Chapter 18 Complications of Intraarticular Joint Injections and Musculoskeletal Injections
 There should be a constant awareness of potential complications from interventional pain procedures, and efforts to minimize these complications should be implemented.
There should be a constant awareness of potential complications from interventional pain procedures, and efforts to minimize these complications should be implemented.Introduction
Over recent years, interventional pain management has grown steadily. Consequently, the prevention of complications from interventional pain procedures should be a very important aspect of pain management. Although the true incidence is difficult to assess, it is extremely important to note and understand the potential risks and consequences. Appendicular intraarticular joint (hip, knee, shoulder, hand) and musculoskeletal injections are deemed some of the safest procedures performed in interventional pain management. The most common complications are infection, although septic arthritis, osteomyelitis, peripheral nerve injuries, pneumothorax, and skeletal muscle toxicity have all been reported (Table 18-1). The use of ultrasonography or fluoroscopy can assist in the visualization of nearby structures, thus decreasing the incidence of damage of these structures.
Table 18-1 Potential Complications and Avoidance at Each Site
| Joint | Problem | Avoidance |
|---|---|---|
| Hip joint |
Hip Joint Injections
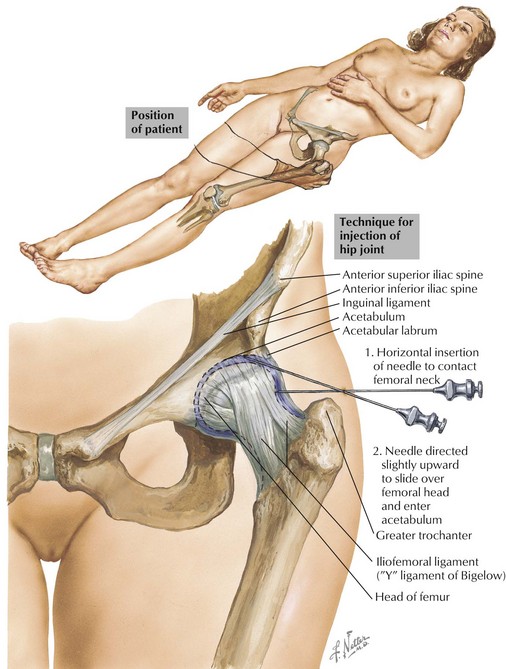
Hip injection is a common procedure to alleviate hip pain because this is a location commonly affected by osteoarthritis (Fig. 18-1). Complications are rare with hip joint injections with proper patient selection, proper sterile technique, and appropriate injection technique. As with other injections, potential complications include bleeding or bruising, infection, allergic reaction to injectate, and increased pain. Injury to the femoral neurovascular bundle is a theoretical complication using an anterior approach to the hip joint, although it has yet to be described. The use of ultrasonography would allow visualization of this neurovascular bundle and would decrease the possibility of injury. Cheng and Abdil1 (2007) describe air embolism in three pediatric patients undergoing hip injections. During arthrography, injections of a small amount of air can be used to outline the joint for correct needle placement. These injections were done with even small amounts of air (<5 mL). This has not been described in the adult population.
Greater trochanteric bursal injections are commonly given for bursitis-related hip pain. Necrotizing fasciitis has been reported in a case report in 2001 by Hofmeister and Engelhardt.2 Although this is an isolated incident, this soft tissue infection is limb and life threatening and ultimately resulted in death in this patient.
Glenohumeral Joint Injections
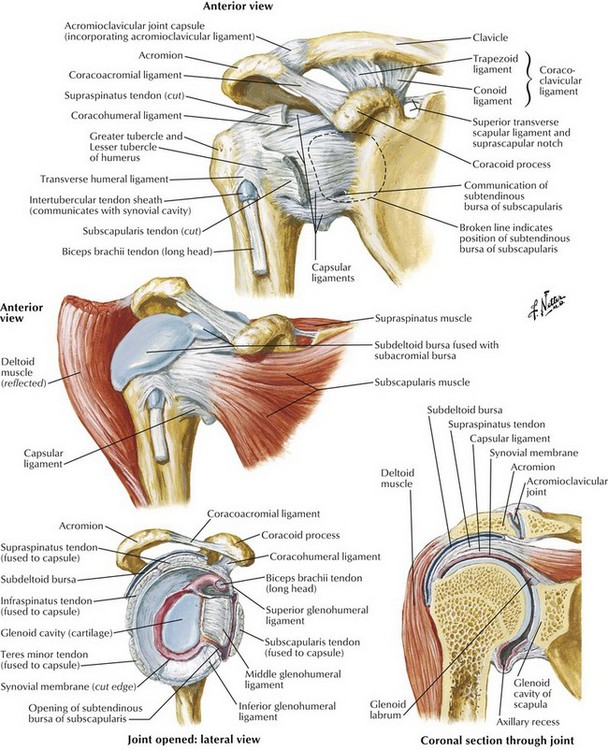
Subacromial and intraarticular injections (Fig. 18-2) are commonly provided for shoulder pain when other conservative therapies such as physical therapy, heat and ice, and over-the-counter antiinflammatory medications are not effective. With proper patients being selected (i.e., no active infection, no bleeding diathesis), using sterile technique, and performing proper injection technique, complications are extremely rare with glenohumeral joint injections. Injury to a neurovascular structure is a potential complication as well, but it should be minimized with proper preprocedure planning and proper technique. In addition, the use of ultrasonography may further minimize this complication.
Infection, although uncommon, is a significant complication. Meticulous adherence to sterile technique is emphasized for performing both subacromial and intraarticular shoulder injections. As in greater trochanteric bursal injection described earlier, necrotizing fasciitis has also been reported during an intraarticular shoulder injection.3 This patient recovered after extensive surgical debridement, aggressive resuscitative efforts, and intravenous antibiotics. A case of scapular osteomyelitis after subacromial corticosteroid injection has also been reported. Again, meticulous attention to sterile technique has been suggested.4
Knee Joint Injections
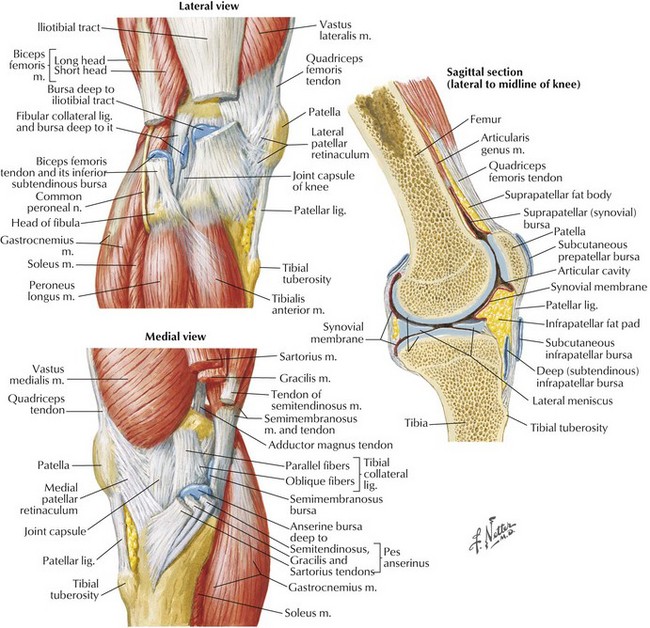
Pain at the site of injection has been noted to have the highest prevalence; it may occur in 20% of patients.5 However, severe local inflammation and development of joint effusion are rare.5 Granulomatous inflammation of the synovium was reported in six cases of hyaluronic acid–based injections in 2002.5
Although there is a theoretical risk of damage to neurovascular structures, there has been only one case of saphenous neuropathy after a medial approach to an intraarticular knee injection (Fig. 18-3).6
Septic arthritis has been reported in a few cases with different organisms, including Actinomyces naeslundii and Candida albicans.7–9 Aseptic acute arthritis has also been described in two cases.10
Trigger Point Injections
Trigger point injections are generally considered very safe. They are common procedures performed by many practitioners, including pain, primary care, and emergency department physicians. Even though they are considered very safe, serious complications can result. Some of these complications include pneumothorax, intrathecal injection, epidural abscess, and skeletal muscle toxicity.11–14 Of the 276 claims reported in the American Society of Anesthesiologists Closed Claims Project, 17 cases involved trigger point injections in which pneumothorax (15 of 17 cases) was the most common.15
Skeletal muscle toxicity is a rare and uncommon side effect of local anesthetics. In fact, intramuscular injections with any local anesthetic can result in reversible myonecrosis. Bupivacaine seems to be the most myotoxic, and procaine appears to be the least.14 In most cases, there is no sequela and muscle regeneration, and healing usually take 3 to 4 weeks.14
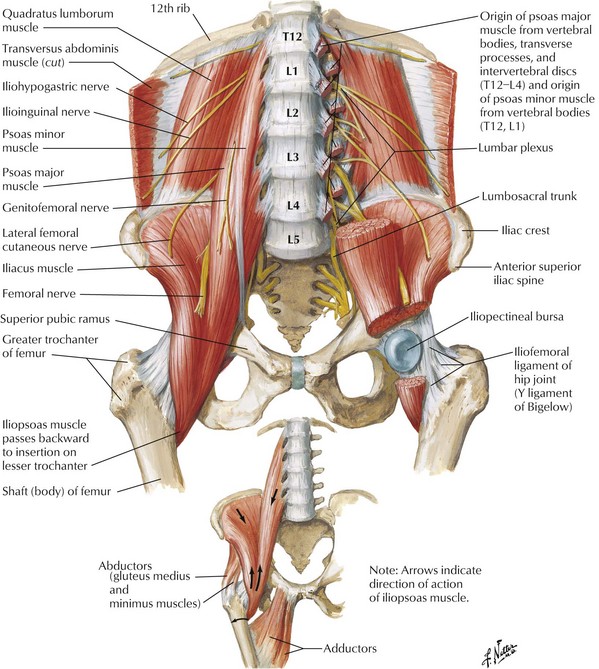
Regarding trigger point injections of the quadratus and iliopsoas muscles, there are particular points to mention given the proximity of vital nearby structures. As described before, the quadratus has its origin at the iliac crest and iliolumbar ligament and inserts around the 12th rib and the transverse processes of the lumbar vertebrae (Fig. 18-4). It is posterior to the kidney; thus injection should be done with this in mind because renal damage is a potential risk, although it has yet to be described. The iliopsoas muscle is lateral to the vertebral foramen and posterior to the lumbar sympathetic chain and the great vessels of the abdomen, so caution with needle depth is important.
1 Cheng J, Abdi S. Complications of joint, tendon, and muscle injections. Tech Reg Anesth Pain Manag. 2007;11(3):141-147.
2 Hofmeister E, Engelhardt S. Necrotizing fasciitis as complication of injection into greater trochanteric bursa. Am J Orthop. 2001;30:426-427.
3 Birkinshaw R, O’Donnell J, Sammy I. Necrotising fasciitis as a complication of steroid injection. J Accid Emerg Med. 1997;14:52-54.
4 Buckley SL, Alexander AH, Barrack RL. Scapular osteomyelitis. An unusual complication following subacromial corticosteroid injection. Orthop Rev. 1989;18:321-324.
5 Chen AL, Desai P, Adler EM, et al. Granulomatous inflammation after Hylan G-F 20 viscosupplementation of the knee: a report of six cases. J Bone Joint Surg. 2002;84-A(7):1142-1147.
6 Iizuka M, Yao R, Wainapel S. Saphenous nerve injury following medial knee joint injection: a case report. Arch Phys Med Rehabil. 2005;86:2062-2065.
7 Lequerre T, Nouvellon M, Kraznowska K, et al. Septic arthritis due to Actinomyces naeslundii: report of a case. Joint Bone Spine. 2002;69:499-501.
8 Evanich JD, Evanich CJ, Wright MB, et al. Efficacy of intraarticular hyaluronic acid injections in knee osteoarthritis. Clin Orthop Relat Res. 2001;390:173-181.
9 Christensson B, Ryd L, Dahlberg L, et al. Candida albicans arthritis in a nonimmunocompromised patient. Complication of placebo intraarticular injections. Acta Orthop Scand. 1993;64:695-698.
10 Charalambous CP, Tryfonidis M, Sadiq S, et al. Septic arthritis following intra-articular steroid injection of the knee—a survey of current practice regarding antiseptic technique used during intraarticular steroid injection of the knee. Clin Rheumatol. 2003;22:386-390.
11 Shafer N. Pneumothorax following “trigger point” injection. JAMA. 1970;213:1193.
12 Nelson LS, Hoffman RS. Intrathecal injection: unusual complication of trigger-point injection therapy. Ann Emerg Med. 1998;32:506-508.
13 Elias M. Cervical epidural abscess following trigger point injection. J Pain Sympt Manage. 1994;9:71-72.
14 Zink W, Graf BM. Local anesthetic myotoxicity. Reg Anesth Pain Med. 2004;29:333-340.
15 Fitzgibbon DR, Posner KL, Domino KB, et al. American Society of Anesthesiologists. Chronic pain management: American Society of Anesthesiologists Closed Claims Project. Anesthesiology. 2004;100:98-105.