be adversely affected for 1 week. Cushing syndrome, steroid myopathy, aseptic meningitis, and anaphylactoid reactions have been reported after single epidural steroid injections.52,53 Other glucocorticoid side effects, including musculoskeletal, ophthalmologic, gastrointestinal, cardiovascular, secondary cortisol deficiency, gynecologic, neurologic, hematologic, psychiatric, and dermatologic, have been described.54
1 Manchikanti L, Singh V, Pampati V, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308-316.
2 Rupert MP, Lee M, Machikanti L, et al. Evaluation of sacroiliac joint interventions: a systemic appraisal of the literature. Pain Physician. 2009;12:399-418.
3 Cohen SP, Williams KA, Kurihara C, et al. Multicenter, randomized comparative cost-effectiveness study comparing 0, 1 and 2 diagnostic medial branch (facet joint nerve) block treatment paradigms before lumbar facet radiofrequency denervation. Anesthesiology. 2010;113:395-405.
4 Laslett M, Young SB, Aprill CN, McDonald B. Diagnosing painful sacroiliac joints: a validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother. 2003;49:89-97.
5 van der Wurff P, Buijs EJ, Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil. 2006;87:10-14.
6 Kapural L, Stojanovic M, Bensitel T, Zovkic P. Cooled radiofrequency of L5 dorsal ramus for RF denervation of the sacroiliac joint: technical report. Pain Med. 2010;11:53-57.
7 Cohen SP, Strassels SA, Kurihara C, et al. Outcome predictors for sacroiliac joint (lateral branch) radiofrequency denervation. Reg Anesth Pain Med. 2009;34(3):206-214.
8 Dreyfuss P, Henning T, Malladi N, et al. The ability of multi-depth sacral lateral branch blocks to Anesthetize the sacroiliac joint complex. Pain Med. 2009;10(4):679-688.
9 Vallejo R, Benyamin RM, Kramer J, et al. Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain Med. 2006;7(5):429-434.
10 Manchikanti L, Singh V, Pampati V, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308-316.
11 Vanelderen P, Szadek K, Cohen SP, et al. Evidence based medicine 13. Sacroiliac joint pain. Pain Pract. 2010;5:470-478.
12 Moghadam A, Talebi-Taher M, Dehghan A. Sacroiliitis as an initial presentation of acute lymphoblastic leukemia. Acta Clin Belg. 2010;65(3):197-199.
13 Hwangbo Y, Kim HJ, Ryu KN, et al. Sacroiliitis is common in Crohn’s disease patients with perianal or upper gastrointestinal involvement. Gut Liver. 2010;3(4):338-344.
14 Dussault RG, Kaplan PA, Anderson MW. Fluoroscopically guided sacroiliac joint injection. Radiology. 2000;214:273-277.
15 Bogduk N. Practice guidelines. In: Spinal diagnostic and treatment procedures. San Francisco: ISIS; 2004:66-86.
16 Ebraheim NA, Xu R, et al. Sacroiliac joint injection: a cadaver study. Am J Orthop. 1997;26:338-341.
17 Fortin JD, et al. Sacroiliac joint injection: pain referral maps upon applying a new injection/arthrography technique. Part 1: asymptomatic volunteers. Spine. 1994;19(13):1475-1482.
18 Centeno C. How to obtain an SIJ arthrogram 90% of the time in 30 seconds or less. Pain Physician. 2006;9:159.
19 Daitch J, Frey M, Snyder K. Modified SIJ injection technique. Pain Physician. 2006;9:367-368.
20 Schwarzer AC, Aprill CN, Bognuk N. The sacroiliac joint in chronic back pain. Spine. 1995;20(1):31-37.
21 Fortin JD, Tolchin RB. Sacroiliac arthrograms and post-arthrography computerized tomography. Pain Physician. 2003;6:287-290.
22 Kim MW, Lee HG, Wo JC, et al. A randomized controlled trial of intraarticular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010;16(12):1285-1290.
23 Maigne JY, Aivakiklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation test in 54 patients with low back pain. Spine. 1996;21:1889-1892.
24 Irwin RW, Watson T, Minick RP, Ambrosius WT. Age, body mass index, and gender differences in sacroiliac joint pathology. Am J Phys Med Rehabil. 2007;86:37-44.
25 Cohen SP, Abdi S. Lateral branch blocks as a treatment for sacroiliac joint pain: a pilot study. Reg Anesth Pain Med. 2003;28(2):113-119.
26 McKenzie-Brown AM, Shah RV, Sehgal N, Everett CR. A systematic review of sacroiliac interventions. Pain Physician. 2005;8:115-125.
27 Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine. 1995;20:31-37.
28 Horlocker TT, Rowlingson JC, Enneking FK, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition). Reg Anesth Pain Med. 2010;35(1):64-101.
29 Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165-1177.
30 Cohen SP, Hurley RW, Buckenmaier CC, et al. Randomized placebo controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109:279-288.
31 Cohen SP, Strassels SA, Kurihara C, et al. Outcome predictors for sacroiliac joint (lateral branch) radiofrequency denervation. Reg Anesth Pain Med. 2009;34(3):206-214.
32 Dobrogowski J, Wrzosek A, Wordliczek J. Radiofrequency denervation with or without addition of pentoxifylline or methylprednisolone for chronic lumbar zygapophysial joint pain. Pharmacol Rep. 2005;57:475-480.
33 Ma K, Yiqun M, Wang W, et al. Efficacy of diclofenac sodium in pain relief after conventional radiofrequency denervation for chronic facet joint pain: a double blind randomized controlled trial. Pain Med. 2010;12(1):27-35.
34 Cohen SP, Hurley RW, Buckenmaier CC3rd, et al. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109(2):279-288.
35 Dreyfuss P, Snyder BD, Park K, et al. The ability of single site, single depth sacral lateral branch blocks to anesthetize the sacroiliac joint complex. Pain Med. 2008;9:844-850.
36 Ferrante FM, King LF, Roche EA, et al. Radiofrequency sacroiliac joint denervation for sacroiliac syndrome. Reg Anesth Pain Med. 2001;26:137-142.
37 Kapural L, Nageeb F, Kapural M, et al. Cooled radiofrequency system for the treatment of chronic pain from sacroiliitis: the first case-series. Pain Pract. 2008;8(5):348-354.
38 Hansen HC, McKenzie-Brown AM, Cohen SP, et al. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007;10:165-184.
39 Stone JA, Bartynski WS. Treatment of facet and sacroiliac joint arthropathy: steroid injections and radiofrequency ablation. Tech Vasc Interventional Radiol. 2009;12:22-32.
40 Cosman ERJr, Gonzalez CD. Bipolar radiofrequency lesion geometry: implications for palisade treatment of sacroiliac joint pain. Pain Pract. 2011;11(1):3-22.
41 Meydani A, Schwartz A, Foye PM, Patel AD. Herpes simplex following intra-articular sacroiliac corticosteroid injection. Acta Dermatoven APA. 2009;16(3):135-137.
42 Wong MR, Del Rosso P, Heine L, et al. An outbreak of Klebsiella pneumoniae and Enterobacter aerogenes bacteremia after interventional pain management procedures, New York City 2008. Reg Anesth Pain Med. 2010;35(6):496-499.
43 Mancaarella L, De Santis M, Magarelli N, Ierardi AM, Bonomo L, Ferraccioli G. Septic Arthritis: an uncommon septic arthritis. Clin Exp Rheuatologu. 2009 Nov-Dec;27(6):1004-1008.
44 Shealy CN. Percutaneous radiofrequency denervation for spinal facets: treatment for chronic back pain and sciatica. J Neurosurg. 1975;43:448-451.
45 Katz SS, Savitz MH. Percutaneous radiofrequency rhizotomy of the lumbar facets. Mount Sinai J Med. 1986;53:523-525.
46 Ogsbury JS, Simon RH, Lehman RAW. Facet “denervation” in the treatment of low back pain. Pain. 1977;3:257-263.
47 Gevargez A, Groenemeyer D, Schirp S, Braun M. CT-guided percutaneous radiofrequency denervation of the sacroiliac joint. Eur Radiol. 2002;12:1360-1365.
48 Habib GS. Systemic effects of intra-articular corticosteroids. Clin Rheumatol. 2009;28:749-756.
49 Ward A, Watson J, Wood P, et al. Glucocorticoid epidural for sciatica: metabolic and endocrine sequelae. Rheumatology (Oxford). 2002;41:68-71.
50 Cook DM, Meikle AW, Bowman R. Systemic absorption of triamcinolone after a single intraarticular injections suppresses the pituitary-adrenal axis [abstract]. Clin Res. 1988;36(suppl A):121A.
51 Kay J, Findling JW, Raff H. Epidural triamcinolone suppresses the pituitary-adrenal axis in human subjects. Anesth Analg. 1994;79:501-505.
52 Knight CL, Burnell JC. Systemic side effects of extradural steroids. Anaesthesia. 1980;35:593-594.
53 Boonen S, Van Distel G, Westhovens R, et al. Steroid myopathy induced by epidural triamcinolone injection. Br J Rheumatol. 1995;34:385-386.
54 Nesbit LT. Minimizing complications from systemic glucocorticosteroid use. Dermatol Clin. 1995;13:925-939.
55 Kapural L, Mekhail N, Hick D, et al. Histological changes and temperature distribution studies of a novel bipolar radiofrequency heating system in degenerated and nondegenerated human cadaver lumbar discs. Pain Med. 2008;9:68-75.
56 Burnham RS, Yasui Y. An alternate method of radiofrequency neurotomy of the sacroiliac joint: a pilot study of the effect of pain, function, and satisfaction. Reg Anesth Pain Med. 2007;32:12-19.
57 Yin W, Willard F, Carreiro J, Dreyfuss P. Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine. 2003;28(20):2419-2425.
58 Fortin JD, Washington WJ, Falco JE. Three pathways between the sacroiliac joint and neural structures. Am J Neuroradiol. 1999;20:1429-1434.
59 Maugars Y, Mathis C, Berthelot JM, et al. Assessment of the efficacy of sacroiliac corticosteroid injections in spondyloarthropathies: a double-blind study. Br J Rheumatol. 1996;35:767-770.