CHAPTER 27 Complications of adjustable gastric banding
Step 1. Surgical anatomy
♦ Band complications can occur early or late. The most common late complications are port or tubing problems (2% to 3%), band slippage (3% to 6%), and band erosion (0.5% to 1%). We will concentrate on band slippage and band erosion in this chapter.
♦ In revisional operations, caution should be paid to the left gastric artery, or an aberrant left hepatic artery arising from the left gastric. These relatively large vessels can be obscured by a dense inflammatory reaction and may be unrecognized when dissecting to the left of the stomach and band buckle.
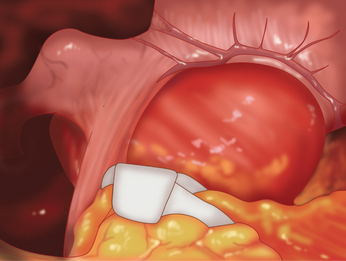
♦ The operative treatment of band slippage involves laparoscopic reduction of the herniated stomach, with band replacement or repositioning. This is usually possible via a laparoscopic approach. Contrast swallow shows an eccentric pouch enlargement above the band and that the angle of the band to the vertical is greater than 90 degrees (Figure 27-1 and 27-2).
♦ A hiatal hernia is commonly found in association with a band slip and should be repaired at the time of revisional surgery. Exploration reveals a dilated, eccentric gastric pouch above the band (Figure 27-2).
Step 2. Preoperative considerations
Patient preparation
♦ The modern technique of band placement is the pars flaccida approach, favored because of a decreased incidence of posterior band slippage. There is minimal posterior dissection at the level of the confluence of the left and right diaphragmatic crura. The posterior position of the band is at or just below the esophagogastric junction. Anteriorly a small (15 mL) virtual pouch is created.
♦ All patients should have a reassessment of their comorbidities and nutritional state before undergoing revisional bariatric surgery. Patients may develop anemia after band slippage secondary to erosive gastritis in the dilated pouch.
♦ Diagnosis and anatomy should be well defined preoperatively; the investigation of choice for band slip is a contrast swallow, and for band erosion it is an upper endoscopy.
Step 3. Operative steps
Access and port placement
♦ Trocar placement is similar to primary laparoscopic adjustable gastric banding.
♦ Care should be taken to avoid the existing access port, which can be retained for use with the new band.
For band slippage
♦ Initial dissection using cautery should proceed along the band tubing with sequential division of biomembrane until the band is reached.
♦ The band must be dissected away from biomembrane, adhesions, and the left lateral section of the liver until the buckle is free.
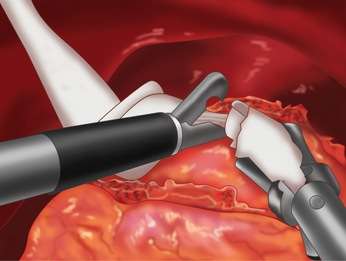
♦ After the buckle of the band is free, the band may be cut with hook scissors (Figure 27-3). Retaining the band for use as a retractor during some of the remaining dissection may also be useful.
♦ The previous tunnel formed by the gastro-gastric sutures is usually taken down. This can be achieved through careful dissection using laparoscopic scissors. If the dissection plane is not clear, a linear cutting stapler may be used to avoid inadvertent gastrotomy.
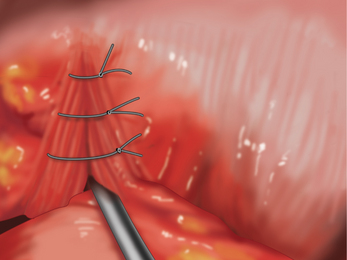
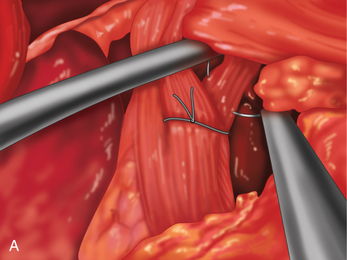
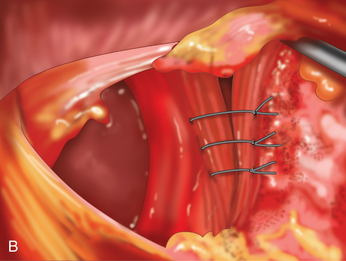
♦ Crural defects should be repaired prior to placement of a new band. I close anteriorly (Figure 27-4) or posteriorly (Figures 27-5A and 27-5B), and sometimes both, wherever I find the gap.
♦ We then replace the band using a new adjustable gastric band placed via the pars flaccida technique posteriorly and in a higher position anteriorly.
♦ Gastro-gastric sutures are placed between fundus and gastric pouch anteriorly to prevent reslip. Occasionally I will omit sutures on revisions as they place too much tension.
♦ An EndoCatch (Covidien, Mansfield, Massachusetts) bag facilitates removal of the old band.
♦ The tip of the tubing of the new band is brought out and spliced to the existing access port extracorporeally using a metal connector that comes with the new band.
For band erosion
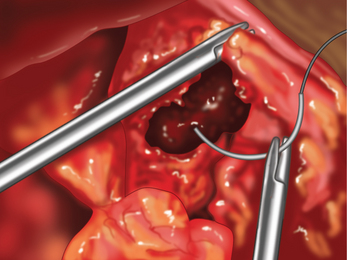
♦ An adjustable gastric band can be seen with a retroflexed endoscope. It is eroding into stomach lumen (Figure 27-6).
♦ The treatment of band erosion involves band removal, via an endoscopic, or laparoscopic approach, along with closure of the gastric perforation. We favor the latter technique as it facilitates the gastric repair.
♦ Patient positioning and trocar placement is as for band slippage.
♦ Initial dissection is with electrocautery, using the tubing to identify the position of the band if possible.
♦ The buckle of the band is dissected free, and the band is cut with hook scissors.
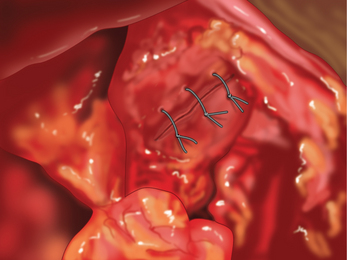
♦ The band is then removed, and the gastric perforation then repaired using laparoscopically placed sutures in two layers (Figures 27-7 and 27-8).
♦ Gastric integrity is tested using methylene blue dye, and fibrin glue is applied.
♦ A closed low suction drain is sometimes placed adjacent to the gastrotomy closure.
Step 4. Postoperative care
♦ Band repositioning or replacement is usually done as an outpatient procedure,whereas band removal for erosion may spend a night.
♦ We usually admit patients to the ward for overnight observation following revisional laparoscopic adjustable gastric band surgery.
♦ Patients are usually kept NPO until after a water soluble contrast swallow on postoperative day.
♦ Oral fluids are then commenced at a rate of 30 mL every 15 minutes.
♦ Patients are discharged when they can tolerate 240 mL of fluid orally over a period of 2 hours.
♦ Patients follow a liquid diet for 2 weeks and a puree diet for 2 weeks. The first band adjustment is usually performed at 4 weeks after the operation.
♦ For band erosion, further revisional surgery is considered after full recovery from band removal. Options include re-gastric banding, Roux-en-Y gastric bypass, and sleeve gastrectomy.
Step 5. Pearls and pitfalls
♦ In an erosion, because of the dense inflammatory reaction, the tubing may not be visible; if this is the case, then dissection should start underneath the left lateral section of the liver. The tubing will be found adherent to the liver in this location and may then be followed to the band.
♦ When dense adhesions make dissecting out an eroded gastric band extremely hazardous, an alternative approach is to remove it transgastrically via a distal gastrotomy, as long as the buckle is within the stomach. A combined laparoscopic/endoscopic approach is also possible in this situation.
♦ Care should be taken to avoid an accessory left hepatic artery running in the gastrohepatic omentum when dissecting out the gastric band. This is especially true for band erosion.
♦ It is important to repair any hiatal hernia or crural weakness found in association with a band slip. This can be repaired using sutures placed anterior or posterior to the esophagus.
♦ When replacing a gastric band after a slip, sutures from the greater curve to the lesser curve below the band, imbricating the redundant fundus, may help to prevent reslippage.
♦ When further revisional surgery is contemplated, such as after band erosion, adhesion prevention barriers, such as SurgiWrap (Mast Biosurgery, Zurich, Switzerland), will facilitate subsequent dissections.
Chevallier JM, Zinzindohoue F, Douard R, et al. Complications after laparoscopic adjustable gastric banding for morbid obesity: experience with 1,000 patients over 7 years. Obes Surg. 2004;14;3:407-414.
Cunneen SA, Phillips E, Fielding G, et al. Studies of Swedish adjustable gastric band and Lap-Band: systematic review and meta-analysis. Surg Obes Relat Dis. 2008;4;2:174-185.
Mehanna MJ, Birjawi G, Moukaddam HA, et al. Complications of adjustable gastric banding, a radiological pictorial review. AJR Am J Roentgenol. 2006;186(2):522-534.
Ponce J, Fromm R, Paynter S, et al. Outcomes after laparoscopic adjustable gastric band repositioning for slippage or pouch dilation. Surg Obes Relat Dis. 2006;2(6):627-631.