CHAPTER 5 Complications of Knee Arthroscopy
CLINICAL OR MEDICAL COMPLICATIONS
Deep Venous Thrombosis and Pulmonary Embolus
Deep venous thrombosis (DVT) has been reported to be as high as 17.9% after arthroscopy of the knee. Some authors have stated that without proper screening, fatal pulmonary embolus (PE) may be as high as 1.3% of cases.1 At an advanced arthroscopic knee course in August 2006, the audience was surveyed; 4 out of 40 knee arthroscopic surgeons had experienced a fatal PE in their practice, with an incidence in this small group of 10%.2 Although arthroscopy of the knee is considered to be a “benign” procedure, one study noted at least one risk factor for DVT in 37% of patients undergoing routine knee arthroscopy.3 In 2004, Geerts and colleagues4 reported on multiple risk factors contributing to DVT and PE, including obesity, history of prior DVT, cancer, use of oral contraceptives, and increased age. Anderson and Spencer5 categorized the top 10 factors causing DVT and ranked them in terms of risk. Age older than 40 years was the most significant causative factor followed by obesity, prior history of DVT, cancer, bed rest longer than 5 days, major surgery, congestive heart failure, varicose veins, hip or lower extremity fracture, and estrogen treatment. They further noted that one or more risk factors increased the incidence of development of subclinical DVT or PE to 96.3%.
Eynon and associates6 were one of the first to suggest that all patients having routine knee arthroscopies should receive anticoagulant prophylaxis. One study has reported the incidence of DVT and/or PE when comparing a control group and a second group treated with low-molecular-weight heparin (LMWH) without any known risk factors to be as high as five times greater when diagnosed by ultrasound on days 7 and 10 postoperatively.7 Another study noted a 10 times greater incidence of DVT and/or PE after preoperative and postoperative treatment with LMWH when diagnosed with ultrasound at 12 and 31 days postoperatively.8 It is estimated that between 20% to 30% of calf thrombi propagate proximally to the popliteal and femoral veins, which have an increased chance of resulting in PE. Some have argued that pharmacologic DVT prophylaxis should be routinely prescribed to patients undergoing knee arthroscopy for that reason.1,6 However, there are no agreed on recommendations in the literature about prophylaxis for arthroscopy of the knee, with or without prior history of DVT or PE.1 We recommend that all those undergoing knee arthroscopy should be given acetylsalicylic acid (ASA) preoperatively and postoperatively for 4 weeks and that those with acquired, genetic, or hemostatic risk factors be placed on preoperative and postoperative warfarin (Coumadin) or LMWH for 3 to 4 weeks to reduce the possibility of PE or DVT.
Wrong-Site Surgery
Wrong-site surgery (WSS) accounts for approximately 2% of all orthopedic claims. However, 84% result in a mean court award to the plaintiff of $48,087. Most of these were knee arthroscopies. The Physician Insurer’s of North America recorded 331 WSS claims from 1985 to 1995, and 225 were against orthopedic surgeons.9 The incidence of WSS reported to the American Academy of Orthopaedic Surgeons (AAOS) between January 1995 and December 2003 were 17% wrong knee, 12% wrong person, and 10% wrong procedure. Interestingly, hospital-based ambulatory surgery centers had the highest incidence of errors, 53%. The three most important factors to prevent wrong-site surgery errors were preoperative patient identification, surgical site indelible marking, and the physician’s signature on the surgical site. When all three of these were done, there was a 0% failure rate. However, when only two of these three were done, there was a 12% incidence of failure.10 Additional analysis of the complications that occurred estimated that an orthopedic surgeon has a 25% chance of performing wrong-site surgery during his or her career and that WSS tends to increase with increasing age and increased caseloads.9,11
In a survey presented at the AAOS in 2005, 1575 Arthroscopy Association of North America members reported an incidence of one WSS for every 26,581 arthroscopic procedures that were performed. The average age of the respondents was 48.2 years, with a practice mean of 15.8 years; 8.5% of respondents had performed wrong-site arthroscopy at least once during their careers. In this survey report, the risk of WSS increases with surgeon age, increasing years of practice, and increased surgical volume.12 In Minnesota, in 2004, there were 22 adverse events reported—13 patients had the wrong body part operated on, in four cases the wrong patient was operated on, and in five cases the wrong procedure was performed. In 2005, in Minnesota, there were 26 adverse events—16 patients had the wrong body part operated on, in two cases the wrong patient was operated on, and in eight cases the wrong procedure was performed.13
Infection
The incidence of infection after knee arthroscopy has been reported to be from 0.04% to 0.42%.14–16 Risk factors that have been reported to contribute to knee arthroscopy infections include intra-articular steroids given intraoperatively, increased surgical time, prior surgical procedures, chondroplasty, and soft tissue débridement.17 The diagnosis of infection can be difficult to make immediately postoperatively. Persistent pain and swelling after arthroscopy should have joint aspiration and culture despite the absence of fever, erythema, leukocytosis, or benign-appearing joint fluid. This diagnosis needs to be made immediately, if possible, and then treated with knee arthroscopy, lavage, and 2 to 6 weeks of intravenous antibiotics. Antibiotic prophylaxis in knee arthroscopy has been discussed and debated by several authors. Based on objective published literature, there is no statistical improvement in infection rates with preoperative IV antibiotics in routine arthroscopic surgery of the shoulder and knee.18 However, in today’s legal climate, others have argued that prophylactic antibiotics may be considered the standard of care in the local community and should be given regardless.19 Suggestions to avoid infections include operating efficiently and using antibiotic prophylaxis on immunocompromised patients. Furthermore, avoid the use of intra-articular steroids immediately prior, during, or after surgery. Finally, treat a swollen extremely painful knee postoperatively with immediate aspiration, cultures, and then aggressive arthroscopic débridement if the culture is positive, followed by IV antibiotics.
TECHNICAL OR IATROGENIC COMPLICATIONS
Nerve and Vascular Injury
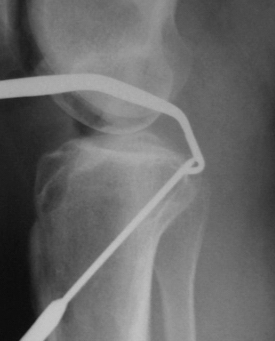
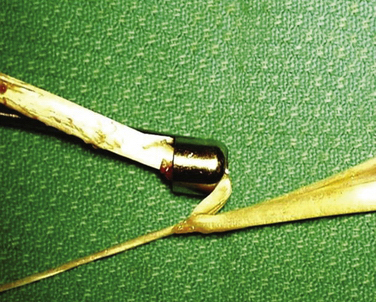
Early reported complications of meniscal repair were common; these included saphenous neuropathy medially and peroneal neuropathy laterally secondary to injury and for nerve entrapment. Other complications associated with open meniscal repair, including both outside-in and inside-out techniques, were arthrofibrosis, severe postoperative effusion, and superficial and deep infection. Combined complication rates were reported as high as 18%.20 Nerve and vascular injury have also been reported secondary to lateral meniscectomy and posterior cruciate and anterior cruciate ligament reconstruction. Despite the use of guide pins for the placement of the tibial guide pin (Fig. 5-1) during both anterior and posterior cruciate ligament reconstruction, popliteal artery injury (Fig. 5-2) continues to be of concern.21
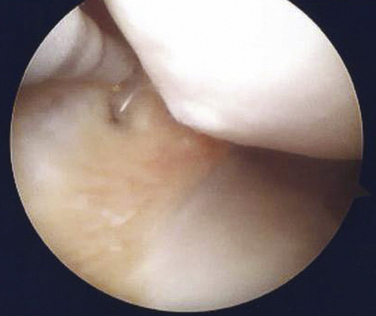
Chondral Injury
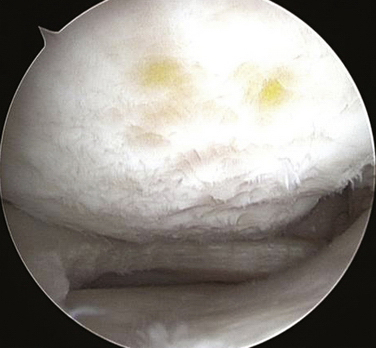
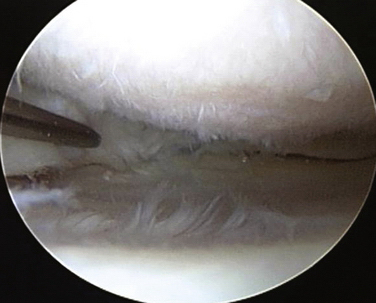
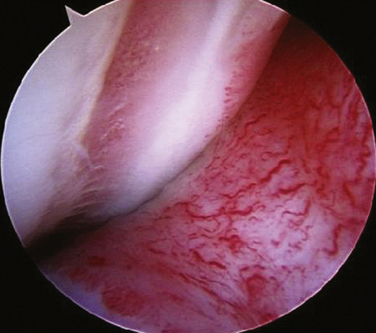
Iatrogenic chondral injury is common during routine meniscectomy, especially in a tight medial compartment. In our experience, the presence of articular scuffing will result in significant degenerative changes within a few years and sometimes even in a few months. Note the significant chondral injury at 1 year postoperatively in a 45-year-old patient after a routine meniscectomy (Fig. 5-3). After 4 years, significant changes can occur from a routine meniscectomy (Fig. 5-4). Articular cartilage is about 2000 μm thick. A motorized shaver will shave up to 253 ± 78 μm and a radiofrequency (RF) thermal device will destroy up to 200 μm of articular cartilage. Some authors have argued that use of a RF device is more conservative than using a shaver.22 In a series of 256 patients who had partial medial meniscectomies at a mean age of 47 years, with an average follow-up of 18.5 years, 63% had undergone grade I or II surface changes,23 yet 83% had good to excellent clinical results. In this series, age, gender, and meniscal tear type did not influence functional results.24 Factors such as the larger size of meniscal resection and female gender resulted in the most consistent associations with more x-ray evidence of osteoarthritis (OA) across multiple studies.25
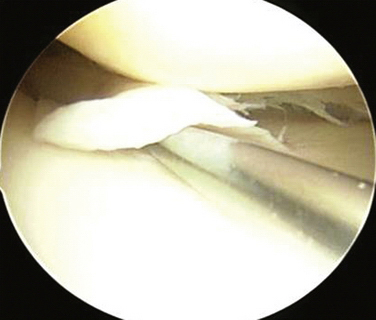
Chondral injury is also dependent on the type of tear that occurs. Complex and horizontal cleavage tears are highly associated with an increased incidence and severity of cartilage degeneration compared with other types of meniscal tears.26 In one study, 45 lateral meniscal tears were associated with another articular surface procedure within 13 years postmeniscectomy secondary to the development of OA.27,28 Suggestions to avoid chondral injury during meniscectomy include removing as little meniscal tissue as possible, but still leaving a stable meniscal remnant. Also, avoid damage to the articular surface with the meniscal resector tools.29 Furthermore, consider doing a partial intra-articular release of a portion of the medial collateral ligament (MCL) when the knee is too tight in the medial compartment before proceeding with meniscal resection, either using a pie crust technique with a spinal needle (Fig. 5-5) or cutting through the anterior portion of the MCL several millimeters from the meniscal rim with a cutting cautery (Fig. 5-6). Inadequate meniscal resection during meniscectomy with a retained superior or inferior horizontal cleavage flap has been implicated in causing long-term chondral damage (Fig. 5-7). Finally, not recognizing malalignment of the extremity will result in increasing failure rates subsequent to meniscectomy, with progressive OA of the meniscectomized compartment.30
Anterior Cruciate Ligament Surgery Complications
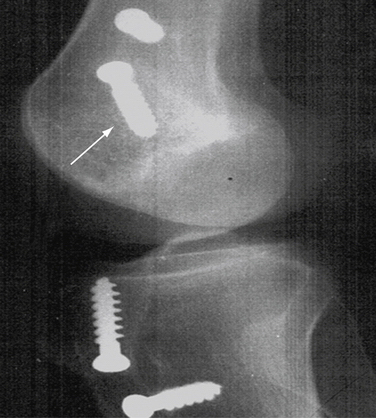
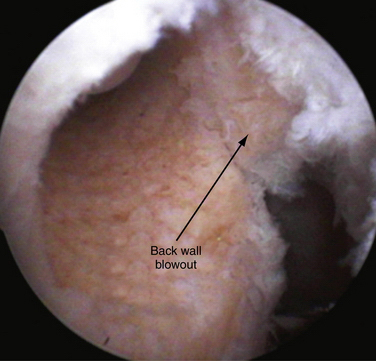
Anterior cruciate ligament (ACL) reconstruction complications are not uncommon with single- or double-bundled techniques. Anterior placement of the fixation device in the intercondylar notch (Fig. 5-8) or posterior placement of the fixation device in the tibia (Fig. 5-9) are not uncommon. Cyclops lesions (Fig. 5-10) are also common as well. There appears to be no advantage of supplemental aperture fixation with screws or bone cores to reduce tunnel widening. It has been argued that supplemental aperture fixation is associated with increased tunnel widening.31 Also, it has been suggested that leaving the stump of the ACL intact at the time of ACL surgery will reduce the incidence of cyclops lesions, because leaving the soft tissue in this area decreases the amount of debris that will surround the ACL in the tibia and reduce the amount of osteolysis that occurs next to the ACL.32 Delayed laxity, recurrent tearing, and graft failure are not uncommon. Furthermore, poor preparation of the hamstring graft so that it loosens during stress can occur. The allograft must be thawed prior to preparation to avoid stretching prior to implantation. Other complications include premature tearing of the hamstring graft during harvesting (Fig. 5-11) and posterior wall blowout (Fig. 5-12). Patellar fracture after patellar tendon bone (PTB) harvesting is becoming less common because of increased usage of allograft material but chronic anterior knee pain secondary to inadvertent infrapatellar nerve injury can occur subsequent to patellar tendon autograft harvesting. Double-bundle ACL reconstruction complications are primarily those of difficulty of placement of the double femoral tunnels. Also, fracture of the tunnel wall is not uncommon because it needs to be thin to place the tunnels in the anatomic position.33
MATERIAL- OR DEVICE-ASSOCIATED COMPLICATIONS
Biodegradable Implant Complications
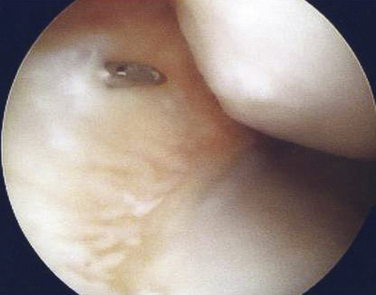
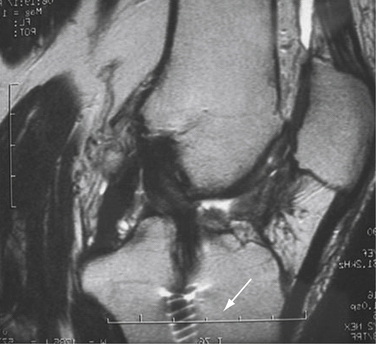
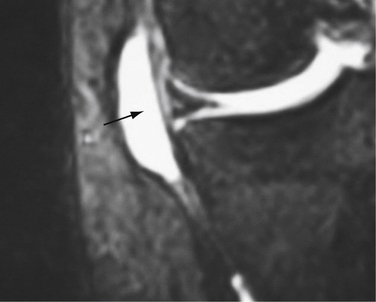
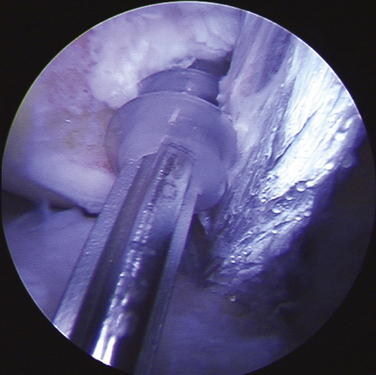
Failed resorption of biodegradable implants has been reported with multiple designs. Meniscal arrows (Biofix; Bionx Implants, ConMed Linvatec, Pa) and Biostingers (ConMed Linvatec, Largo, Fla) have resulted in failure of repair with loosening and/or incomplete resorption at 5, 7, 9, and 13 months, resulting in persistent knee pain (Fig. 5-13). In all cases, the remnants of the biodegradable material were removed, synovectomies were performed, and all patients responded favorably. Several authors have described synovitis and chondral lesions up to 13 months postoperatively. On removal of implants and following synovectomy, patients ultimately did well. Chondral injury was present in all cases.34–37 A case of the RapidLoc PLLA implant (DePuy Mitek, Raynham, Mass) loosening, resulting in chondral injury, was reported at 4 months postarthroscopy (Figs. 5-14 and 5-15). These patients most commonly present with mechanical symptoms at the time of device loosening.38 The FAST-Fix meniscal repair system (Smith & Nephew, Andover, Mass) can cause a meniscal cyst at subsequent implantation prior to resorption of the device.39 This was seen in one of the senior author’s ( JB) cases at 16 weeks postoperatively, with MRI confirming a meniscal cyst adjacent to a Fast-Fix meniscal repair device (Fig. 5-16).
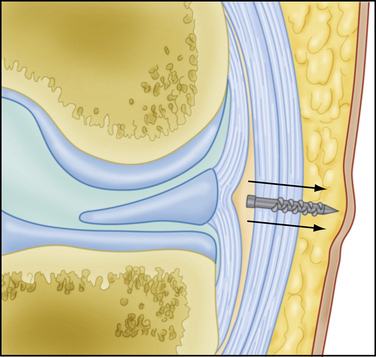
FIGURE 5-13 Posterior penetration of meniscal arrow, resulting in soft tissue irritation (arrows).
(Courtesy of Dr. Alan Barber.)
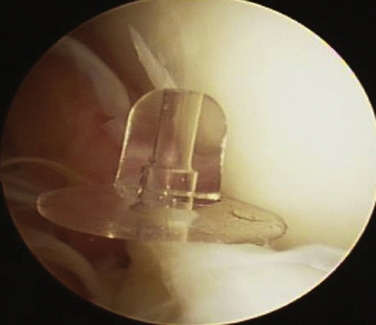
FIGURE 5-14 Dislodged RapidLoc fixation device (DePuy Mitek, Raynham, Mass).
(Courtesy of Dr. Alan Barber.)
Miscellaneous Complications
Miscellaneous complications include fluid extravasation as a result of arthroscopy pump or tubing failure. If the pump continues to run without an egress cannula in the joint, and the joint becomes taut with fluid, the pump should be immediately shut down or extravasation of fluid into the thigh (Fig. 5-17) can occur.40 Chronic synovitis after routine arthroscopy of the knee (Fig. 5-18) has been reported to be from 2% to 3%. Care must be taken not to overlook a postoperative infection. Treatment is prolonged oral anti-inflammatories or intra-articular steroid injections.41
PEARLS& PITFALLS
PEARLS
CONCLUSIONS
Clinical, technical, and material-related complications are still present during or subsequent to routine arthroscopic knee surgery. Phlebitis and pulmonary emboli continue to be reported and are difficult to predict without a previous medical history. Prophylactic anticoagulation for routine arthroscopic procedures remains controversial. Technical complications are still common, including nerve and vascular injuries, despite improvements in instrumentation. Material complications have increased as a result of increased use of biodegradable implants. Suture technique complications are decreasing because of increased use of biodegradable devices, but still occur. It is important for the knee arthroscopist to be continuously aware of possible complications, even during the most routine arthroscopic knee procedures. Special vigilance is needed for the patient with a medical history that indicates a propensity to venous thromboembolism. There should be a continued awareness of knee anatomy when using percutaneous guide wires and performing suture repair techniques to avoid vascular and nerve complication.
1. Bushnell B, Anz A, Bert J. Venous thromboembolism in lower extremity arthroscopy. Arthroscopy. 2008;24:604-611.
2. Hunter R, Sgaglione N, Carter T, Bert J. Treatment of articular cartilage injuries of the knee. Rosemount, Ill: Hunter R, Sgaglione N, Carter T, Bert J; September 9-10, 2006. Paper presented at: Orthopaedic Learning Center, Arthroscopy Association of North America Instructional Course
3. Williams J, Hulstyn M, Fadale P, et al. Incidence of deep vein thrombosis after arthroscopic knee surgery: a prospective study. Arthroscopy. 1995;11:701-705.
4. Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on antithrombotic and thrombolytic therapy. Chest. 2004;126:338-400.
5. Anderson FAJr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107:9-16.
6. Eynon AM, James S, Leach P. Thromboembolic events after arthroscopic knee surgery. Arthroscopy. 2004;20:23-24.
7. Wirth T, Schneider B, Misselwitz F, et al. Prevention of venous thromboembolism after knee arthroscopy with low-molecular weight heparin (reviparin): results of a randomized controlled trial. Arthroscopy. 2001;17:393-399.
8. Michot M, Conen D, Holtz D, et al. Prevention of deep-vein thrombosis in ambulatory arthroscopic knee surgery: a randomized trial of prophylaxis with low-molecular weight heparin. Arthroscopy. 2002;18:257-263.
9. Canale T. Wrong-site surgery: a preventable complication. Clin Orthop Relat Res. 2005;433:26-29.
10. Wong D. AAOS patient safety: tools for implementation. Paper presented at: AAHKS 14th Annual Meeting; November 5-7, 2004; Denver.
11. Meinberg EG, Stern PJ. Incidence of wrong-site surgery among hand surgeons. J Bone Joint Surg Am. 2003;85:193-197.
12. Albright D, McDaniel S. The incidence of wrong-site surgery in knee arthroscopy. Sidney, Australia: Albright D, McDaniel S; October 24-29, 2004. Paper presented at: Combined Meeting of Orthopaedic Associations
13. Minnesota Department of Health. Second Annual Public Report. Adverse Health Events in Minnesota; February 2006, Available at: http://www.health.state.mn.us/patientsafety/ae/aereport0206.pdf Accessed December 14, 2009.
14. DeLee J. Complications of arthroscopy and arthroscopic surgery: results of a national survey. Arthroscopy. 1985;1:214-220.
15. Johnson L. Two per cent glutaraldehyde: a disinfectant in arthroscopy and arthroscopic surgery. J Bone Joint Surg Am. 1982;64:237-239.
16. D’Angelo G, Ogilvie-Harris D. Septic arthritis following arthroscopy, with cost/benefit analysis of antibiotic prophylaxis. Arthroscopy. 1988;4:10-14.
17. Armstrong RW. Septic arthritis following arthroscopy: clinical syndromes and analysis of risk factors. Arthroscopy. 1992;8:213-223.
18. Bert J, Giannini D, Nace L. Antibiotic prophylaxis for arthroscopy of the knee: is it necessary. Arthroscopy. 2007;23:4-6.
19. Lubowitz J, Kurzweil P. Editorial response to antibiotic prophylaxis for arthroscopy of the knee. Arthroscopy. 2007;23:1-3.
20. Small, NC. Complications in arthroscopic meniscal surgery. Clin Sports Med. 1990;9:609-617.
21. Austin K, Sherman O. Complications of arthroscopic meniscal repair. Am J Sports Med. 1993;21:864-869.
22. Voloshin I, DeHaven KE, Steadman JR. Second-look arthroscopic observations after radiofrequency treatment of partial thickness articular cartilage defects in human knees: report of four cases. J Knee Surg. 2005;18:116-122.
23. Outerbridge R. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752-757.
24. Patel D, Bibbo C, Gupta M, Gehrmann R. Long-term results of arthroscopic partial medial meniscectomy in an otherwise normal knee. Chicago: Patel D, Bibbo C, Gupta M, Gehrmann R; March 22-26, 2006. Paper presented at: American Academy of Orthopaedic Surgeons Annual Meeting
25. Meredith DS, Losina E, Mahomed NN, et al. Factors predicting functional and radiographic outcomes after arthroscopic partial meniscectomy: a review of the literature. Arthroscopy. 2005;21:116-122.
26. Christoforakis J, Pradhan R, Sanchez-Ballester J, et al. Is there an association between articular cartilage changes and degenerative meniscus tears? Arthroscopy. 2005;21:1366-1369.
27. Kuraishi J, Akizuki S, Takizawa T, et al. Arthroscopic lateral menscectomy in knees with lateral compartment osteoarthritis: a case series study. Arthroscopy. 2006;22:878-883.
28. Alford JW, Cole BJ. Rapid progression of chondral disease in the lateral compartment of the knee following meniscectomy: a review of the literature and case reports. Arthroscopy. 2005;21:11-13.
29. Bert JM. Use of an electrocautery loop probe for arthroscopic meniscectomy: a five-year experience with results, indications, and complications. Arthroscopy. 1992;8:148-156.
30. Covall DJ, Wasilewski SA. Roentgenographic changes after arthroscopic meniscectomy: five-year follow-up in patients more than 45 years old. Arthroscopy. 1992;8:242-246.
31. Novak PJ, Wexler GM, Williams JSJr. Comparison of screw post fixation and free bone block interference fixation for anterior cruciate ligament soft tissue grafts: biomechanical considerations. Arthroscopy. 1996;12:470-473.
32. Junkin L, Johnson D. ACL tibial remnant, to save or not. Orthopedics. 2008;31:154-159.
33. Howell S, Gittens M, Gottlieb J, et al. The relationship between the angle of the tibial tunnel in the coronal plane and loss of flexion and anterior laxity after anterior cruciate ligament reconstruction. Am J Sports Med. 2001;29:567-574.
34. Asik M, Sener N. Failure strength of repair devices versus meniscus suturing techniques. Knee Surg Sports Traumatol Arthrosc. 2002;10:25-29.
35. Ross G, Grabill J, McDevitt E. Chondral injury after meniscal repair with bioabsorbable arrows. Arthroscopy. 2000;16:754-756.
36. Seil R, Rupp S, Dienst M, et al. Chondral lesions after arthroscopic meniscus repair using meniscus arrows. Arthroscopy. 2000;16:E17.
37. Song EK, Lee KB, Yoon TR. Aseptic synovitis after meniscal repair using the biodegradable meniscus arrow. Arthroscopy. 2001;17:77-80.
38. Cohen SB, Anderson MW, Miller MD. Chondral injury after arthroscopic meniscal repair using bioabsorbable Mitek RapidLoc meniscal fixation. Arthroscopy. 2003;19:24-26.
39. Lombardi JA. Second-look arthroscopy with removal of bio- absorbable tacks. Am J Orthop. 2000;29:125-127.
40. McGuire D, Hendricks S. Incidence of frostbite in arthroscopic knee surgery postoperative cryotherapy rehabilitation. Arthroscopy. 2006;22:1141.e1-1141.e6 Arthroscopy. 2002;10:25.
41. Rasmussen S, Lorentzen JS, Larsen AS, et al. Combined intra-articular glucocorticoid, bupivacaine and morphine reduces pain and convalescence after diagnostic knee arthroscopy. Acta Orthop Scand. 2002;73:175-178.