CHAPTER 29 Complex Instability of the Elbow
INTRODUCTION
Since the first edition of this book, improvements in the recognition and treatment of complex instability are among the most significant developments in managing elbow trauma. The coexistence of multiple articular and soft tissue injuries is being increasingly appreciated.9,42
DEFINITION
Complex instability of the elbow is defined as an injury that destabilizes the elbow because of damage to the articular surface and to the ligamentous structures.21 Others add soft tissue involvement, including neural and vascular injuries in the diagnosis.36 However, vascular injuries are uncommon in this setting. Over a 10-year period, for example, Moneim and Garst20 documented only two instances of vascular injury among 56 with fracture dislocation injury. The clinical presentation is usually one in which the instability is obvious, but more subtle forms are being recognized.39 In this chapter, the relative contributions of the articulation and the ligaments to normal stability, as well as to their interactions, are first defined. We then offer a rationale for the reliable treatment of a spectrum of these acute injuries.
CONTRIBUTIONS TO NORMAL STABILITY
ARTICULAR ELEMENTS
Although the distal humerus is sometimes involved, for the purpose of this discussion, it is assumed that the distal humerus is intact. Therefore, the articular elements to be considered are the radial head, olecranon, and coronoid. The relative role of these elements to elbow stability have been recently reviewed.27
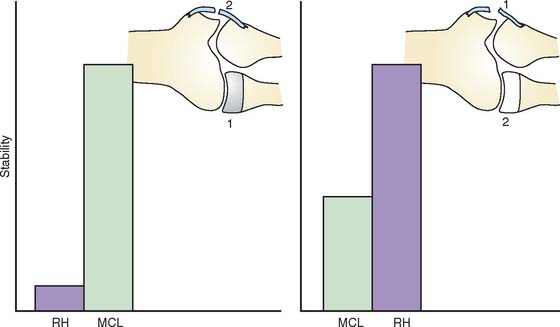
Radial Head
It is known clinically that the radial head may be resected without altering the stability of the otherwise normal elbow.27 Therefore, the contribution of the radiohumeral joint to elbow stability is intimately related to and dependent on the integrity of the collateral ligaments. Experimental data have clearly documented that the resistance to valgus stress provided by the radial head is minimal when the medial collateral ligament is intact24,25,40 (Fig. 29-1). However, the radiohumeral joint offers enough resistance to valgus stress to prevent subluxation if the medial collateral ligament is attenuated or torn. The major structure resisting initial valgus displacement, even with an intact radial head, is the medial collateral ligament. If the medial collateral ligament is intact, the radial head offers little resistance to valgus stress, but if the medial collateral ligament is attenuated or torn, the radial head assumes the role of an important stabilizer. Thus, the radial head is an important secondary stabilizer to valgus stability.
The relationship of the radial head to the ulnar part of the lateral collateral ligament has been initially defined experimentally by O’Driscoll and associates.30,32 Today, posterolateral rotatory instability is well recognized to be associated with lateral ulnar collateral deficiency5,19,33 and can occur in the presence or absence of the radial head. However, clinical experience suggests that elbows without a radial head do less well after reconstruction of the ulnar part of the lateral collateral ligament than do those in which the radial head is intact.2,29 This provides further evidence of the important role of the radial head to resist posterolateral rotatory instability but, once again, in a secondary capacity.
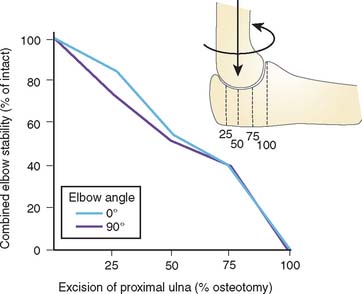
Olecranon
The major determinant of stability of the elbow is clearly the ulnohumeral joint, specifically the coronoid. Although the stabilizing influence of this joint has not been studied to any great extent, the relative contribution of the olecranon in resisting various loading configurations has been shown to be linearly correlated with the extent of resection of the proximal part of the ulna (Fig. 29-2).1 The critical amount of articulation required for maintaining stability is about 50%. These data may be altered by dynamic forces, but this has not been studied.
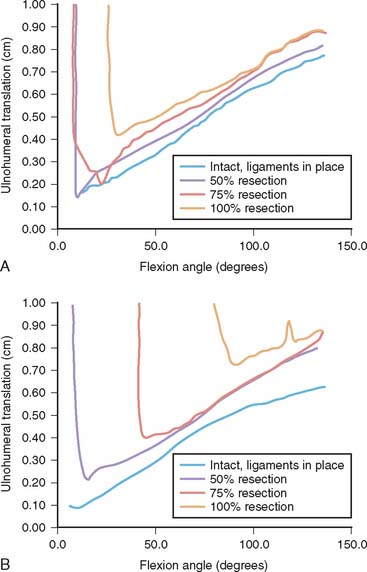
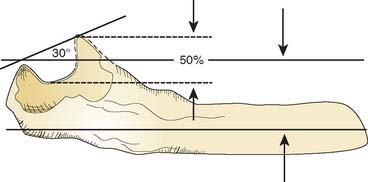
Coronoid
The amount of the coronoid required for stability with or without ligamentous integrity and with and without the radial head is just now emerging. Experimental and clinical experience suggests that at least 50% of the coronoid must be present for the ulnohumeral joint to be functional (Fig. 29-3). Absence of the radial head further and dramatically compromises the elbow with a 50% coronoid deficiency. From a practical perspective, we have found it useful to observe that the typical 30-degree angle formed by a line from the intact olecranon and coronoid is reduced to 0 degrees when the critical50% of the coronoid is present (Fig. 29-4). Anatomically and clinically, the coronoid is the subject of intense investigation to better understand fracture patterns, and the “critical portion” needed for stability.4
LIGAMENTOUS CONTRIBUTIONS
The relative contributions of the medial and lateral collateral ligaments to varus-valgus stability with the elbow articulation intact and in flexion and extension have been studied experimentally.23 This investigation has shown that the collateral ligaments provide approximately 50% of the varus-valgus stability of the joint, and the articular surfaces provide an additional 50%. The only exception is with the elbow in full extension: under this condition, the ulnohumeral joint and anterior capsule render the elbow stable to varus-valgus stress, even in the absence of collateral ligaments. The role of the ligaments in conjunction with the articulation is described earlier.
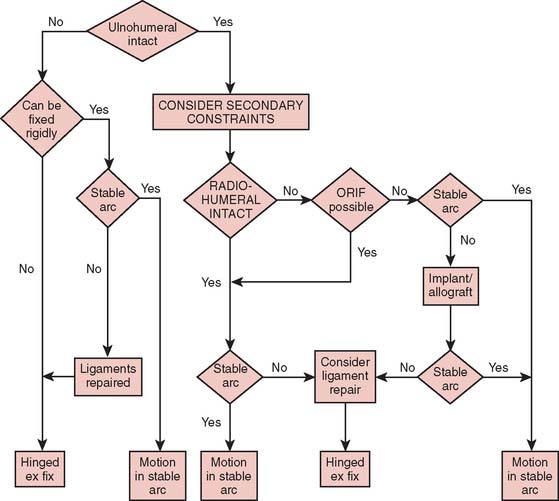
CLINICAL MANAGEMENT: PRINCIPLE
A basic principle underlying the treatment of complex instability is simply that a competent ulnohumeral jointbe attained and maintained.21,31 This is the primary overriding principle.
FRACTURE OF THE RADIAL HEAD WITH ATTENUATION OR TEAR OF THE MEDIAL COLLATERAL LIGAMENT
The presentation of medial ligament injury can be extremely subtle. The prevalence is difficult to ascertain, but in my experience, as an isolated lesion, it has occurred only in about 1% to 2% of patients who had a fracture of the radial head.22 One should have a highlevel of suspicion that an injury to the ligament might be present when there is a compression fracture with or without comminution of the radial neck. Ecchymosis on the medial side of the elbow should be an obvious clue but is often absent.
Treatment
Treatment of this difficult structured problem is based on the realization that the medial collateral ligament tends to heal if the ulnohumeral joint is reduced. Furthermore, the radial head is an important secondary stabilizer to valgus stress when the medial collateral ligament has been disrupted. The primary goal of the treatment strategy is to restore ulnohumeral joint stability. However, a reconstructed medial collateral ligament has been observed to stretch in the absence of radial humeral integrity; hence, if it is amenable to fixation, the fracture is fixed; if not, the head is replaced. If the arc is stable within 40 degrees of extension, unrestricted passive motion is allowed after 7 to 10 days of protection. If dislocation occurs with extension of approximately 60 degrees, the elbow is immobilized for 10 days, after which motion in a Mayo Elbow Brace with a 45-degree extension stop, is allowed for 2 weeks. In our practice, the collateral ligament need not be repaired in those with a stable ulnohumeral, radiohumeral joint. Nonetheless, the popularity of suture anchors has prompted a more aggressive attitude toward ligament repair. Rodgers and colleagues38 report 88% satisfactory results in 17 patients treated with suture anchors who had major elbow injuries.
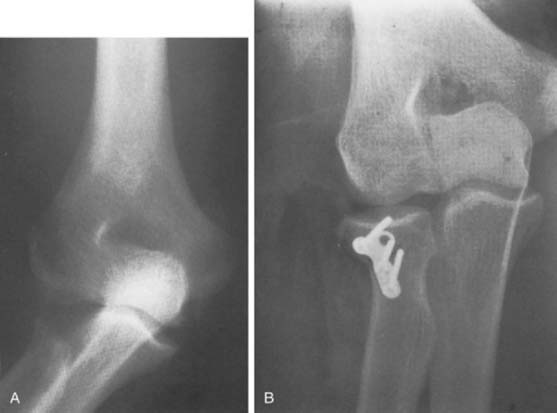
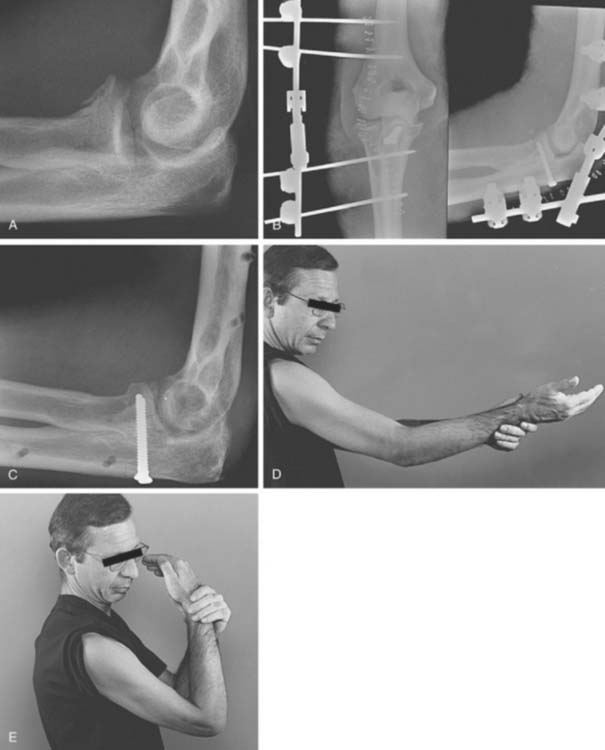
If osteosynthesis is not possible, then restoration of the radiohumeral joint with the use of a prosthesis becomes a higher priority. Prostheses of today are considerably more effective than in the past. Therefore, the possibility of use of metal implants has been reintroduced.7,12,15 In some instances in which the medial collateral ligament has been disrupted, replacement of the radial head with an allograft has been performed as an alternative method of providing stabilization (Fig. 29-5A and B).
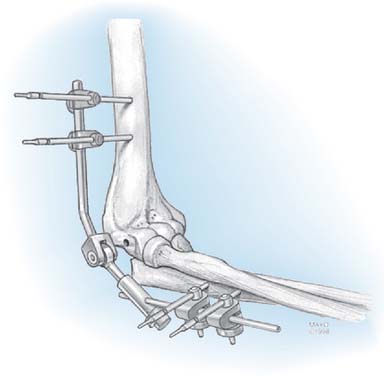
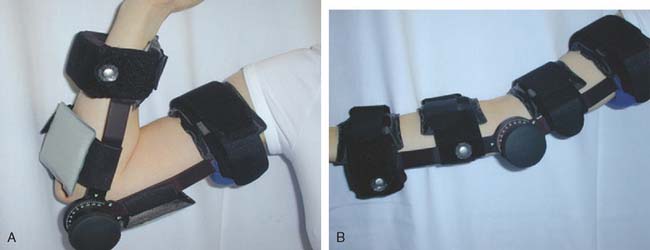
Finally, a hinged external fixator is applied in those circumstances in which it is desirable to protect a fractured radial head, the coronoid, or to protect a ligament repair (see Chapter 33).3,13,17 There are several articulated fixators available, but for this indication, Kamineni has shown that the simple half-pin configuration of the Dynamic Joint Distractor (DJDII) (Stryker, Mahwah, NJ) is effective to stabilize the joint even in the absence of both collateral ligaments. Hence, because of cost and simplicity, this is our choice of devices (Fig. 29-6).13 If the fixator is not used, patients are fitted with the Mayo Brace in the locked mode for protection for about 2 weeks postoperatively; the brace is then unlocked, and motion is allowed in the brace through the stable arc. The hinged brace is worn for a total of at least 6 weeks or until the joint is considered stable.
FRACTURES OF THE RADIAL HEAD WITH DISLOCATION OF THE ELBOW
This lesion is often referred to as a Mason type IV injury, an extension of the original Mason classification of fractures10,27 (see Chapter 24). This association was observed in 59 of the 333 radial head fractures assessed for associated injuries.42 The simple principle defined earlier continues to be relevant. If it is clearly demonstrated that the coronoid is intact, the basic treatment principle is first to reduce the dislocation and then to determine the extent to which the ulnohumeral articulation is inherently stable. Treatment of the radial head is determined according to the type of fracture.27
Type II Fractures
Type II fractures are treated by open reduction and internal fixation. These injuries are the most amenable to such treatment. King and associates14 report a successful outcome in all eight patients so treated. It isessential that elbows with injuries of the collateral ligaments be treated with open reduction and internal fixation, because these injuries result in chronic instability if the radial head is resected.6,7,12,37 Because these fractures are amenable to such treatment, repair of the medial collateral ligament to a great extent becomes personal preference. One of us (BFM) rarely fixes this ligament, whereas the other author (SOD) is more aggressive in this regard. However, if the elbow remains unstable on examination through the arcs described earlier, enhanced stability is obtained by repairing or stabilizing the medial collateral ligament. Josefsson and associates11 reviewed their experience with 19 complex injuries of the elbow and recommended open reduction and internal fixation of the radial head fracture as well as repair of the medial ligament. However, treatment of 4 of 19 coronoid fractures had a poor result, suggesting that this component of the lesion must be specifically addressed. Without question, the lateral ulnar collateral ligament must be formally and securely fixed.
If uncertainty as to stability still exists, we then resort to the use of the external fixator.
Type III Fractures
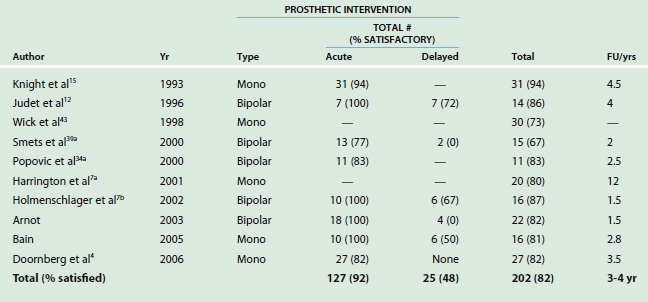
These are the most difficult injuries to treat. Experience has suggested that the entire comminuted radial head should be excised acutely if it cannot be fixed.2 Open reduction and internal fixation is technically difficult and was reported to be successful in only two of six instances by King and colleagues.14 We now know those fractures with more than four fragments should be excised, not fixed. A prosthesis is then used and is considered an essential component of the treatment. A review of the literature regarding treatment with several metallic radial head implants reveal an overall success rate of about 90% when managed acutely (Table 29-1). The elbow is tested according to the scheme described for type I fractures. If the elbow is unstable, then direct repair of the medial collateral ligament might be considered.
If stability remains a problem, a hinged external fixator that allows elbow motion is applied. The indication for use of the external fixator is a joint with a healing radial head with a torn medial collateral ligament that remains unstable (see Chapter 33). If use of an implant or open reduction and internal fixation of the radial head does not restore stability, the distraction device allows congruous alignment of the ulnohumeral joint, allowing motion which lessens the likelihood of stiffness or of fracture displacement. The device is removed as early as the third to fourth week and as late as 12 weeks, after which adjustable splints are used to restore motion (see Chapter 12).
FRACTURE OF THE PROXIMAL PART OF THE ULNA
Fractures of the proximal part of the ulna, both the olecranon or coronoid, pose major treatment problems.22 As always, management consists of restoring the integrity of the ulnohumeral joint, as just described. Ideally, this is accomplished by reduction and stabilization of the fracture.
FRACTURE OF THE OLECRANON
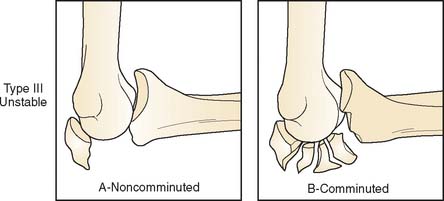
The Mayo classification scheme for fractures of the olecranon is based on displacement, comminution, and stability22 (see Chapter 25). The injury discussed here is termed type III, meaning that the elbow is unstable because of injury both to a collateral ligament and from a displaced fracture of the olecranon (Fig. 29-7). In fact, some might appropriately consider this a Monteggia variant9 and others have referred to this as a transolecranon anterior fracture dislocation.28,37
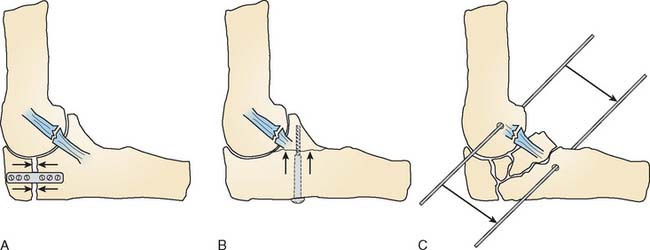
The type III fracture of the olecranon is accompanied by ligamentous disruption. The principle is again applied: stabilize the ulnohumeral joint (Fig. 29-8). If there is minimum comminution of the olecranon, rigid plate fixation restores the ulnohumeral joint. If the olecranon is rigidly fixed, then the unstable injury is converted to a stable one because the ulnohumeral joint is inherently stable. Hence, the technique for rigid fixation of the fracture is of paramount importance (see Fig. 29-8). A 3.5-mm dynamic compression or low-contour dynamic compression plate bent at an 80-degree angle or precontoured plate applied to the posterior surface of the ulna permits excellent fixation on the small proximal fragment.32 Commonly, one fragment may also involve the coronoid. If it does, this is the most important component of the reduction and fixation. If these principles are followed, a success rate of 88% has been reported in series of 828 and 15 patients.37
FRACTURE OF THE CORONOID
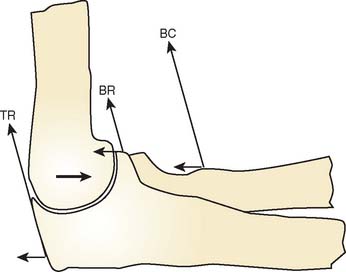
Without question, the coronoid is the most important portion of the ulnohumeral articulation. This is related to the posteriorly directed forces of both the biceps and the triceps that tend to “drive” the humerus into the coronoid fracture (Fig. 29-9). The base also serves as a site of attachment for the collateral ligaments.
Type I Fracture
According to the classification of Regan and Morrey, type I fractures represent a small chip of the tip of the coronoid and serve mainly as an indicator that the elbow has dislocated or at least displaced sufficiently to have sustained an injury of the collateral ligaments.35 The ulnohumeral joint is stable, and rehabilitation is similar to that recommended for type I fracture-dislocations of the radial head. Open reduction is not necessary if the elbow is stable. Occasionally, the fragment will become symptomatic as a snapping or catching requiring arthroscopic removal.16
Type II Fracture
In type II fractures, as much as 50% of the coronoid is involved and the elbow is usually unstable, especially if the radial head is also fractured. Careful examination with the patient under anesthesia reveals whether the joint is stable after reduction (Fig. 29-10). The threshold for fixation varies with individual surgeons but we are aggressive with any hint of instability. If the reduction is stable, motion within the stable arc, as described previously, may be allowed (see Fig. 29-10). If posterior displacement occurs with less than 40 to 45 degrees of flexion, the articulation is considered inadequate, and the ulnohumeral joint must be stabilized. If the fracture fragment is large enough for fixation, osteosynthesis with a single screw is performed. We approach the fracture laterally if the radial head is to be removed and medially if the head is intact. If the fragment is too small for fixation, a heavy No. 5 suture is placed through the fragment (or fragments), which is brought to its anatomic location and tied through drill holes placed in the ulna. In the latter situation, or even if osteosynthesis has been carried out but there is concern about stability, the elbow may need to be neutralized by the application of a hinged external fixatora-as the external fixator eliminates the dynamic forces that are applied to the fracture site by the muscles that flex and extend the elbow joint (Fig. 29-11). The device allows motion of the ulnohumeral joint while a distraction force is placed on the ulna, thus protecting the articulation. The device is maintained for 3 to 6 weeks, depending on the nature of the injury.3 Cobb and Morrey3 reported on seven such injuries and documented a successful outcome in six. In that series, the coronoid fracture was treated as described earlier, and a distraction device was applied in each instance.
Type III Fracture
These injuries are the most difficult to treat because, by definition, they render the ulnohumeral joint grossly unstable. If the coronoid is a large fragment and has notbeen comminuted (type IIIA), it may be fixed with one or two screws and the joint will be stable. However, because of the large forces transmitted through this relatively small surface area, as with the type II fractures, these injuries may be further neutralized with the distraction device. Jeon and colleagues8 highlighted the difficulty in the management in eight patients with this fracture.
The severely comminuted coronoid fracture (type IIIB) is a very difficult injury. In this setting, I reduce the elbow and bring the fracture fragments into relative alignment with the use of a heavy suture or a buttress plate is employed if the fracture pattern is amenable to this type of stabilization. I avoid removing any bone fragments because they may serve as a basis for substantive healing and formation of callus. The ulnohumeral relationship is maintained in a reduced position by the distraction device (Fig. 29-12).
In every instance, the most important goal is to prevent posterior displacement of the ulna against the trochlea—thus, the concept of neutralization with an external fixator that permits flexion and extension while keeping the articulation aligned and eliminating the disruptive force from muscle contracture (see Fig. 29-12). The principle of restoration and maintenance of the ulnohumeral integrity has been followed. After the fixator is removed, we typically use a hinged brace, which further protects the collateral ligaments for an additional 4 to 8 weeks (Fig. 29-13).
Fracture of the Radial Head and Coronoid with Dislocation
These injuries, termed the unhappy triad, are the most difficult to treat. The principle is the same as already discussed: the radial head must be fixed or replaced. The coronoid fracture is fixed, if possible, with use of a direct or retrograde or posigrade screw. In either instance, the elbow may need to be protected by a hinged external fixator. This allows motion but eliminates force on the radial head and the coronoid. Once again, the lateral ligament is always fixed. We typically use a No. 5 absorbable running locked stitch.18
OVERVIEW OF PRINCIPLES
TREATMENT
These basic principles of management are becoming well accepted.
1 An K.N., Morrey B.F., Chao E.Y.S. The effect of partial removal of proximal ulna on elbow constraint. Clin. Orthop. Relat. Res. 1986;209:270.
2 Broberg M.A., Morrey B.F. Results of treatment of fracture-dislocations of the elbow. Clin. Orthop. Relat. Res. 1987;216:109.
3 Cobb T.K., Morrey B.F. Use of distraction arthroplasty in unstable fracture dislocations of the elbow. Clin. Orthop. Relat. Res. 1995;312:201.
4 Doornberg J.N., van Duijn J., Ring D. Coronoid fracture height in terrible-triad injuries. J. Hand Surg. 2006;31:794.
5 Dunning C.E., Zarzour Z.D., Patterson S.D., Johnson J.A., King G.J. Ligamenotus stabilizers against posterolateral rotatory instability of the elbow. J. Bone Joint Surg. 2001;83:1823.
6 Geel C.W., Palmer A.K., Ruedi T., Leutenegger A.F. Internal fixation of proximal radial head fractures. J. Orthop. Trauma. 1990;4:270.
7 Harrington I.J., Tountas A.A. Replacement of the radial head in the treatment of unstable elbow fractures. Injury. 1981;12:405.
7a Harrington I.J., Sekyi-Out A., Barrington T.W., Evans D.C., Tuli V. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: A long-term review. J. Trauma. 2001;50:46.
7b Holmenschlager F., Halm J.P., Winckler S. Les fractures fraîches de la tête radiale. Résultants de la prothèse à cupule flottant de Judet. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2002;88:387.
8 Jeon I.H., Oh C.W., Kyung H.S., Park B.C., Kim P.T., Ihn J.C. Functional outcome after operative treatment of eight type III coronoid process fractures. J. Trauma. 2005;59:418.
9 Jepegnanam T.S. Salvage of the radial head in chronic adult Monteggia fractures. Report of four cases. J. Bone Joint Surg. 2006;88:645.
10 Johnston G.W. A follow-up of 100 cases of fracture of the head of the radius with a review of the literature. Ulster Med. J. 1962;31:51.
11 Josefsson P.O., Gentz C.F., Johnell O., Wendeberg B. Dislocations of the elbow and intraarticular fractures. Clin. Orthop. 1989;246:126.
12 Judet T., de Loubresse C.G., Piriou P., Charnley G. A floating prosthesis for radial-head fractures. J. Bone Joint Surg. 1996;78B:244.
13 Kamineni S., Hirahara H., Neale P., O’Driscoll S.W., An K.N., Morrey B.F. Effectiveness of the lateral unilateral dynamic external fixator after elbow ligament injury. J. Bone Joint Surg. 2007;89A:1802.
14 King G.J., Evans D.C., Kellam J.F. Open reduction and internal fixation of radial head fractures. J. Orthop. Trauma. 1991;5:21.
15 Knight D.J., Rymaszewski L.A., Amis A.A., Miller J.H. Primary replacement of the fractured radial head with a metal prosthesis. J. Bone Joint Surg. 1993;75-B:572.
16 Liu S.H., Henry M., Bowen R. Complications of type I coronoid fractures in competitive athletes: report of two cases and review of the literature. J. Shoulder Elbow Surg. 1996;5:223.
17 McKee M.D., Bowden S.H., King G.J., Patterson S.D., Jupiter J.B., Bamberger H.B., Paksima N. Management of recurrent, complex instability of the elbow with a hinged external fixator. J. Bone Joint Surg. 1998;80B:1031.
18 McKee M.D., Pugh D.M., Wild L.M., Schemitsch E.H., King G.J. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Surgical Technique. J. Bone Joint Surg. 2005;87A(suppl 1, Pt 1):22.
19 Mehta J.A., Bain G.I. Posterolateral rotatory instability of the elbow. J. Am. Acad. Orthop. Surg. 2004;12:405.
20 Moneim M.S., Garst J.R. Vascular injuries associated with elbow fractures and dislocations. Int. Angiol. 1995;14:307.
21 Morrey B.F. Complex instability of the elbow. J. Bone Joint Surg. 1997;79A:460.
22 Morrey B.F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid: Instructional Course Lecture. J. Bone Joint Surg. 1995;77-A:316.
23 Morrey B.F. Fracture of the radial head. In: Morrey B.F., editor. The Elbow and Its Disorders. 2nd ed. Philadelphia: W. B. Saunders; 1993:383.
24 Morrey B.F., Tanaka S., An K.-N. Valgus stability of the elbow: A definition of primary and secondary constraints. Clin. Orthop. 1991;265:187.
25 Morrey B.F. Acute and chronic instability of the elbow. J. Am. Acad. Orthop. Surg. 1996;4:117.
26 Morrey B.F., An K.-N. Articular and ligamentous contributions to the stability of the elbow joint. Am. J. Sports Med. 1983;11:315.
27 Morrey B.F., An K.N. Stability of the elbow: Osseous constraints. J. Shoulder Elbow Surg. 2005;14(1 suppl S):174S.
28 Mortazavi S.M., Asadollahi S., Tahririan M.A. Functional outcome following treatment of transolecranon fracture-dislocation of the elbow. Injury. 2006;37:284.
29 Nestor B.J., O’Driscoll S.W., Morrey B.F. Ligamentous reconstruction for posterolateral rotatory instability of the elbow. J. Bone Joint Surg. 1992;74A(8):1235.
30 O’Driscoll S.W. Technique for unstable olecranon fracture-subluxations. Op Techniques Orthop. 1994;4:49.
31 O’Driscoll S.W., Jupiter J.B., King G.J., Hotchkiss R.N., Morrey B.F. The unstable elbow. Instr. Course Lect. 2001;50:892.
32 O’Driscoll S.W., Morrey B.F., Korinek S., An K.N. Elbow subluxation and dislocation. Clin. Orthop. Relat. Res. 1992;280:186.
33 Olsen B.S., Vaesel M.T., Sojberg J.O., Helmig P., Sneppen O. Lateral collateral ligament of the elbow joint: Anatomy and kinematics. J. Shoulder Elbow Surg. 1996;5(2 pt 1):103.
34 Papandrea R.F., Morrey B.F., O’Driscoll S.W. Reconstruction for persistent instability of the elbow after coronoid fracture-dislocation. J. Shoulder Elbow Surg. 2007;16:68.
34a Popovic N., Gillet P., Rodriguez A., Lemaire R. Fracture of the radial head with associated elbow dislocation: Results of treatment using a floating radial head prosthesis. J. Orthop. Trauma. 2000;14:171.
35 Regan W., Morrey B.F. Fracture of the coronoid process of the ulna. J. Bone Joint Surg. 1989;71-A:1348.
36 Regel G., Seekamp A., Blauth M., Klemme R., Kuhn K., Tscherne H. Complex injury of the elbow joint. Unfallchirurg. 1996;99:92.
37 Ring D., Jupiter J.B., Sanders R.W., Mast J., Simpson N.S. Transolecranon fracture-dislocation of the elbow. J. Orthop. Trauma. 1997;11:545.
38 Rodgers W.B., Kharrazi F.D., Waters P.M., Kennedy J.G., McKee M.D., Lhowe D.W. The use of osseous suture anchors in the treatment of severe, complicated elbow dislocations. Am. J. Orthop. 1996;25:794.
39 Sanchez-Sotelo J., O’Driscoll S.W., Morrey B.F. Medial oblique compression fracture of the coronoid process of the ulna. J. Shoulder Elbow Surg. 2005;14:60.
39a Smets S., Govaers K., Jansen N., van Riet R., Schaap M., Van Glabbeek F. The floating radial head prosthesis for comminuted radial head fractures: A multicentric study. Acta Orthop. Belg. 2000;66:353.
40 Søjbjerg J.O., Ovesen J., Nielsen S. Experimental elbow instability after transection of the medial collateral ligament. Clin. Orthop. Relat. Res. 1987;218:186.
41 van Riet R.P., Morrey B.F., O’Driscoll S.W. Use of osteochondral bone graft in coronoid fractures. J. Shoulder Elbow Surg. 2005;14:519.
42 van Riet R.P., Morrey B.F., O’Driscoll S.W., van Glabbeek F. Associated injuries complicating radial head fractures. Clin. Orthop. Relat. Res. 2005;441:351.
43 Wick M., Lies A., Muller E.I., Hahn M.P., Muhr G. Prostheses of the head of the radius. What outcome can be expected? Unfallchirurg. 1998;101:817.