Chapter contents
7.1 Introduction 115
7.2 The complex pulse parameters 115
7.3 Arterial wall tension 116
7.4 Pulse occlusion 120
7.5 CM pulse qualities defined by arterial wall tension and ease of pulse occlusion 123
7.6 Pulse force 137
7.7 CM pulse qualities defined by pulse force 142
7.8 Pulse contour and flow wave 154
7.9 CM pulses defined by pulse contour 158
7.10 Revision of the 27 CM pulse qualities 170
7.11 Using the pulse parameter system 170
7.1. Introduction
This chapter introduces the more complex CM pulse qualities and the pulse parameters associated with them. The complexity of these CM pulse qualities is related to:
• The increased number of changes in pulse parameters associated with each CM pulse quality
• The complexity of each of the associated pulse parameters.
The complex CM pulse qualities are characterised by changes to two or more of the pulse parameters. For each to be defined as a specific CM pulse quality, it is necessary for changes in all the requisite parameters to be present.
7.2. The complex pulse parameters
In this chapter we examine four complex pulse parameters:
• Arterial wall tension
• Ease of occlusion
• Force
• Flow wave and pulse contour.
Although there may be changes in a number of pulse parameters for a complex CM pulse quality, usually one key parameter is considered to be the defining aspect of that particular CM pulse quality. This key parameter is often used to loosely categorise the CM pulse qualities. It should be noted that different CM texts may utilise different ways of grouping the CM pulses, according to differing pulse parameters.
Changes in these pulse parameters are associated with 15 of the 27 traditional CM pulse qualities. The CM pulse qualities associated with each of the complex pulse parameters are:
• Defined primarily by arterial tension and ease of occlusion: Stringlike (Wiry) pulse, Scallion Stalk pulse, Drumskin pulse, Tight pulse, Scattered pulse
• Defined primarily by flow wave and pulse contour: Slippery pulse, Rough pulse, Surging pulse, Stirred pulse.
As noted above, the pulse parameter of pulse occlusion plays an important role in the differentiation of the traditional CM pulse qualities associated with both arterial tension and pulse force.
The complex pulse parameters are so named because, unlike the simple parameters such as rate or rhythm, there is no single objective measurement to definitively evaluate these parameters. They encompass a number of different physiological characteristics involving the actual structure of the artery and the manner in which it responds to the pressure wave that is produced from cardiac contraction. The quality and quantity of blood volume and blood flow, cardiac function and the variability of smooth muscle tone within the arterial wall are equally important factors that impact on the radial artery pulsation. It is the degree to which these factors are involved that determines the specific CM pulse quality produced.
7.3. Arterial wall tension
The parameter of arterial wall tension is a complex pulse parameter, primarily concerned with the physical structure of the artery wall. The degree of arterial wall tension informs us about the functional state of Qi (particularly Yang) in the body. It is necessary to have some tension in the arterial wall. It is when the degree of arterial tension varies from the norm that this is seen as a diagnostic indicator of pathology. For example, variations in tension can result from the stasis or obstruction of Qi and/or blood, an underlying vacuity of Yin fluids and/or blood, or the vacuity of Qi (especially Yang).
The specific CM pulse qualities associated with this parameter are differentiated by the degree of arterial wall tension, ranging from greatly increased tension to a marked reduction. In this sense, it is not the pulse wave that is being assessed but rather the arterial structure. The tension, or lack of tension, in the artery is assessed distinctly differently from the actual shape of the pulse wave.
Five CM pulse qualities are defined primarily by the parameter of arterial wall tension:
• Stringlike (Wiry) pulse (section 7.5.1)
• Tight pulse (section 7.5.2)
• Scallion Stalk pulse (section 7.5.3)
• Drumskin pulse (section 7.5.4)
• Scattered pulse (section 7.5.5).
7.3.1. Differentiation of the CM pulse qualities primarily defined by changes in arterial wall tension
The five CM pulse qualities primarily defined by the degree of tension in the arterial wall range greatly in their presentation. At one extreme is the Stringlike (Wiry) pulse that resists deformation with finger pressure because of the significant increase in arterial wall tension. At the other extreme, the Scattered pulse is characterised by its distinct reduction in arterial tension, which makes it difficult to manually detect the presence of the arterial wall at all. The Drumskin pulse and Scallion Stalk pulse are also defined by the increased tension in the arterial wall. However, when increasing finger pressure is applied to the artery, the arterial wall has only momentary resistance before succumbing to the pressure, a result of their underlying vacuity. In this sense, they are ‘empty’. Further, a distinguishing feature of the Scallion Stalk pulse is the ability of the arterial wall to remain distinct and pliable even when the pulsation in the artery has been occluded.
In addition to changes in arterial wall tension, accompanying changes in other pulse parameters, such as pulse width, force and depth, further differentiate these five CM pulse qualities. However, it is the increase or decrease in tension in the arterial wall of these five pulses that predominantly differentiates them from the other traditional CM pulse qualities.
To further qualify this: the term ‘arterial wall tension’ has been used to encompass a range of different mechanisms that result in the arterial wall being able to be felt distinctly on palpation. The differing mechanisms influence how the increased arterial wall tension manifests in each pulse quality, depending on the involvement of other pulse parameters. For example, the Stringlike (Wiry) pulse and Tight pulse tend to arise due to increased smooth muscle tension within the artery wall, while the Tight pulse may additionally include sclerotic changes to the arterial wall, causing stiffness and a decreased ability to expand easily. So the underlying condition of the arterial wall may well influence how changes in pulse parameters manifest. For the Scallion Stalk pulse, a combination of increased arterial tension and decreased blood viscosity lead to its distinctive manifestation of pliable arterial wall and easy occlusion. This is replicated in the Drumskin pulse but complicated further by the presence of pathogenic Cold.
Constitutional body types may also influence the manner in which changes in pulse parameters present. For example, in an slim individual with a small build, who has smaller arteries than someone with a taller, larger build, increased arterial wall tension may result in a more typically Stringlike (Wiry) type pulse than it would in someone with a wider artery. However, it is the maintenance of this tension with increasing finger pressure, regardless of the width, that signifies the Stringlike (Wiry) pulse.
7.3.2. Definition of arterial wall tension
The degree of arterial wall tension is denoted by the level of clarity or distinctness felt in the artery wall with the palpating fingers.
Three factors are involved in the parameter of arterial wall tension:
• The distensibility and compliance of the arterial wall to pressure changes, whether this occurs internally from the pulse wave or externally from the pressure exerted by the practitioner’s fingertips
• The tone of the smooth muscle component in the arterial wall structure
• Secondary tensile changes occurring in the arterial wall structure unrelated to vascular smooth muscle.
Arterial tension contributes to the perceived ‘hardness’ of the arterial wall on palpation. When arterial tension is present, the artery can be easily distinguished from the tethering support of the surrounding connective tissue. Equally, a lack of arterial tension makes it difficult to distinguish the artery from the surrounding tissue.
Increased arterial wall tension can occur in both replete or vacuity conditions as a result of different physiological mechanisms. For example, increased arterial wall tension may occur in response to Yin vacuity or loss of Yin fluids, resulting in the relative hyperactivity of Yang and accordingly, increased arterial tension. The Scallion Stalk pulse is a good example of a vacuity-type pulse quality, where tension is not associated with vascular smooth muscle contraction but with tension in other parts of the rigid arterial wall structure (see section 7.3.5.2 Alternative mechanism for increased arterial wall tension). Alternatively, a Cold pathogen may lead to increased arterial wall tension by its contracting nature, obstructing Qi and blood flow. This pathogenic factor is considered to be an excess pattern, reflected in an increase in pulse force and arterial width and an increase in arterial wall tension associated with increased smooth muscle tone. The Tight pulse and the Firm pulse are good examples of excess-type CM pulse qualities with increased arterial tension due to contraction of vascular smooth muscle. Qi stasis may also result in hyperactivity of Yang Qi thus leading to increased tension
7.3.3. Arterial wall tension and its assessment
Assessing the arterial wall tension requires the use of two separate techniques:
• Assessment of the physical characteristics of the radial artery wall to determine the degree of arterial tension
• Assessment of pulse occlusion.
7.3.3.1. Assessment of arterial tension
Assessment of arterial wall tension employs the same technique as used in assessment of arterial width. This is initiated by placing the fingers on the skin surface above the radial artery at the three traditional pulse positions and moving them laterally from side to side, using a rolling type motion. This technique has been previously described in section 6.12.1 (see Fig. 6.10 depicting lateral sideways movement of fingers). When the artery is located deeper in the flesh then further finger pressure is required to locate this before moving from side to side. Be careful not to use excessive pressure when assessing for arterial wall tension, because the parameter is associated with both vacuity and replete-type pulses. If too much pressure is applied, then for the vacuity patterns the arterial wall becomes deformed and assessment of the arterial tension is compromised. Pressure needs to move over the artery without compressing it.
7.3.3.2. Assessment of pulse occlusion
Assessment of pulse occlusion requires compression of the arterial wall; in particular, this involves determining what happens to both the arterial wall and the pulsation when increasing pressure is exerted on it by the fingers. That is, does the wall retain its distinctive shape or is it easily deformed, does it easily regain its original form when pressure is released and how easy is it to occlude the arterial pulsation? (Box 7.1)
Box 7.1
Hints for assessing arterial tension
When assessing arterial tension, don’t focus on any pulsatile movement. Rather, your attention needs to focus on the actual arterial structure. The lateral movement of the assessing fingers will help you in this, disguising arterial movement while assisting in feeling the artery.
To assess ease of pulse occlusion, the fingers are placed at the three traditional pulse positions and finger pressure is gradually increased over the radial artery until pulsations can no longer be felt. This is held for five seconds. There are two subcategories for ease of occlusion:
• Easy to occlude: A pulse that is classified as easy to occlude requires little pressure exerted on it to halt the pulsations, with either the arterial walls easily compressed or the arterial pulsation being easily stopped. The level of depth at which the pulsation can be felt strongest does not affect pulse occlusion. That is, both superficially and deeply located pulses may be easily occluded.
• Difficult to occlude: Significant pressure is required to occlude the pulse, equal to the pressure that is needed to palpate to the deep level. In some cases, the pulse may be still felt under the fingers. Sometimes the pulse can still be felt at the side of the proximal side of the ring finger. This is seen as an indicator of pulse strength
7.3.3.3. Interpretation of findings
When arterial wall tension is increased above normal, the artery feels very distinct and can still be clearly felt under the fingers when pressure is applied into the deeper levels of depth. In the extreme case it is even difficult to indent the arterial wall at the deep level of depth. At the other extreme, a lack of tension often means that only a pulsation can be felt; there is no evidence of the arterial wall. In this situation when the fingers are moved from side to side on the wrist where the artery is situated, only the soft skin of the wrist can be felt; there is no indication of the artery. Of course, between these two extremes there is a range of degrees of arterial tension.
7.3.3.4. Normal levels of arterial tension
Ideally, some tension in the arterial wall is required for a pulse to be classified as healthy. Such a phenomenon is due to sympathetic vasomotor tone, which will be discussed in more detail shortly. When considered healthy, arterial tension should be felt so that there is a distinct ‘impression’ of the arterial wall so that the width can be ascertained, but it is not ‘hard’.
7.3.4. Regulation of arterial tension: CM perspective
From a CM perspective, arterial tension is particularly related to Yang Qi. Therefore factors that affect Yang Qi affect arterial tension. Variations in arterial wall tension may arise as a result of hyperactivity of Yang Qi due to obstruction or stasis, vacuity of Yang Qi or damage to Yin fluids, or as the result of emotional stress.
7.3.4.1. Role of Yang Qi
Pulse tension depends on the functional state of Yang Qi. Lu (1996: p. 109) quotes from the Nei Jing ‘When Yang Qi functions normally, it can maintain the flexibility of the tendons and vessels.’ This is explained further, that arterial tension increases when Yang Qi is hyperactive and decreases when Yang Qi is deficient. A good example of this is the Stringlike (Wiry) pulse that results from a hyperactivity of Liver Yang Qi. Conversely, when Yang Qi is deficient the arterial wall may be difficult to feel clearly, as in the Scattered pulse.
7.3.4.2. Effect of Yin and Blood deficiency on arterial tension
Both Yin and Blood, as a Yin fluid, not only act as carriers for Qi but also have a balancing, cooling and nourishing effect on Yang, allowing it, among other responsibilities, to maintain the normal tension in the arterial walls. If that harmonising effect is impaired through loss of Yin (in numerous ways such as acute or chronic loss of blood or body fluids through sweating, vomiting or diarrhoea) then this may have a number of effects on the pulse. In the case of arterial tension, Yang Qi becomes relatively hyperactive, leading to an increase in arterial wall tension.
7.3.4.3. Emotions and arterial wall tension
In CM, emotional stress is considered to be a major cause of disease due to the flow-over effect on the physical body. The expression of a range of emotional responses is considered to be a healthy part of the normal psyche, but if any of these becomes prolonged or excessive in nature, or is not expressed freely, this may have an adverse effect on the individual’s health. Most commonly this may affect the normal flow of Qi, which, if sustained, may lead to problems of Qi stagnation.
In particular, the Liver is susceptible to emotional disturbance, particularly anger or frustration or the inhibition of emotional responses. As the Liver has a vital role in maintaining the free flow of Qi and consequently blood, factors impacting on the Liver may also affect arterial tension.
7.3.5. Regulation of arterial wall tension: biomedical perspective
The nervous system is responsible for controlling general blood flow to different regions of the body, heart activity and arterial blood pressure regulation as discussed by Guyton & Hall (2006: pp. 204-215) in Chapter 18. It does so via the autonomic nervous system in which the sympathetic nervous system plays an integral role. Most of the blood vessels in the body (except the capillaries, precapillary sphincters and metarterioles) are innervated via sympathetic vasomotor nerve fibres that leave the spinal cord through the thoracic and upper two lumbar spinal nerves. These enter the sympathetic chain and then travel to the heart and viscera via specific sympathetic nerves, or travel through the spinal nerves to the blood vessels at the periphery of the body. Higher control from the vasomotor centre located in the medulla and pons of the brain transmits sympathetic impulses to the blood vessels around the body and parasympathetic impulses to the heart via the vagus nerves (Guyton & Hall 2006: p. 206). Blood flow is regulated via vasoconstriction or vasodilatation of the blood vessels (Box 7.2).
Box 7.2
Effects of the autonomic nervous system on blood flow
• Increased sympathetic activity increases heart rate and strength of cardiac contraction
• Increased parasympathetic activity decreases heart rate, but the effect on heart contractility is only minor.
7.3.5.1. Sympathetic vasoconstrictor tone
The perceived ‘hardness’ of the radial arterial wall relates to the tone of the vascular smooth muscle in the tunica media of the blood vessels wall and is influenced by the nervous system’s effect on the contraction and expansion of the arteries (Lu 1996: p. 179). (See Fig. 2.5 for layers of the muscular arteries.)
Under normal conditions there is a ‘partial state of contraction in the blood vessels, called vasomotor tone’ caused by the vasomotor centre in the brain sending continual signals to the vasoconstrictor nerve fibres systemically. This helps to maintain pressure within the arterial system (Guyton & Hall, 2006: p. 206).
7.3.5.2. Alternative mechanism for increased arterial wall tension
The distinctness of the arterial wall is not always due to vasoconstriction. The Scallion Stalk pulse and the Drumskin pulse are examples of pulse qualities that have a distinct arterial wall that is not due to increased vascular smooth muscle tone. The maintenance of a distinct arterial wall such as that perceived in the Scallion Stalk and Drumskin pulses in the presence of vascular smooth muscle relaxation causing vasodilatation (as a consequence of compensatory response to blood loss) may be explained as follows. Kelly & Chowienczyk (2002) state that in muscular arteries such as the radial artery, decreased vascular smooth muscle tone usually leads to increased compliance (the ability to accommodate large volumes with little increase in arterial pressure). As vessel diameter increases, compliance usually does too. However, this does not always happen. Sometimes very large decreases in vascular smooth muscle (i.e. in a fully relaxed state) may result in the stress being transferred to other rigid components of the arterial wall and this then leads to decreased compliance. This may hypothetically explain the appearance of the Scallion Stalk or Drumskin pulses so that even though the arterial diameter is increased (signifying vasodilatation and therefore relaxation of the smooth muscle) the arterial wall still has increased definition.
7.3.5.3. Effects of febrile conditions and the shiver reflex
Febrile disease (caused by factors such as bacterial infection, environmental conditions, dehydration or tissue damage) has an effect on the temperature control centre in the hypothalamus, resetting the body temperature to a higher than normal value (Guyton & Hall 2006: pp. 898-901). As a result, the current body temperature is now below the new set point so a number of mechanisms are activated to help raise the body temperature to the new level. They include skin vasoconstriction, thyroxine secretion and sympathetic nervous system effects to increase cellular metabolism. During this time the individual usually feels very cold, the skin is cold because of vasoconstriction and this stimulates shivering which is experienced as ‘chills’. The shivering reflex increases the tone of the skeletal muscles throughout the body.
Hypothetically, the combination of the sympathetic effects on the blood vessels, causing vasoconstriction, in conjunction with the increased muscular tone, may result in increased radial arterial wall tension. This may explain why the Tight pulse is described as appearing in acute conditions such as an attack of EPA of Cold, accompanied by fever and chills.
7.3.5.4. Arterial tension and hypertension
From a biomedical point of view, the specific cause of primary hypertension is largely unknown, with a combination of genetic and environmental factors thought to be responsible for its progression according to Brashes (Chapter 30 in McCance & Huether 2006: pp. 1086-1092). It appears that a number of factors may lead to increased blood volume and increased peripheral resistance including overactivity of the sympathetic nervous system (increased vasoconstriction and cardiac output), overactivity of control of vascular tone and defects in excretion of sodium by the kidneys, leading to increased water retention and therefore increased blood volume. As the cardiovascular system attempts to deal with the increased blood volume, cardiac output increases, then regulatory vasoconstriction occurs. Blood volume remains high and as a result the increased peripheral resistance leads to increased arterial pressure, hence hypertension.
The vasoconstriction of the systemic arteries and resulting increased peripheral resistance may explain why increased arterial wall tension is considered to appear in hypertension, with some authors citing the Stringlike (wiry) pulse or the Tight pulse as occurring in this condition (Maciocia 2004, Wiseman & Ellis 1996). Researchers at the First PLA Medical University, Guangzhou found that ‘Most patients suffering from coronary heart disease have stringlike pulse due mainly to disorder of cardiac function, lowered arterial compliance and increased total peripheral resistance’ (Chen, Lin, Meng et al 1996). Utilising a combination of manual palpation to identify possible CM pulse qualities and biomedical cardiac function indices, they found generally that the coronary disease group were assessed as having ‘taut pulses’ (113 out of 120 cases) as well as having decreased myocardial contractility, stroke volume, left ventricular and arterial compliance, impaired left ventricular function and increased total peripheral resistance. It was surmised that the formation of the Stringlike (Wiry) pulse was due to a combination of factors such as arteriosclerosis, decreased vascular compliance and increased peripheral resistance. While the majority of patients were considered to have ‘taut pulses’ it appeared that these tended to appear in combinations with other CM pulse qualities such as Slippery, Slow, Thready and Rapid. However, there was no further breakdown of the group into subcategories. In addition, no concrete definition was provided for the term ‘taut’ and this seems to have been used interchangeably with the term ‘stringlike’.
The Guangzhou College (1991) notes explain that the mechanism of the taut (Stringlike) pulse may be due to increased vasoconstriction or increased blood volume or a combination of both, caused by arteriosclerosis which leads to increased arterial pressure and peripheral vascular resistance.
7.3.5.5. Arterial tension versus arterial hardening
The distensible nature of the vascular system refers to the ability of the arteries and veins to expand and accommodate pressure changes: both those associated with normal moment-to-moment changes with heart contraction and long-term pressure changes with hypertension and hypotension. This reflects the body’s normal ability to respond to the nervous system’s signals for vasoconstriction or vasodilatation.
As discussed by Brashers (Ch. 30 in McCance & Huether 2006: pp. 1086-1092), factors such as arteriosclerosis can affect the stiffness of arterial walls impacting upon their ability to dilate or constrict. Arteriosclerosis is caused by thickening and hardening within the arterial wall with eventual narrowing of the arterial lumen. While perhaps due to normal aging, it may also play a role in hypertension and other circulatory disorders. Atherosclerosis is an inflammatory pathological change to the arterial system that results in the laying down of fatty plaques in the walls of the medium-sized and large arteries. This has effects on blood flow via a decreased lumen due to the presence of atherosclerotic plaques and other changes to the arterial wall. It plays a major role in coronary artery disease and cerebrovascular disease (stroke) by causing obstruction to blood flow. However, it has been noted by O’Rourke et al (1992: p. 98) that despite the obstructive effects on the coronary and cerebral blood vessels, it appears that atherosclerosis has ‘little effect on the transmission of the pulse over long lengths of the aorta or other conduit arteries’ and the ‘contour of the brachial or radial arteries is rarely altered’.
7.3.5.6. Other factors influencing vascular tone
The ability of the vascular walls to dilate and constrict is influenced not only by the nervous system activity but also by substances that are actively produced by the endothelial cells lining the inside of the blood vessels. These substances play a role in influencing the tone and structure of the arterial wall and also influence its susceptibility to damage such as atherosclerosis. Nitric oxide (which causes vasorelaxation) and endothelin (a strong vasoconstrictor) are mediators produced by the endothelium and participate in the regulation of both basal vascular tone and blood pressure (Cockcroft et al 1997: p. 55). It is hypothesised that increased arterial stiffness may therefore result not only from physical changes to arterial wall structure due to ageing and arteriosclerosis, but also from endothelial dysfunction, affecting the availability of nitric oxide.
7.3.5.7. Ageing and arterial changes
Generalised degenerative changes to the arterial tunica media are responsible for arterial stiffness leading to changes in arterial pressure with age, and this is emphasised with arteriosclerosis (O’Rourke et al 1992: p. 98). Arteriosclerosis reduces arterial compliance and affects the ability of the arteries to expand and contract to the changing pressures during systole and diastole. The stiffening of the arteries occurring with ageing is distinct from that of atherosclerosis, which affects mainly the intimal layer of the artery wall.
7.4. Pulse occlusion
Pulse occlusion refers to the method of applying finger pressure to temporarily stop the pulsation in the radial artery by compressing it against the radius. Specifically, we use the term ‘ease of occlusion’ to refer to the amount of pressure that is required to halt the radial arterial pulsation. Additionally, this parameter encompasses whether pulsation can still be felt at the side of the ring finger once the pulsation has been occluded. This is usually indicative of a pulse that has force and signifies sufficient fluid in the vessel.
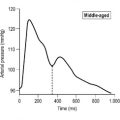
The parameter of pulse occlusion is not an actual component of the pulse, such as pulse rate, but rather is used as a diagnostic technique to provide further information about changes in other pulse parameters such as pulse force and arterial wall tension. Accordingly, pulse occlusion is used to further determine the overall strength of the pulse, relative fluid volume and the degree of tension within the arterial wall (Fig. 7.1). As such, it enables us to further differentiate between specific CM qualities that are defined by a number of other parameters.
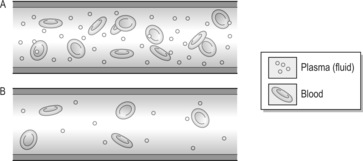 |
| Figure 7.1Schematic representation of variations in density of blood affecting tactile sensation of ease of occlusion. (A) ‘Normal’ blood viscosity. (B) Reduction in blood viscosity. |
7.4.1. Pulse occlusion: CM perspective
The parameter of pulse occlusion supplies information about the overall force of the pulse. However, this view is overly simplistic, as the ease with which a pulse is occluded is also influenced by other variables, including:
• The quality and activity of Yang Qi
• The volume of circulating fluids.
7.4.1.1. The quality and activity of Yang Qi
Yang Qi provides the motive force that initiates and sustains cardiac contraction, propelling blood through the arterial system. Yang Qi also plays a role in maintaining the normal tension of the arterial wall. Therefore, Yang Qi vacuity may result in a pulse that lacks force and/or has decreased arterial wall tension, resulting in a pulse that is easily occluded. Conversely, hyperactivity of Yang Qi may result in an increase in arterial wall tension and therefore the perceived ‘hardness’ of the arterial wall. The overall pulse strength and the volume of blood and Yin fluids may further influence this. For example, if Blood vacuity develops, then blood no longer cools the Liver, the Liver becomes hyperactive and overall Yang Qi is in relative excess resulting in an increase of arterial tension. In this situation, although tension is increased the pulse is relatively easy to occlude because of the underlying vacuity. There are two or three CM pulse qualities whose formation may be explained in this way.
The stronger the pulse wave the more difficult it is to occlude the pulse against the blood flow. Pulse force relates to both the relative activity of Yang Qi and the presence of sufficient Yin fluids to act as the medium to convey force. If Yin fluids diminish so too does pulse volume; accordingly, the loss of the carrier means that the force of the pulse is not transmitted through the vessels. The artery therefore becomes easier to occlude.
7.4.1.2. Volume of Yin fluids
Yin fluids refers not only to blood circulating in the arterial system but also to body fluids and Essence that reside in other areas of the body (see section 6.11.4.1 for futher information). These are involved in nourishing the organs, skin, muscle and joints and also in the maintenance of blood volume. As Clavey (1995: p. 13) notes, ‘In pathological situations, blood and jin ye fluids influence each other considerably’.
Therefore with blood loss, Jin Ye fluids can move into the blood vessels from the surrounding tissues to compensate for the fluid loss and replenish the blood volume, but not necessarily the quality of blood (there is no immediate regenerative effect on the loss of red blood cells). This has the effect of decreasing the viscosity of the blood (due to the loss of red blood cells, and therefore a greater proportion of plasma than usual). This may result in an artery that feels ‘empty’ (decreased density) and therefore more easily occluded.
Conversely, when there is a loss of body fluids, this can cause fluids from the blood to leave the blood vessels to help replace the lost body fluids. However, this leaves the ‘vessels empty and deficient, a condition known in TCM as “jin ku xue zao”: jin withered and blood parched. This can lead to severe Shen disturbance as the blood that would normally nourish the Heart becomes inadequate’ (Clavey 1995: p. 14). This also has the effect of increasing the viscosity of the blood (greater proportion of red blood cells than usual due to decreased plasma volume). As a result, this may result in the blood flowing less smoothly, due to increased resistance to the blood flow due to increased ratio of red blood cells to plasma (see Box 7.6).
Box 7.6
Body fluid loss versus Blood loss
From a biomedical perspective, the loss of either blood or body fluids (if severe, leading to hypovolemic shock) has a similar effect physiologically on the circulatory system by reducing cardiac output. Body fluid loss may occur due to excessive sweating, excessive urination or failure to replace lost fluids (inadequate fluid intake), while severe vomiting and diarrhoea can also affect both fluid and electrolyte balance. This loss of body fluid is known as dehydration.
In body fluid loss, plasma moves from the intravascular (inside the circulatory system) to the extravascular space to compensate for the lost volume. While this has a similar effect on the body’s autoregulatory mechanisms as a decrease in blood volume, there is an important difference:
• A decrease in plasma volume means that the viscosity of the blood is greatly increased due to the higher concentration of red blood cells and as such, results in sluggish blood flow (Guyton & Hall 2006: p. 285).
• Blood loss, on the other hand, results in a loss of both plasma volume and red blood cells, therefore the viscosity of blood will tend to decrease. This has the effect of decreasing the resistance to blood flow and increasing the flow rate, as thick fluids cause greater resistance to flow and move more slowly than thin fluids (McCance & Huether 2006: p. 1057).
7.4.2. Pulse occlusion: biomedical perspective
In biomedical terms, the degree of ease with which the pulse can be occluded is considered to be a function of pulse volume. The pulse volume is equated with pulse strength or amplitude, which is reflective of both stroke volume (the amount of blood expelled from each ventricle during systole) and peripheral vascular resistance (Estes 2006: p. 252). The pulse volume (perceived as the strength of pulsation) should be equal with each beat and should be palpable with moderate pressure, being able to be occluded with increased pressure.
Pulse volume is usually assessed via a three- or four-point scale ranging from absence of pulsation through to ‘bounding’ which is described as being ‘difficult to obliterate with pressure’ (Estes 2006: p. 254). Terminology that is commonly used to describe pulses with decreased volume includes ‘thready’ or ‘weak’, and these pulses are considered to be very easily occluded with light pressure, in accordance with the similarly defined CM pulse qualities (Box 7.3).
Box 7.3
Objective measurements of the pulse and ease of occlusion
In a study comparing objective measurements of the radial arterial pulse using applanation tonometry and assessment of the pulse using manual palpation, Walsh (2003) found a significant relationship for two tonometry measurements and the manual evaluation of pulse occlusion. These were PMaxPdt and peripheral systolic pressure (PSP) for the right hand.
The PSP reading was a measure of the maximum pressure exerted by the pulse wave in the radial artery during systole. For ease of pulse occlusion, the results indicated that high peripheral systolic pressure was associated with an increased difficulty in occluding the radial pulse by the pulse assessors using manual palpation (systolic pressure means below 120.2 mmHg for assessor 1 and 117.2 mmHg for assessor 2). Pulses that were selected as easy to occlude were associated with a low peripheral systolic pressure (means below 108.2 mmHg for assessor 1 and 107.7 mmHg for assessor 2).
PMaxPdt relates to the change in pressure with respect to time during systole. Walsh (2003) found that a greater mean value was associated with pulses selected as difficult to occlude (>700 mmHg/s) while a low value was associated with pulse selected as easy to occlude (< 600 mmHg/s). This indicates that the quicker maximum pressure is attained during systole (requiring the heart to contract strongly), the more likely the pulse was to be identified as being difficulty to occlude. This indicated a significantly shorter time to reach maximum pressure when the heart contracted for pulses rated as difficult to occlude compared to pulses rated as easy to occlude. Hence pulse force also has a bearing on ease of pulse occlusion.
The relationships as noted by Walsh (2003) must be viewed as a preliminary finding and as such need to be replicated in further studies with the possible investigation of CM descriptions of overall qualities described as easy to occlude, such as the Vacuous and Stringlike (Wiry) pulse, with specific disease states.
Changes in pulse volume from the norm can occur due to changes in either stroke volume or peripheral resistance. The pulse may be easily occluded if the circulating blood volume in the arterial system is decreased. Factors resulting in decreased stroke volume can include heart failure, cardiogenic shock leading to problems with heart contraction or decreased ventricular filling time due to problems with the heart’s conduction system.
Peripheral vascular resistance (PVR) is related to the ease with which blood flows through the circulatory system. Increased PVR (due to narrowing of the aorta or inflammation of the pericardium) may lead to a pulse with low amplitude that is easily occluded.
Conversely, the pulse may be more forceful than normal due to fever, infection, exercise, emotional anxiety or hyperthyroidism. Severe anaemia is also considered to be a factor causing a ‘bounding pulse’ due to the dual effect of decreased blood viscosity leading to decreased peripheral resistance and hypoxia (decreased oxygen to tissues) resulting in increased peripheral dilatation of blood vessels. These both lead to a greatly increased venous return to the heart and therefore greatly increased cardiac output (Guyton & Hall 2006: p. 236).
7.4.2.1. Factors affecting blood volume
As pulse volume is partially reflective of blood volume then factors affecting blood volume can also impact on how easily the pulse can be occluded. Blood volume can may be impaired as a result of:
Acute blood/plasma/body fluid loss
Blood/plasma loss may occur suddenly such as acute haemorrhaging due to trauma or gastrointestinal bleeding such as a perforated stomach ulcer. Fluid loss may occur due to excessive vomiting, sweating, diarrhea, dehydration or excessive urination. Hypovolemic shock is a type of circulatory shock that refers to the decreased blood volume resulting from blood or plasma loss. Circulatory shock causes inadequate blood flow around the body. There are usually three stages of circulatory shock (Guyton and Hall 2006: pp. 279-285, Tortora & Grabowski 2000, McCance & Huether 2006):
1. Nonprogressive (or compensated) shock: the body’s normal compensatory circulatory mechanisms are sufficient to eventually restore normal blood flow.
2. Progressive shock: certain positive feedback mechanisms occur to further weaken the heart and reduce cardiac output so the shock becomes progressively worse.
3. Irreversible shock: the further progression of shock until death.
From a CM perspective the different stages of hypovolemic shock may be the mechanism underlying the traditional CM pulse qualities such as the Faint pulse or the Scallion stalk pulse, relating to sudden acute blood loss (see individual CM pulse qualities for more information).
Chronic blood loss
Chronic blood loss may occur over time due to heavy menstrual bleeding, abnormal uterine bleeding, gastrointestinal bleeding, nosebleeds, hematemesis, hemoptysis, bleeding from haemorrhoids or cancer. Chronic blood loss may mean that blood loss is occurring at a faster rate than haemoglobin can be replaced, resulting in smaller red blood cells containing less haemoglobin (Guyton & Hall 2006: p. 426).
According to McCance & Huether (2006: p. 942)‘haemorrhage that is chronic (occult) produces adaptations that are less prominent and the individual experiences an iron deficiency anaemia when iron reserves become depleted.’
Insufficient blood production
Dietary restraints on eating sources of iron or the poor absorption of appropriate nutrients for the production of blood will also affect blood quality. While plasma volume remains unchanged, the number or size of red blood cells (RBCs) may be adversely affected, leading to a decrease in blood viscosity.
Each of the above situations impacts upon either the number of RBCs, plasma volume or haemoglobin-carrying capacity of the RBCs and therefore affects the circulatory system in varying degrees, hence the appearance of certain CM pulse qualities (see section 7.5.3.7 for more detailed information). These processes may be reflected within the CM pulse qualities such as the Fine, Faint or Scallion Stalk pulse qualities.
7.5. CM pulse qualities defined by arterial wall tension and ease of pulse occlusion
7.5.1. Stringlike (Wiry) pulse (Xián mài)

The Stringlike (Wiry) pulse is primarily defined by the physiological presentation of the arterial wall. Specifically, it is the high degree of arterial wall clarity that is of interest. The actual shape of the flow wave through the artery is a consequence of this increased tension in the radial arterial wall (Fig. 7.2).
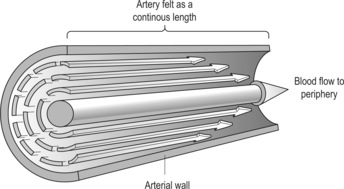 |
| Figure 7.2Schematic representation of the Stringlike (Wiry) pulse: Arterial tension constraining flow wave. The arterial wall is felt distinctly as a continuous length under all three fingers.(Adaptal from Figure 29.33 of McCance & Huether 2006 by permission of Elsevier Mosby.) |
7.5.1.1. Alternative names
In CM pulse literature the Stringlike (Wiry) pulse is most commonly called the Wiry pulse, but is also variously known as the Bowstring, Stringy or Strung pulse.
7.5.1.2. Requisite parameters
The Stringlike (Wiry) pulse is defined by changes to three pulse parameters:
• Arterial wall tension: The Stringlike (Wiry) pulse has increased arterial tension
• Length: The Stringlike (Wiry) pulse can be felt at all three traditional pulse positions and beyond Chi
• Pulse occlusion: With increasing finger pressure the arterial wall resists deformation, retaining its definitive shape.
7.5.1.3. Clinical definition
The Stringlike (Wiry) pulse has an increase in arterial wall tension and therefore the pulse wave cannot express its normal wave-like fluidity. Rather, it is the distinctness or tension in the arterial wall that inhibits the normal expansion and contraction response to the pressure and flow wave travelling through it. In this sense, it is not the pulse wave that defines the Stringlike (Wiry) pulse, but the actual physical structure of the arterial wall.
The arterial wall is perceived as rigid or dense due to the increased arterial tension, strongly resisting changes to its form when increasing finger pressure is exerted on it. Due to the increased smooth muscle tone in the arterial wall, the pulse is felt as a length of pulsation across the entire arterial segment at the wrist.
7.5.1.4. Identifying whether the Stringlike (Wiry) pulse is present
Step 1: This technique requires assessment of the ‘rigidity’ of the arterial wall (we are not actually concerned with the pulse wave at this time). Fingers are placed on the skin above the radial artery exerting light pressure moving repeatedly over the artery, medially and laterally (rolling side to side). (See Fig. 6.10 showing direction of movement of fingers across the width of the radial artery.)
Step 3: It is noted in the pulse literature that the Stringlike (Wiry) pulse retains its form when pressure is exerted on it: ‘stiff under the force of the fingers’ (Deng 1999: p. 143) and ‘press and it does not vary’ (Li, Flaws (trans) 1998: p. 100). The often repeated comparison of the Stringlike (Wiry) pulse with the wire string of a musical instrument also brings to mind the image of a pulse that retains its shape even with pressure exerted on it. In terms of the resilience of Stringlike (Wiry) pulse to deformation, two factors should be noted:
• The arterial wall resists deformation to finger pressure possibly even maintaining its shape as the deep level of depth is examined, although it can probably be occluded with sufficient pressure.
• From our experience, when pressure is released from the deep level of depth, the arterial wall quickly regains its original shape.
7.5.1.5. Levels of depth
The Stringlike (Wiry) pulse may be able to be felt at all levels of depth, but is usually strongest at the middle level of depth. However, pulse depth is not an essential component of the Stringlike (Wiry) pulse, rather it is the increased arterial tension. Where changes in both pulse depth and arterial tension occur concurrently, this may develop into a different CM pulse quality such as the Firm pulse which has increased arterial tension but is also found to be forceful and wide at the deep level of depth. Such a pulse type has a different pathogenic mechanism to that of the Stringlike (Wiry) pulse and therefore a different physical presentation.
7.5.1.6. Classical description from The Lakeside Master’s Study of the Pulse
The bowstring pulse is level and straight like the long [description from the Su Wen].
It is like a drawn bowstring [description from the Mai Jing].
Press and it does not vary …
Its shape is like the strings of a zither [description from the Mai Jue].
Passing through, straight and continuous,
It is stiff under the fingers’
7.5.1.7. CM indications
The Stringlike (Wiry) pulse primarily reflects pathology relating to constrained Qi, particularly involving the Liver. This may be transient, reflecting acute stressful situations, or may be indicative of chronic constraint of Qi and consequently associated with pathology. This is termed Qi stagnation and is commonly associated with the Liver. Other CM patterns that can be associated with obstruction of Qi include the presence of pathogenic factors such as Phlegm or Damp. Pain is also usually the result of Qi or Blood stasis (stagnation), so the Stringlike (Wiry) pulse can occur in any condition accompanied by pain.
Liver disharmonies
The Liver is traditionally associated with assisting the free spread of Qi throughout the body, and its movement is considered to have an expansive nature. In addition, the Liver has a major role to play in the storage of blood, providing sufficient blood to circulate through the blood vessels and channels, while returning at night to be stored in the Liver. The patterns of disharmony associated with the Liver therefore involve obstruction of this normal free flow and spreading of Qi and blood.
Liver disharmonies associated with the Stringlike (Wiry) pulse include Liver Qi stagnation, Liver Yang rising, Liver Fire, internal Liver Wind and Liver Blood stasis (Box 7.4).
Box 7.4
Signs and symptoms associated with Liver/gallbladder disharmonies
These depend on the exact Liver pattern but may be associated with the following:
• Irritability, anger, frustration, depression
• Rib or flank pain
• Sighing
• Flatulence
• Pellet-like stools
• Sore, red eyes
• Bitter taste in the mouth
• Muscular problems such as cramping
• Clinical relevance: Liver patterns can often be seen in patients suffering from emotional stress of some type or actual liver or gallbladder disease. The Stringlike (Wiry) pulse can also result from painful conditions of liver or gallbladder origin such as cholecystitis.
• Mechanism: The Liver is responsible for allowing the smooth circulation of Qi and therefore Blood throughout the body. Liver Qi is easily affected by emotions such as anger, irritability, resentment or the suppression of emotional stress, obstructing Qi flow.
Yang Qi is responsible for maintaining the normal tension of the arterial wall. If Liver Yang becomes hyperactive this can lead to increased tension in the pulse.
Phlegm or Damp
A number of authors agree that the Stringlike (Wiry) pulse can be seen in Phlegm patterns (Deng 1999, Li (Flaws trans) 1998, Lu 1996, Lyttleton 2004, Maciocia 2004). Phlegm is formed by a number of different processes (see Clavey (1995) for a comprehensive discussion on the aetiology and symptomatology of Phlegm) and may occur due to Heat or Fire within the body, causing body fluids to dry up and congeal. Alternatively, Liver Qi stasis can eventually turn to fire, again drying fluids. Flaws (1997: p. 53) describes Yin obstruction (due to Damp, Phlegm, food or blood causing obstruction or stasis) as being capable of impeding the free flow of Qi.
Phlegm/Damp is able to enter and ‘choke the circulation both inside and outside of the blood vessels’ (Clavey 1995: p. 177) impeding the flow of blood. This can be equated with hypertension in a biomedical context, where there is sclerotic loss of vascular elasticity and therefore increasing hardness of the arterial wall.
Clinically this can be seen in conditions such as epigastric fullness, nausea, vomiting, coughing with production of phlegm. Phlegm/Damp may also result in gynaecological problems such as amenorrhoea and infertility and this may present as a Stringlike (Wiry) pulse, particularly if Liver Qi stagnation is the contributing cause (Lyttleton 2004).
Pain
The Stringlike (Wiry) pulse may be seen in any condition where there is pain. From a CM perspective, pain indicates obstruction of Qi or blood or both. Therefore the lack of free flow is reflected in the increased arterial tension in the pulse. Pain evokes a systemic response, activating the sympathetic nervous system. This will tend to override other pulse variables, with increased arterial tension the predominating change in pulse parameters. Clinically, this pulse may be seen in abdominal or epigastric pain, dysmenorrhoea, headaches and musculoskeletal problems, irrespective of the cause.
Liver attacking the Spleen
Rogers (2000) describes this pattern as Wood energy attacking Earth energy, while Lu (1996) and Deng (1999) briefly mention the pattern of Liver encroaching on Spleen due to an underlying vacuity of the Earth energy. The aetiology is premised on the Five Phase (Wu Xing) arrangement of the organs involving the Ke cycle. The Ke cycle is the controlling cycle and within this cycle the Liver is responsible for keeping in check the functions of the Earth, particularly the Spleen. When the Spleen and Stomach Qi become deficient, or the Wood overexerts its controlling function, this results in digestive problems that present with both Wood and Earth type symptoms. For example, irritable bowel syndrome presenting with alternating diarrhoea and constipation and exacerbated by stress is a classic presentation of the Wood attacking the Earth pattern. Flaws (1997) suggests that a commonly seen pattern is Liver Qi stasis, occurring in conjunction with both Spleen damp and Blood vacuity.
Malaria
A number of authors (Li, Flaws (trans) 1998, Deng 1999, Lu 1996) describe malaria as presenting with a Stringlike (Wiry) pulse. Malaria is a febrile condition and in CM is usually recognised as having an exogenous Cold origin that has entered the body and is located between the interior and exterior. This is equivalent to the Shao Yang stage of Six Divisions (associated with the Gallbladder and Triple Energiser channels). Typical symptoms include fever, chills and severe headaches.
7.5.1.8. Does the Stringlike (Wiry) pulse occur in vacuity patterns?
The Stringlike (Wiry) pulse, in its true form, usually occurs in replete (excess-type) patterns. This is not to say that increased arterial wall tension does not occur in response to Yin or Blood vacuity. Flaws (1997) advises that the Stringlike (Wiry) pulse may evolve as the result of Blood vacuity, which affects the Qi by removing its ‘moisture and nourishment’. This, in turn, affects the free flow of Qi, leading to stagnation.
A number of pulses that reflect Blood vacuity do in fact present with increased tension, but these are not necessarily the definitive Stringlike (Wiry) pulse. If Blood vacuity occurs, then one might expect accompanying changes in other pulse parameters refecting the underlying vacuity pattern (such as a decrease in pulse force or change in width) and consequently the formation of another CM pulse quality, for example the Scallion Stalk pulse.
7.5.1.9. Clinical relevance of arterial wall tension
Although the Stringlike (Wiry) pulse in its extreme form may not always be present, there are many instances in which increased arterial wall tension may be identified in the pulse. Rather than trying to fit such a pulse into a certain CM pulse quality definition, and risk disregarding changes in other pulse parameters by doing so, we need to understand what the increase in arterial tension actually means in terms of pathogenesis.
Increased arterial tension may be construed as resulting from obstruction or stasis of Qi and/or blood, remembering that this may have a number of differing causes. This may seem overly simplistic, but it should be remembered that this information should then be incorporated into the bigger picture with the diagnostic information obtained from other aspects of the pulse and the other diagnostic techniques. The example used in the above section on Blood vacuity is a prime example of this. If the pulse information were underutilised to identify the pulse solely as the Stringlike (Wiry) pulse, then information regarding the underlying vacuity (represented by the ease of pulse occlusion in conjunction with the lack of force) would be lost.
7.5.1.10. Increased arterial wall tension as a reflection of stress
An increase in arterial tension in the pulse may be a normal transient response to stressors. This can be seen in the ‘fright, flight or fight’ response due to the release of epinephrine (adrenaline) and norepinephrine (noradrenaline) mediated through the sympathetic nervous system. CM would see this as a pathological type quality, but it could also be seen as a normal response to an acute situation. Stress in this situation is not considered an adverse reaction, but as an effective mechanism for allowing us to cope with increased demands on the body whether due to physical, emotional or psychological factors. A similar situation is seen in the body’s response to pain. In the pulse literature, the pulse qualities often associated with pain have as one of their main defining characteristics, an increase in arterial wall tension, for example the Tight or Stringlike (Wiry) pulses. In this regard, pain is seen as a stressor in the body.
Stress only becomes a problem if this tension remains after the stressor has passed, or if this type of stress becomes chronic. Clinically, if stress occurs – for example preparing for an exam or meeting deadlines at work – then the temporary stress is seen as a useful motivating force, rather than something to be treated. It is when the stress affects the body’s ability to be productive or to continue with normal activities, or when stress becomes chronic, that intervention is required. In these cases, levels of cortisol are consistently raised. Cortisol – one of the glucocorticoids produced by the adrenal cortex, useful in helping the body’s resistance to stress by increasing the production of ATP (used to produce energy) – makes the blood vessels more sensitive to substances that have a vasoconstrictive effect, which means that it effectively raises blood pressure (Tortora & Grabowski 2000). This is effective if the stress is due to blood loss; however, if it is not and this is happening consistently, then the increased blood pressure may have potentially harmful long-term effects on the heart and circulatory system.
7.5.2. Tight pulse (J n mài)
n mài) 
 n mài)
n mài) 
The Tight pulse is a complex pulse quality that is defined primarily by the effect of increased arterial wall tension on the pulse wave.
7.5.2.1. Alternative names
The Tight pulse is also known as the Tense, Intent, Taut or Squeezed pulse.
7.5.2.2. Requisite parameters
The Tight pulse has changes in four pulse parameters:
• Arterial wall tension: The Tight pulse has increased arterial tension.
• Force: There is an increased intensity of pulsation, so that this is a forceful pulse quality.
• Width: The arterial width is increased, so that it is perceived as a wide pulse.
7.5.2.3. Clinical definition
The Tight pulse, as its name implies, has a decrease in the elastic properties of the arterial wall so that is less able to expand and contract smoothly in response to the pressure and flow waves produced by the contraction of the heart. This is felt as an increase in arterial tension, so that the arterial wall is perceived as ‘hard’. The pulse displaces a wide surface area laterally across the finger, being perceived as having a wide arterial diameter. The pulsation hits the finger with increased intensity, and is therefore classified as a forceful pulse.
Although there are no direct references to the length of the Tight pulse, it is often likened to the Stringlike (Wiry) pulse (Li, Flaws (trans) 1998, Lu 1996, Wiseman & Ellis 1996) which is commonly described as long. Additionally, the descriptions often infer length and increased width by equating the Tight pulse with a rope or cord.
While increased width, length and tension are also invoked by the description of ‘vibrates to the left and right like a tightly stretched rope’ (Li, Huynh (trans) 1981: p. 18), this description also gives rise to what is considered to be, by some authors, the distinguishing feature of the Tight pulse; the slight lateral or sideways movement of the artery under the palpating fingers. This is surmised as occurring due to the heightened degree of increased arterial wall tension; the pressure pulse wave causes the artery to ‘vibrate’ or ‘contort’ side to side (left to right) due to the arterial wall’s inability to absorb and transmit the pulsatile force readily.
7.5.2.4. Confusion over pulse descriptors
There is some confusion in the CM literature over the actual presentation of this pulse quality. While some texts mention a side to side or left to right movement, much of the literature tend to also reiterate the traditional pulse descriptions which describe its similarity to feeling a ‘tightly twisted’, ‘taut’ or ‘tensely drawn’ rope (Deng 1999, Flaws 1997, Kaptchuk 2000, Lu 1996, Wang, Yang (trans) 1997).
Review of the pulse literature reveals that the Tight pulse is generally considered to be a forceful pulse. Li (Flaws trans 1998: p. 93) describes the Tight pulse as ‘left and right, pellet-like to the human hand’. The term ‘pellet like’ is defined earlier in the same text in another pulse definition as being round and hard, but not short. It is also described in the Mai Jing (Yang (trans) 1997: p. 3) as feeling ‘irregular like a turning rope’. Deng (1999: p. 128) utilises a number of different references, which again address the rope metaphor. However, the idea of an irregularity in form, not rhythm, is also raised, with additional descriptions of the pulse ‘with pressure it is like rolling, not even, but with bumps’ and reinforced by the likeness of the Tight pulse to a cord composed of a number of different threads twisted together. There are at least three possible interpretations here: one referring to the physical imperfections of the arterial wall; another to the action of the pulse wave due to the greatly increased tension of the arterial wall causing the artery to appear to slightly ‘shake’ or ‘vibrate’ sideways; thirdly, to the actual slipping of the artery from under the fingers due to the heightened arterial tension.
7.5.2.5. Identifying whether the Tight pulse is present
The Tight pulse is formed due to the increased arterial wall tension, which affects how the pressure and flow wave travels through the radial artery.
Step 1: The main feature of the Tight pulse is the significantly increased arterial wall tension, resulting in a tautness that can be felt under the palpating finger. The increased rigidity of the arterial wall results in either: the pressure wave causing the artery to move sideways as it passes through the artery or the artery moves sideways when finger pressure is applied, slipping away from the tips of the fingers.
Step 2: When assessing pulse force, the pulsation hits the fingers with increased intensity, and the artery resists deformation with increasing finger pressure.
Step 3: The pulsation is felt across a broad surface area of the palpating fingers and is therefore defined as wide.
7.5.2.6. Differentiating the Tight pulse from similar CM pulse qualities
There are a number of CM pulse qualities that have increased arterial wall tension. However, these are further distinguished by differences in other pulse parameters and accordingly these changes reflect the underlying pathogenesis (Table 7.1).
| -:not a requisite pulse parameter for this CM pulse quality. | |||||
| Tight pulse | Firm pulse | Stringlike (Wiry) pulse | Drumskin pulse | Scallion Stalk pulse | |
|---|---|---|---|---|---|
| Arterial tension | ↑ tension | ↑ tension | Significantly ↑ tension | Significantly ↑ tension | ↑ tension |
| Response of arterial wall to degree of tension | Arterial wall very distinct, ↑ tension causes slight sideways movement | Arterial wall very distinct | Arterial wall very distinct | Very taut on palpation | Can feel arterial wall distinctly |
| Pulse occlusion | Retains form with increasing finger pressure due to increased internal resistance within artery. | Retains form with increasing finger pressure due to increased internal resistance within artery. | Retains form with increasing finger pressure due to increased internal resistance within artery. | Retains form with increasing finger pressure but with heavy pressure, the pulse is easily occluded due to the lack of internal resistance (decreased volume) | Retains form even when pulse is occluded but rather than being rigid, it has a pliable arterial wall. |
| With significant pressure, pulse is occluded. | With significant pressure, pulse is occluded. | With significant pressure, pulse is occluded. | The pulsation is easily occluded due to the lack of internal resistance (decreased volume) | ||
| Arterial width | ↑ width | ↑ width | – | ↑ width | ↑ width |
| Pulse length | Long | Long | Long | – | – |
| Pulse force | ↓ force | ↑↑ force | – | ↓ force | ↓ force |
| Pulse depth | – | Deep level of depth | − | Superficial level of depth | Superficial level of depth |
| Pathogenesis | Pain, food retention, EPA cold or internal cold | Internal cold, internal obstruction due to Qi or Blood stasis and pain | Qi stagnation LV/GB disharmony phlegm/damp malaria pain | Yin vacuity complicated by EPA cold acute profuse Yin fluid loss severe Yin & Essence vacuity | Loss of Blood or Yin fluids (acute or chronic Blood vacuity) |
The five CM pulse qualities listed in Table 7.1 all present have increased arterial present wall tension. The Scallion Stalk pulse and Drumskin pulse are easily occluded with pressure, whereas the Stringlike (Wiry) pulse clearly retains its form. The Firm pulse has a similar pathogenic mechanism to the Tight pulse, in relation to the presence of pathogenic Cold. In this sense, the Firm pulse and the Tight pulse are interrelated and the Firm pulse could be considered a variation of the Tight pulse but located at the deep level, reflecting the invasion of pathogenic Cold moving directly into the interior. The Tight pulse and Firm pulse have similar changes in pulse parameters and therefore may present in a similar fashion; however, the Firm pulse is always found to be relatively strongest at the deep level of depth. This specifies the location of the disease, which is at the internal level and also reflects the inability of Yang Qi to move outwards due to obstruction, shown by the increased arterial tension. In addition, the Tight pulse as an increase in arterial tension such that the artery gives the impression of slightly moving side to side as a result of the pulse wave moving through the constricted arterial wall.
7.5.2.7. Classical description from the Mai Jing and The Lakeside Master’s Study of the Pulse
The tight pulse is an inflexible pulse like a tensely drawn rope [said in another version to feel like a turning rope]
The tight pulse comes and goes with force.
Left and right, pellet-like to the human hand. Su Wen)
7.5.2.8. CM indications
It is commonly understood that the Tight pulse is indicative of pain. Pain arises from the obstruction of Qi and/or blood flow. With the Tight pulse, Cold is considered the primary cause of pathogenesis in the pulse literature. This is attributed to the contracting nature of Cold, which is seen as having a constricting effect on the arterial wall. Therefore the Tight pulse can be seen in disharmonies relating to stagnation of Qi and/or blood commonly due to pathogenic Cold, usually presenting with pain as a primary symptom. However, the Tight pulse may be seen in any painful condition due to obstruction of the normal flow of Qi and blood. The four patterns associated with the Tight pulse are:
• Pain
• Internal Cold
• EPA of Cold
• Food retention
Pain
Pain is a common symptom associated with obstruction of Qi and/or blood flow. The associated signs and symptoms will depend on the location of the pain and the specific organ affected. The nature of the pain, for example sharp, distending, stabbing or dull, assists in identifying the pattern of disharmony.
Internal Cold (abdominal and pelvic regions)
Three organs are particularly vulnerable to direct invasion by pathogenic Cold: the stomach, the large intestine and the uterus (Maciocia 1989). This can result in strong pain due to the obstruction caused by the contracting nature of Cold on Qi and blood flow.
Clinically, the Tight pulse may be seen in conditions such as sudden stomach pain, abdominal distension and fullness, diarrhoea, loss of appetite or dysmenorrhoea (menstrual pain). Exposure to environmental cold or excessive consumption of cold, raw food such as ice cream, fruit, salad or cold drinks may contribute to the formation of this pulse. In women, exposure to Cold during menstruation, such as swimming or wearing inadequate clothing in cold weather, are also seen as potential causative factors (Lyttleton 2004: p. 17).
EPA of Cold (without abdominal symptoms)
This may be seen in an external invasion of Wind Cold and may occur following exposure to cold weather. Pathogenic Cold has a contracting effect on the blood vessels, causing an increase in arterial tension. As an EPA, it would be expected that the pulse would also be felt relatively strongest at the superficial level of depth, providing the body’s Zheng Qi is strong.
Clinically, this may be seen as an acute onset of a cold or flu-type viral infection. Common signs and symptoms include strong body aches, aversion to cold, chills and fever, no thirst or sweating and a sore throat.
Food retention
Food retention may occur when Stomach Qi is deficient or not descending properly or there is excessive food intake. This can cause obstruction of Qi and blood leading to pain, hence the formation of the Tight pulse.
7.5.2.9. Biomedical perspective
The over-distension of a hollow organ, such as the stomach, can result in pain either by overstretching the actual tissue or because the overfilling leads to compression of blood vessels supplying or surrounding the organ. This can lead to pain due to the reduced blood flow to the area (this is known as ischaemic pain) (Guyton & Hall 2006: p. 604).
Intestinal obstruction can occur within or outside the intestines, resulting from fibrous adhesions (postsurgical or from trauma), twisting of the part of the intestine, herniation, inflammatory intestinal disease or diverticulitis. This may lead to distension and pain, depending on the severity and location of the obstruction.
7.5.3. Scallion Stalk pulse (Kōu mài)

The main area of focus for the Scallion Stalk pulse is on the physiological presentation of the arterial wall and the manner in which it reacts to increased finger pressure, retaining its clarity and form.
7.5.3.1. Alternative names
Hollow, Onion Stalk, Leekstalk or Split pulse.
7.5.3.2. Requisite parameters
The Scallion Stalk pulse is a complex pulse quality with changes to five pulse parameters:
• Arterial wall tension: There is an increased arterial wall tension
• Depth: The Scallion Stalk pulse is found to be relatively strongest at the superficial level of depth
• Width: The arterial width is increased, resulting in a wide pulse
• Force: The overall pulse force is decreased in intensity
7.5.3.3. Clinical definition
Two components are involved in defining this pulse: the first relates to the arterial wall tension and the second concerns the pulse wave. There is a distinct and palpable arterial wall at both the superficial and deep levels of depth, reflecting an increase in the arterial wall tension. The pulse wave can be felt relatively strongest at the superficial level of depth, but there is an overall lack of intensity to the pulsation reflecting the underlying vacuity of blood. This means that when finger pressure is applied to the artery the pulsation is easily occluded.
It is the combination of the above two factors which creates the most distinguishing feature of this pulse; the wall of the artery can still be very distinctly felt even when the pulsation within the artery has been occluded. This results in being able to roll the fingers over the arterial wall under the palpating fingers, and ‘squash’ it, rather like flattening a plastic drinking straw. In this sense, it is not the pulse wave that defines the Scallion Stalk pulse, but the actual physical structure of the arterial wall that can be felt regardless of the pressure exerted on it.
This aspect readily reflects the traditional description of an onion or scallion stalk, indicating a distinct and pliable arterial wall but lacking in substance in the interior. In this case, the substance lacking is Blood. The metaphorical description of the pulse used extensively in the traditional literature in this situation is quite apt in conveying the actual sensation of the pulse as felt.
7.5.3.4. Identifying whether the Scallion Stalk pulse is present
Step 1: The Scallion Stalk pulse should be able to be felt with the fingers resting lightly on the surface of the skin, at the superficial level of depth. The pulsation is decreased in strength and the arterial diameter is relatively wide.
Step 2: This involves feeling for the physical characteristics of the artery wall. The arterial wall is well delineated, being able to be felt easily at the superficial level of depth, with fingers resting on the skin surface. When finger pressure is increased from the superficial level of depth downwards, the arterial wall compresses easily and the pulsation is stopped. However, the arterial wall can be easily rolled underneath the fingers, like squashing a plastic drinking straw, so that the walls are still distinctly felt under finger pressure. This requires moving the palpating fingers from left to right, over the arterial wall.
7.5.3.5. Classical descriptions from the Mai Jing and The Lakeside Master’s Study of the Pulse
The scallion stalk pulse is a floating pulse, large but soft. It is empty in the middle but solid at the sides when pressure is applied. [It is said in another version to be a pulse absent under directly under the (feeling) fingers but present at the sides.]
Centre is empty, external is replete [or real, i.e. it exists]
Its shape is like an onion stalk.
7.5.3.6. CM indications
The Scallion Stalk pulse is always considered a pathological pulse quality and is commonly associated with the loss of blood or Yin fluids (Box 7.5Box 7.6 and Box 7.7). While many authors agree that this is usually due to acute haemorrhage, others describe this pulse appearing due to chronic insidious blood loss, Blood vacuity patterns or in chronic illness affecting the haematological system, such as anaemia or leukaemia (Lu 1996).
Box 7.5
Blood vacuity signs and symptoms
• Pale white or sallow complexion
• Dizziness
• Floaters in the vision, also called ‘flowery vision’
• Pale lips, inner rim of the lower eyelid
• Pale nail beds
• Pale tongue, may have orange sides if severe
• Palpitations
• Dry skin
• Insomnia, particularly trouble falling asleep
• Numbness
• Poor memory
Specific signs and symptoms may differ according to the particular organs involved:
• Liver: Dry eyes, muscle cramping, menstrual problems
• Heart: Shen disturbances such depression or anxiety
• Spleen: Tiredness, loss of appetite
Box 7.7
Does profuse loss of body fluids lead to the formation of the Scallion Stalk pulse?
Besides blood loss, the profuse loss of body fluids is sometimes implicated in the development of the Scallion Stalk pulse (Maciocia 2004, Townsend & De Donna 1990). From a CM perspective, when body fluids are seriously depleted, fluids (plasma) from the blood can move from the blood vessels into other body tissues to replace lost fluids. From a biomedical pespective the loss of plasma volume results in a decrease in overall blood volume, and an increase in blood viscosity. The increased proportion of red blood cells adds extra resistance to flow as the red blood cells move against each other and the vessel walls. This extra friction causes the blood flow to become sluggish and therefore more turbulent. It is this characteristic of the blood flow that becomes the main defining aspect of the resulting pulsation. As such we could surmise that the Rough pulse, with its fluctuating pulse force reflecting the sluggish blood flow, will tend to manifest as a result of loss of body fluids, while the Scallion Stalk pulse reflects loss of blood.
Blood vacuity may be due to dietary causes, malabsorption problems or congenital conditions such as pernicious anaemia, thalassaemia or sickle cell anaemia. Anaemia is a complex disease state that can have a number of different causes, affecting both the presentation of the pulse and reflecting the underlying causal factors. Blood vacuity due to iron deficiency anaemia results in a decrease in the number or size of the red blood cells but no loss of plasma volume. This leads to a decrease in the viscosity of the blood that, with regard to the Scallion Stalk pulse, may partially account for the ease with which the pulse is occluded.
Other causes of Blood vacuity include blood loss through various means: vomiting blood (haematemesis), coughing up blood (haemoptysis), gastrointestinal bleeding, uterine bleeding or abnormally heavy menstrual bleeding. In this case both red blood cells and plasma are lost, resulting in a decrease in overall blood volume as well. In addition, the profuse loss of body fluids may also result in the formation of the Scallion Stalk pulse. There are two main patterns that can result in the formation of the Scallion Stalk pulse both reflecting Blood vacuity but due to different causes. These are:
• Acute: Blood loss due to haemorrhage
• Chronic: Chronic blood loss, vacuity of Blood or Kidney Essence.
Acute, following severe loss of blood (haemorrhage)
From a CM perspective, the acute loss of blood results in an artery that feels ‘empty’ due to the decreased volume of circulating blood and is therefore easily occluded. Yang Qi, which is normally anchored and stabilised by Yin blood, moves upwards and outwards causing the pulse to become strongest at the superficial level of depth. Yang Qi becomes relatively hyperactive, having lost the calming aspect of the Yin, leading to an increase in arterial wall tension. This leads to the distinctive arterial wall.
Major blood loss can lead to ‘Qi deserting with the Blood’ (Wiseman & Ellis 1996: p. 151) and may be accompanied by decreased blood pressure, cold sweats or even sudden loss of consciousness.
Chronic: vacuity of Blood or Essence
Vacuity of Blood can occur via the chronic loss of blood due to bleeding from the gastrointestinal tract (for example, ulcerative colitis, stomach ulcers, Crohn’s disease or coeliac disease), chronic nosebleeds, abnormal uterine bleeding, haemoptysis or blood in the urine. Although the daily loss may be small in quantity, consistent loss of blood may lead to the body being unable to produce enough blood (haemoglobin to compensate adequately for the continual loss.
Blood vacuity may also occur due to problems with the organs that are involved in blood production such as the Spleen, Heart or Kidneys, so that sufficient blood is not produced. As these organs are also important in the production of Qi, concurrent Qi vacuity signs and symptoms may be present. The Liver helps to replenish blood, so Liver disharmony may also affect the quality of blood.
Chronic illness of any kind can affect the production of both Qi and blood, so that blood and Qi are not replenished. Kidney Yin vacuity can lead to vacuity of Kidney Essence, which in turn affects blood production and nourishment.
7.5.3.7. Biomedical and clinical perspective
The Scallion Stalk pulse can present as a result of:
• Acute blood loss
• Chronic blood loss or reduced iron intake.
Acute blood loss
The Scallion Stalk pulse may be seen in patients following blood loss, usually due to an acute situation. This may result from physical trauma or non-trauma-related blood loss such as acute gastrointestinal bleeding, for example a perforated ulcer. This may cause hypovolemic shock, referring to the decrease in blood volume due to loss of blood (hypovolemic shock also refers to the loss of plasma that may occur due to severe burns, intestinal blockage or the excessive loss of body fluids due to profuse sweating, vomiting, diarrhoea or urination) (see Box 7.6 for further information).
The term ‘shock’ refers to ‘an inadequate cardiac output that results in a failure of the cardiovascular system to deliver enough oxygen and nutrients to meet the metabolic needs of body cells’ (Tortora & Grabowski 1996). As previously discussed in section 7.4.2, there are three stages of shock. The Scallion Stalk pulse may possibly arise following either a small amount of blood loss or with increased blood loss (Box 7.7).
If blood loss is less than 10% of total volume then this is known as nonprogressive shock and compensatory mechanisms are initiated in the period after the blood loss to return blood volume back to normal (see Box 7.8). This includes the absorption of fluids from the interstitial spaces and intestinal tract. Although this is helpful in increasing the plasma volume back to normal (which takes 1-3 days), it does not compensate for the loss of red blood cells, which may take 3-6 weeks to return to normal. Therefore, following nonprogressive blood loss the red blood cell concentration is low while plasma volume returns to normal fairly quickly. This results in posthaemorrhagic anaemia and may help explain why the pulsation is more easily occluded as the blood flow is less dense (lower proportion of red blood cells) and has a decreased viscosity (‘thinner’ in consistency). This has a number of effects: a decrease in peripheral resistance so blood flow is increased; peripheral vasodilatation to increase blood flow through the tissue because of decreased oxygen supply to tissues due to decreased red blood cell concentration. These both result in more blood returning to the heart and an increased cardiac output. This may cause the pulse to be more readily palpated at the superficial level of depth, have a wider diameter than usual and be more readily occluded.
Box 7.8
Body’s response to hypovolemic shock
Nonprogressive shock (compensated shock)
There are certain initial compensatory mechanisms that occur in response to hypovolemic shock to attempt to restore the body’s homeostasis, return cardiac output and arterial blood pressure to normal. This includes activation of the sympathetic nervous system and the release of the certain substances that increase heart rate, cardiac contraction and the secretion of certain hormones such as aldosterone and antidiuretic hormone (ADH) that help to retain water and increase vasoconstriction to increase blood volume and blood pressure. This process starts immediately and may continue up to 48 hours if necessary.
Some of the factors than come into play when there is blood loss include the following effects on the circulatory system (Guyton & Hall 2006: p. 279-281):
• Immediate (within 30 seconds): Sympathetic reflexes that cause vasoconstriction of vessels throughout the circulatory system.
• Within 10 to 60 minutes:
– Release of angiotension and vasopressin, substances that help to constrict peripheral arteries and veins to increase water retention by kidneys.
– A reverse stress-relaxation of the circulatory system causes the blood vessels to contract down around the decreased volume in order to make it fill the circulartory system more appropriately.
• Longer term (within 1 to 48 hours): Replacing the fluid loss via absorption from the interstitial spaces and intestinal tract and stimulation of thirst and increased desire for salt.
If blood loss is more severe, dropping by more than 15% of total volume, then the normal compensatory mechanisms are not sufficient and urgent medical intervention to replace fluids lost is required to return blood volume to normal. This is known as progressive shock, and cardiac output falls dramatically, which is worsened by the instigation of positive feedback cycles. Due to the decreased cardiac output, the heart muscle becomes ischaemic, leading to even lower output and blood pressure. This in turn adversely affects the activity of the vasomotor centre in the brain that controls vasoconstriction. This leads to generalised vasodilatation of blood vessels. The pulse is forceless due to the decreased cardiac output, the arterial width is increased due to vasodilatation and is easily occluded due to the lack of volume in the arterial system and hence, the Scallion Stalk pulse manifests.
The increased arterial wall tension that results in the distinctive pliable arterial wall of the Scallion Stalk pulse (as previously discussed in section 7.3.5) occurs due to tension in other parts of the arterial wall structure, not from contraction of vascular smooth muscle. In fact, the artery wall is in a state of vasodilatation because of the blood loss.
The Guangzhou College notes (1991) state that the Hollow (Scallion Stalk) pulse has been shown to appear experimentally when blood loss is both rapid and heavy (>400 ml) and when the usual compensatory reflexes of vasoconstriction have not resulted in strong contraction of the blood vessels (no specific research study has been cited).
Chronic blood loss or reduced iron intake
Chronic blood loss may result in anaemia, occurring over a period of time due to the body’s inability to absorb enough iron from the intestinal tract (mainly the small intestine) to replace the lost haemoglobin. This can result in the production of smaller red blood cells containing insufficient haemoglobin. A loss of 2-4 ml of blood per day is enough to cause iron deficiency anaemia (McCance & Huether 2006: p. 934). Chronic disease such as chronic inflammatory disease, HIV/AIDS, hepatitis and chronic renal failure may also result in anaemia due to alterations to iron metabolism, red blood cell life span, and blood cell production in the bone marrow (McCance & Huether 2006: Ch. 26).
Chronic blood loss may occur due to occult bleeding such as gastrointestinal tract bleeding from ulcers, inflammatory bowel disease, coeliac disease, carcinoma or a range of other gastrointestinal complaints. In addition, menorrhagia (heavy menstrual bleeding) or abnormal uterine bleeding may also contribute to blood loss.
Alternatively, there may be inadequate dietary sources of iron resulting in anaemia due to general decreased food intake, specific dietary restrictions (for example, restrictions on meat) or problems with iron absorption such as coeliac disease or other inflammatory intestinal disease.
As noted by Guyton and Hall (2006), anaemia has a systemic effect on the circulatory system. In anaemia, it is the lowered proportion of red blood cells to plasma volume that results in a decreased blood viscosity. This in turn has a positive effect on the peripheral resistance to blood flow, resulting in an increased amount of blood flowing through the tissues and returning to the heart. The increased blood flow to the heart results in increased cardiac output, which is further enhanced by vasodilatation of peripheral blood vessels due to decreased oxygen supply to tissues (hypoxia). The rate of blood flow also increases. In other words, the cardiovascular system, particularly the heart, has to work much harder to continue to supply the body with sufficient oxygen and nutrients and transport metabolic waste products to be eliminated.
Over time this can have a detrimental effect on the heart, leading to eventual cardiac failure if the underlying cause of anaemia is not addressed. In severe anaemia, the cardiac output may be raised to as much as three or four times normal levels (Guyton & Hall 2006: p. 427).
From a CM perspective, such physiological changes are represented in the pulse by:
• Increased pulse width due to both the peripheral vasodilatation and increased cardiac output
• Distinct presence of the pulse at the superficial level due to the increased cardiac output
• Easy occlusion due to the decreased viscosity and therefore density of blood flow (reflecting the underlying vacuity of blood).
Recent research has shown that Helicobacter pylori, bacteria commonly implicated in digestive dysfunction such as duodenal and stomach ulcers, may also lead to iron deficiency anaemia (Russo-Mancuso et al. cited in McCance & Huether 2006: p. 934). H. pylori has been shown to impair iron absorption (Ciacci et al. cited in McCance & Huether 2006: p. 934). This has an interesting correlation with CM theory, where impaired functioning of the Spleen and Stomach, integral to digestive functioning, can also lead to the impaired production of both blood and Qi.
7.5.4. Drumskin pulse (Gé mài) 
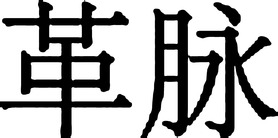
With the Drumskin pulse, it is the physiological characteristics of the arterial wall that are of primary interest, in particular the significant increase in arterial wall tension, in conjunction with the lack of force.
7.5.4.1. Alternative names
Leather, Tympanic, Leathery or Leather-like pulse.
7.5.4.2. Requisite parameters
The Drumskin pulse is a complex pulse quality with changes in five pulse parameters:
• Arterial wall tension: The Drumskin pulse has increased arterial tension
• Depth: The pulse can be felt relatively strongest at the superficial level of depth
• Width: There is an increase in the arterial width from normal, resulting in a wide pulse
• Pulse occlusion: The Drumskin pulse can be easily occluded with heavy pressure
7.5.4.3. Clinical definition
The Drumskin pulse has a wide arterial diameter, so a large surface area is displaced laterally on the fingertip with each pulsation. The Drumskin pulse has a greatly increased arterial tension so that on light palpation the arterial wall feels extremely tense and rigid. Given this, the arterial wall has strong initial resistance to light finger pressure, but with increasing pressure the pulse is easily occluded. This is facilitated by the decrease in blood volume. This also affects the intensity of the pulsation, resulting in a forceless pulse. The Drumskin pulse is felt as a length of pulsating artery, as opposed to distinct wave-like pulsations due to the effect of increased tension in the arterial wall.
When the Drumskin pulse is described in the pulse literature, it is commonly equated with both the Stringlike (Wiry) pulse and Scallion Stalk pulse. For example, Li (Flaws (trans) 1998: p. 103) describes the Drumskin pulse as ‘bowstring and scallion-stalk’ while Lu (1996) says the pulse is ‘felt hard on its walls but hollow in the centre’. Accordingly, we can surmise from this that the important features of the Drumskin pulse relate to:
• Increased arterial wall tension (a common feature of the Stringlike and Scallion Stalk pulse also)
• Decreased volume of either Blood or Yin fluids (common to both the Scallion Stalk pulse and Drumskin pulse), resulting in its forceless pulsation and easy occlusion.
The differentiating feature between the Drumskin pulse and the Scallion Stalk pulse is the degree of increased arterial wall tension: the Drumskin pulse has significantly more tension in its arterial wall, resulting in a more rigid and less pliable artery wall than the Scallion Stalk pulse. Additionally, unlike the Drumskin pulse, the distinct arterial wall is still felt in the Scallion Stalk pulse even when the pulsation within the artery is occluded.
The description and indications for the Drumskin pulse in The Lakeside Master’s Study of the Pulse are comparatively brief in relation to that of many of the other pulse qualities. This suggests that it only occurs in quite defined situations (as opposed to some of the other pulses that may be seen in a number of different scenarios) and therefore this pulse quality is not commonly seen.
There are also relatively few references to the Drumskin pulse in the Mai Jing and these are generally repeated throughout. The Mai Jing’s description of the Drumskin pulse is identical to more recent definitions of the Firm pulse, being ‘replete, large, and long as well as a little bowstring’ and somewhat like the deep pulse’. The commentary in the text notes that this is suspected to actually be the Firm pulse rather than the Drumskin pulse (Wang, Yang (trans) 1997: p. 4). If this is the case, the Drumskin pulse, in its current form, was not included as one of the 24 pulse qualities mentioned in the Mai Jing.
However, an examination of the Mai Jing (Wang, Yang (trans) 1997: p. 343) reveals a further reference to a pulse that is described as ‘bowstring and large’, further explained as ‘modulated bowstring’ (as opposed to ‘pure bowstring’) and ‘not so large as scallion stalk’. Pointing out that modulated bowstring indicates cold and scallion stalk means vacuity, the author notes the interaction of these two results in the pulse becoming ‘drumskin’. This description closely resembles the definition of the Drumskin pulse as it is known today. Pathogenic Cold has a contracting effect (that is, a vasoconstricting effect on the arterial wall) which may explain why it is described as being not as large (wide) as the Scallion Stalk pulse.
7.5.4.4. Identifying whether the Drumskin pulse is present
Step 1: The Drumskin pulse can be felt relatively strongest at the superficial level of depth, with fingers resting gently on the surface of the skin above the radial artery. However, of primary interest is the significant tautness of the arterial wall. The arterial wall is relatively wide, displacing a wide surface area of the palpating finger. The overall pulsation is forceless.
Step 2: With increasing finger pressure the arterial wall initially resists deformation, maintaining its tenseness. However, as finger pressure is further increased the arterial wall gives in easily, as there is decreased internal resistance within the artery due to the decreased volume of fluids. The pulsation can be completely occluded.
7.5.4.5. Classical description from The Lakeside Master’s Study of the Pulse
Drumskin pulse, bowstring and scallion-stalk
(Zhong-jing).
Like pressing the skin of a drum
7.5.4.6. CM indications
Although the Drumskin pulse is always considered to be a pathological pulse quality, there is some disagreement in the pulse literature over its aetiology. There is general consensus about blood or fluid loss being the main causal factor, but some authors indicate that this can be complicated by pathogenic Cold, resulting in the greatly increased tension in the arterial wall. There are three main patterns and both are associated with an underlying vacuity of Yin fluids or blood:
• Acute profuse Yin fluid loss
• Chronic disease leading to severe vacuity of Yin and Essence
Acute: vacuity of Yin fluids complicated by EPA of Cold
This acute pattern of an EPA of Cold occurs on top of an underlying vacuity of body fluids or blood loss. The causes of this blood or body fluid loss are varied and have been discussed previously in the section on the Scallion Stalk pulse. The Drumskin pulse could be interpreted as a further development of the Scallion Stalk pulse, due to the complication of an EPA of Cold.
If the Drumskin pulse is seen in a relatively new illness, this is seen as less critical and therefore has a good prognosis.
• Mechanism of pulse formation: The external pathogenic attack causes the pulse to become relatively stronger at the superficial level of depth as Zheng Qi (antipathogenic Qi) moves to the exterior to fight the pathogen. However, because of the underlying vacuity, the Zheng Qi is not strong and the overall pulse intensity is forceless. The contracting nature of the Cold pathogen causes strong contraction of the arterial wall, thereby greatly increasing arterial wall tension. The underlying loss of Yin fluids enables it to be easily occluded.
From a biomedical perspective, the Drumskin pulse (similarly to the Scallion Stalk pulse) has increased arterial tension but not only due to vasoconstriction (smooth muscle contraction). Due to the loss of blood there is compensatory vasodilatation (relaxation of vascular smooth muscle), so tension/stress in the arterial wall is transferred to other structures within the wall. The additional complication of pathogenic Cold stimulates the body’s attempts to maintain warmth, thereby activating vasoconstriction of the arterial walls which has an additive effect on the tension already in the arterial walls, hence the extremely ‘hard’ presentation of the artery on palpation.
Acute profuse Yin fluid loss (Blood, Essence, body fluids)
The Drumskin pulse may be seen in patients with an acute profuse loss of Yin fluids due to haemorrhage, excessive sweating, diarrhoea or vomiting.
• Mechanism of pulse formation: In this case the pulse can be palpated relatively strongest at the superficial level of depth because the severely decreased Yin can no longer restrain or anchor Yang Qi, which naturally moves upward and outward. This causes Yang Qi to float, becoming more superficial. The extremely vacuous Yin also results in a hyperactivity of Yang Qi, leading to the increased arterial wall tension. The vacuity of Yin fluids enables it to be easily occluded.
• Clinical relevance: The Drumskin pulse is usually associated with blood loss and in the pulse literature a number of authors (Deng 1999, Li, Flaws (trans) 1998, Lu 1996) note its appearance in abnormal uterine bleeding or miscarriage leading to continuous uterine bleeding in women. The Drumskin pulse can appear postnatally due to abnormal bleeding. Following childbirth, failure of the uterus to contract to compress the uterine blood vessels and stop flow to the placenta can result in primary postpartum haemorrhage. Retention of part of the placenta may also result in abnormal uterine bleeding (Guangzhou Chinese Medicine College 1991) and may be a possible cause of secondary postpartum haemorrhaging, occurring anywhere from 24 hours to 12 weeks postnatally (Stables & Rankin 2005: pp. 575-578).
• In men, the Drumskin pulse may be associated with deficiency of Kidney Essence (associated with lower back pain, nocturnal emissions and other Kidney signs).
Chronic: severe Blood/body fluid loss or Kidney Essence (Jing) consumption due to chronic disease.
The Drumskin pulse may also appear in the course of chronic illness. This is seen as a critical worsening of the disease, indicating the increasing severity of vacuity of blood, body fluids or Kidney Essence, and therefore is considered to have a bad prognosis. The mechanism is similar to the previous pattern.
7.5.5. Scattered pulse (Sàn mài) 

Of primary interest in the Scattered pulse is the physiological presentation of the arterial wall (or rather, the lack of presentation in this case).
7.5.5.1. Alternative names
Dissipated or Diffusing pulse.
7.5.5.2. Requisite parameters
The Scattered pulse is a complex pulse quality differentiated by its lack of arterial wall definition. There are changes in five pulse parameters:
• Arterial wall tension: The Scattered pulse has a marked decreased in arterial wall tension.
• Force: There is a decrease in the overall forcefulness of the pulse.
• Depth: The Scattered pulse is felt relatively strongest at the superficial level of depth.
• Pulse occlusion: The Scattered pulse is very easily occluded with pressure.
7.5.5.3. Clinical definition
The Scattered pulse is primarily characterised by its lack of arterial wall tension, presenting with an arterial wall that is virtually indistinguishable on palpation (Fig. 7.3). This marked reduction in the arterial wall tension results in difficultly clearly differentiating the boundaries between the arterial wall and the surrounding connective tissue. The Scattered pulse has a wide arterial diameter. Lacking force, it is palpated as an area of pulsating tissue. It is considered to be a pulsation without form and is easily occluded with finger pressure.
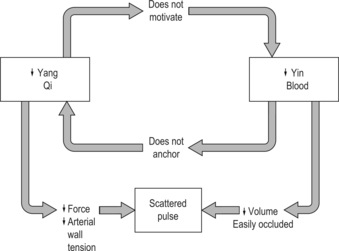 |
| Figure 7.3The development of the Scattered pulse. |
7.5.5.4. Comparison of definitions
While there is general agreement in the CM pulse literature regarding the main features of the Scattered pulse, its lack of arterial wall definition and general lack of force of pulsation, there are a number of other features that cannot be agreed on. The Scattered pulse is commonly described as a ‘large’ pulse, but this could be interpreted in a number of ways. It could be a reference to the overall forcefulness of the pulse (which is highly unlikely, as it is a vacuity-type pulse) or it could refer to the width of the arterial wall (most likely). Deng (1999), Flaws (1997), Li (Flaws trans) (1998) and Maciocia (2004) are some of the authors who refer to the appearance of the Scattered pulse at the superficial level of depth. In this respect it is considered to be ‘without Root’, being represented at the exterior but not present in the interior, and enabling it to be completely occluded with heavy pressure. All four authors have drawn from traditional pulse descriptions in the Mai Jing, which could account for the similarities in their descriptions of the Scattered pulse.
A clear description of the Scattered pulse in the classical texts is difficult to find. In the Mai Jing, the term ‘scattered’ is used as a descriptor of other pulse qualities. For example, in the first chapter describing 24 separate pulse qualities, ‘scattered’ is used in both the description of the ‘choppy’ and ‘dissipated’ pulses (Wang, Yang (trans) 1997: p. 4). As noted by Hammer (2002: p. 62), there is no explanation of the term ‘scattered’ so we do not know exactly in what context it is being used. Although the ‘scattered’ pulse is not a designated pulse quality in the Mai Jing, the ‘dissipated pulse’ resembles the Scattered pulse described in other CM pulse literature.
However the Scattered pulse is also variously described as ‘uncountable, uneven in rhythm, uneven in rhythm, showing no sign of pause’ (Guangzhou College notes, 1991), ‘large and irregular’ (Amber & Babey-Brooke 1993) and ‘feels as if it were “broken” into many tiny dots instead of flowing smoothly’ (Maciocia 2004). These references to the irregularity of pulse rhythm appear to support the concept of extreme Qi and Blood vacuity affecting the heart’s functional capacity to contract effectively, confirming the seriousness of the condition. One wonders why then is this pulse not included as a subdivision of the rhythm pulses? It would seem that the presence of arrhythmia is dependent on whether there is Heart involvement in the pattern, but is not an essential characteristic of the Scattered pulse quality. Rather, if irregularity of rhythm does occur then this indicates the extreme severity of the condition and would be identified as a change in an additional pulse parameter, rather than identifying it solely as the Scattered pulse.
Li (Flaws (trans) 1998: p. 110) has a number of descriptions for the Scattered pulse, including the phrase ‘Or it may come many and depart few’ (our emphasis). This description could possibly refer to the manifestation of what is known in biomedicine as pulse deficit, which occurs when premature ventricular contractions (before the heart is properly filled) lead to a greatly decreased stroke volume so that the pulse wave cannot be felt at the radial artery. This results in a greater number of apical beats (as measured at the heart) compared to that felt in the radial pulse (Guyton & Hall 2006: p. 150).
The varying descriptions seem to imply that the Scattered pulse has possibly more than a single presentation, depending on the actual pattern of disharmony. This appears to be supported by Deng (1999: p. 105) who says ‘Clinically, there ought to be close investigation of the changes in the disease circumstances.’
In fact, it is to be expected that the Scattered pulse will not be a commonly seen pulse in the average CM clinic, being usually seen in someone who is extremely sick. It must be remembered that many of these CM pulse qualities were originally developed hundreds of years ago, where the local acupuncturist or herbalist was the primary or sole provider of health care. Patients with a diverse spectrum of illnesses, ranging in chronicity and severity, would have been seen in their clinics. Correspondingly, a wide range of pulse qualities reflecting these differing health problems would have been observed. Today, in modern societies especially, the local general practitioner or hospital is the primary provider of healthcare, and some of the more extreme pulse qualities reflecting critical or severe illness are less likely to be seen in the CM clinic, and more likely to be encountered in a hospital ward or intensive care unit.
On the other hand, the increasing interest in ‘alternative’ or ‘complementary’ health services has also seen an increase in patients with more chronic or severe illnesses in CM clinics. Therefore the ability to recognise these CM pulse qualities and understand what they mean in terms of the effect of the disease process on Qi, Blood, Yin and Yang becomes ever more important.
7.5.5.5. Classical description from Mai Jing and The Lakeside Master’s Study of the Pulse
The dissipated pulse is a large yet scattered pulse. The dissipated pulse is an indication of Qi repletion but blood vacuity, presence (i.e., repletion) in the exterior but absence (i.e., vacuity) in the interior.
Its edges are scattered and not restrained …
Departs and comes without definitude
7.5.5.6. CM indications
The Scattered pulse is considered to be a vacuity-type pulse, often associated with severe vacuity. Therefore, it can be seen in patterns such as:
• Severe vacuity of Qi and Blood
• Vacuity of Yuan Qi.
Severe vacuity of Qi and Blood
The Scattered pulse is a sign of severe disease, reflecting a severe vacuity of Qi, Blood, Yin and Yang. This may be due to chronic illness that, over time, consumes these substances, reflecting increasing vacuity of the organs involved in the transformation and transportation of Qi and blood, including the Spleen, Stomach, Lung, Kidney and Heart.
The Kidneys are considered to be the source of both Yin and Yang for the entire body, providing both the motive and nourishing aspects that support health. Therefore if Kidney function is affected, over time this can affect the functioning of all organs.
Severe vacuity of Yuan Qi or Kidney Qi
Yuan Qi provides the motive force for all the functional activity in the body. If this is exhausted, then Yang Qi will also be adversely affected. Yang Qi maintains the normal arterial wall tension. If Yang Qi is deficient then the arterial wall loses definition, blurring the boundaries between the artery and surrounding tissue.
• Clinical relevance: It is generally accepted that if the Scattered pulse is seen in a chronic or serious illness, this has a poor prognosis as it indicates a critical worsening of the condition.
The Scattered pulse may also be seen in pregnant women, during the birthing process or as a sign of impending delivery (Deng 1999, Li, Flaws (trans) 1998, Lu 1996). While this is seen as a normal occurrence by some authors, with one interpretation being that it is a sign of the ‘outgoing of Qi and blood in order to give birth’ (Lu 1996: p. 118), Maciocia (2004) states that it may signify a prolonged and difficult labour. In addition its appearance during the course of pregnancy may also be pathological, associated with the risk of miscarriage (Li, Flaws (trans) 1998, Maciocia 2004).
7.5.5.7. Biomedical perspective
The Scattered pulse may occur as a result of neurogenic shock, a type of circulatory shock that occurs without any loss of blood volume. This can occur when there is a sudden loss of vasomotor tone throughout the body (Guyton & Hall 2006: p. 285). It is seen as the imbalance between parasympathetic and sympathetic stimulation of the smooth muscle in the blood vessels. As a result, extensive vasodilatation occurs, resulting in an increase in the vascular capacity so that the normal amount of circulating blood becomes inadequate to fill the circulatory system. This causes a decrease in the mean systemic filling pressure, which in turn leads to decreased venous return to the heart and resultant decreased cardiac output.
Neurogenic shock may occur as the result of trauma to the spinal cord, deprivation of oxygen to the medulla, depressant drugs, anaesthesia or severe emotional stress and pain (McCance & Huether 2006: p. 1629).
The vasodilatation and the lack of vasomotor tone are reflected in the distinct lack of tension in the radial arterial wall, and the lack of force is reflected in the decreased cardiac output.
As noted by Wiseman and Ellis (1996; p. 118), the appearance of the Scattered pulse ‘indicates the dissipation of Qi and blood and the impending expiry of the essential Qi [essence] of the organs.’ It is usually attended by other critical signs. From a biomedical perspective the Scattered pulse may be seen at the end stage of severe heart disease (Lu 1996: p. 110). This reflects the inability of the heart to contract effectively, leading to impaired circulation.
7.6. Pulse force
Pulse force is the most complex of all the pulse parameters because it depends on a range of variables such as the strength of cardiac contraction, blood volume and the tensile compliance of the arterial wall. It is how these variables interact at any given point in time that determines pulse force; a change in any one of these variables will cause a corresponding change in the overall pulse intensity and thus the perception of pulse force.
The parameter of pulse force is used to provide clinically useful information for both diagnostic and prognostic purposes and so is integral to further pattern differentiation, even when pulse force is not a requisite parameter for the CM pulse quality involved, or the pulse parameters do not form a recognisable CM pulse quality. A good example of this concept is using pulse force for differentiation of Yin vacuity Heat and an EPA Heat. Both patterns present with Heat signs and symptoms and so may have an accompanying increase in pulse rate, and so the Rapid pulse can form (>90 bpm). An increase in pulse rate or even the Rapid pulse provides information only in respect to the fact that Heat is present, but does not indicate whether the Heat is arising from a vacuity process (Yin vacuity) or a replete process (EPA Heat). Rather, accompanying changes in the pulse force should correspond with the process occurring; a forceful pulse usually indicates repletion (excess) while a forceless pulse generally indicates vacuity (deficiency), and so Yin vacuity Heat can be differentiated from an EPA Heat by assessing pulse force.
There are six CM pulse qualities that can be classified primarily according to the parameter of pulse force:
• Replete pulse (section 7.7.1)
• Firm pulse (section 7.7.2)
• Vacuous pulse (section 7.7.3)
• Faint pulse (section 7.7.4)
• Weak pulse (section 7.7.5)
• Soggy pulse (section 7.7.6).
These are complex pulse qualities, ranging from those that are abnormally forceful to those that have a decreased pulse force or can barely be perceived. They are differentiated further by changes in a number of other pulse parameters, but are most distinctly defined by the change in pulse force.
7.6.1. Differentiating between specific and descriptive terminology
Terminology such as ‘replete’, ‘full’, ‘vacuous’ ‘empty’ and ‘weak’ is often used interchangeably in the CM literature. The terms are used to describe changes in pulse force and used generically to identify the overall nature of an illness (or pattern), whether vacuous or replete. Unfortunately, these terms are also used to name specific CM pulse qualities. When used in this way the terms have a greater range of diagnostic meaning than when used as generic descriptors of illness and dysfunction. For example, a pulse that hits the finger with decreased intensity may be described as ‘weak’. Thus it is inferred that a general vacuity pattern is occurring. This is not to be confused with the traditional CM pulse quality, the Weak pulse, which encompasses more than just a change in pulse intensity in its definition. That is, although the Weak pulse has a decrease in intensity (also inferring a vacuity pattern), it is also defined/noted as having changes in pulse width (it is thin) and is located at a specific level of depth (felt strongest at the deep level of depth and cannot be felt at the superficial level of depth). As such, the Weak pulse provides more specific information, not only about the nature of the disharmony (by the force), which is further specified by the pulse width, but also the location of the disharmony (via the level of depth).
This means that to avoid confusion and incorrect interpretation terms need to be distinguished or contextualised on whether they are being applied generically as descriptive terms, or specifically as diagnostic terms for specific CM pulse qualities. Clinically, this means that considered choices should be made to always use correct terminology always. This is paramount when there are several practitioners operating from the one clinic, or when several practitioners regularly confer, so terms are not misinterpreted or wrongly applied.
7.6.2. Pulse force and its assessment
The method for assessing pulse force requires evaluation of the intensity of the radial artery’s pulsations hitting the palpating fingers. This is done by assessment of:
• Amplitude of the pulse wave
• Strength of cardiac contraction (and so the time taken for the pulse to reach maximum pulse amplitude)
• Contact area of artery being touched with the fingertips.
In assessing pulse force, the level(s) of depth where the pulse is most apparent need to be first identified. This is done by applying pressure simultaneously with all three fingers over the three pulse positions and varying the amount of pressure to examine each of the three levels of depth. This process is termed assessment of the relative strength, the level of depth where the pulse is felt most strongest, irrespective of whether the pulse is forceful, forceless or neither. (Sometimes two or all three levels of depth are similar in their level of strength.) Note should also be made of the presence or absence of the pulsation beyond Cun and beyond Chi pulse positions, as this can help in determining whether the pulse is forceful or not.
Once the level(s) of depth and positions are identified where the pulse is most apparent, then the assessment of the actual force of the pulse can be made. This is assessment of the overall force: the force reading which is used to identify several of the traditional CM pulse qualities. (Assessment of overall pulse force needs to be distinctly differentiated from assessment of relative force. Relative force refers to the ‘subtle’ comparative assessment of differences in strength between positions, levels of depth or left and right arms. That is, irrespective of whether the pulse is forceful, forceless or neither, one side or position may be relatively stronger than the other (King et al 2002: p. 153). This concept and related application in different pulse assumption systems is discussed further in Chapter 9.)
There are two basic subdivisions of pulse force:
• Forceful
• Forceless.
Forceful
A forceful pulse is defined as having a large pulse pressure wave or amplitude, with the change in pressure occurring rapidly so that the pulse strikes the finger strongly and displaces a wide surface area on the fingertip (Fig. 7.4). It is defined as being forceful in at least two of the three traditional pulse positions and with the pulse likely to be apparent in the beyond Chi and/or beyond Cun pulse positions.
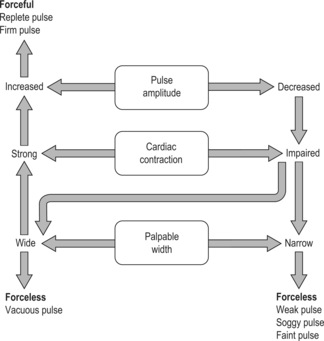 |
| Figure 7.4Factors affecting the formation of forceful and forceless pulses. |
Forceless:
A pulse that is forceless is defined as either:
• A small pulse pressure wave (amplitude) striking the fingertip weakly with a small displacement of area on the fingertip; or
• A slow rate of change in the pressure pulse wave (amount of time required to reach maximum amplitude) and a wide displacement of surface area on the fingertip.
7.6.2.1. Additional palpatory technique for assessing force
When evaluating pulse force the assessment of the pulse parameter ‘ease of pulse occlusion’ can provide useful information. Occlude the pulse and check whether the pulsation can still be felt at the proximal (body) side of your ring finger (positioned at the Chi position). This is not a failure to occlude the pulse but rather is due to the pulse waves hitting the barrier (your finger) that has blocked their normal pathway of progression along the radial artery. When a forceful pulse is present then a pulsation can still be apparent on that side of the finger.
When the pulse is very forceful, then pulse occlusion may be very difficult to achieve as well, especially at the Chi position.
7.6.2.2. A pulse that is neither forceless nor forceful
A pulse that presents as neither forceful nor forceless is often of no consequence in either the identification of some pathological CM pulse qualities or pulse assessment using the pulse parameters. Indeed, a pulse that is neither forceless nor forceful would usually be considered to be a ‘normal’ pulse presentation of this parameter.
The exception is when the ‘neither’ pulse force is either weaker or stronger than the individual’s usual pulse force. If the individual’s pulse is weaker than it usually is, then this may be seen as a sign of weakening Qi or Yang but does not necessarily mean that the Yang or Qi is definitively vacuous. Transient factors such as a poor night’s sleep or hunger can often cause such temporary decreases in pulse force.
Similarly, if the pulse force for an individual has been forceless but starts to increase in intensity, then this can be viewed as a sign of improvement, a good prognostic sign (so long as it is not accompanied by adverse changes in other pulse parameters or other signs and symptoms).
7.6.2.3. Differences between left and right radial arteries
Assessment of the overall force of the pulse should be compared between the left and right arteries, either individually or with simultaneous bilateral palpation. If there is a significantly large discrepancy in force between the two sides (10-15 mmHg), the decreased pulsatile flow may be the result of arterial narrowing or occlusion (McCance & Huether 2006: p. 1069). (From a CM perspective more subtle differences relate to the Qi and blood balance and are discussed in Chapter 9.)
7.6.3. Regulation of pulse force: CM perspective
Pulse force is intrinsically linked with both Qi and Blood and their inter-relationship of function and form. Sufficient Qi is required to cause the blood to move in the vessels, longitudinally through the length of the arteries but also laterally, expanding the arterial wall. This relates to the heart’s functional capacity to contract, thus Heart Qi, and the strength of that contraction, which is Yang force. For example, if Yang is vacuous then the heart contraction is weak and relatively slow and the pulse is felt without force. If Qi is weak then the heart’s functional ability to contract at all is affected and so the rhythm becomes irregular. In this sense, Qi initiates function while Yang is the expression of the Qi’s strength.
A pulse without force can also arises when the blood is vacuous. This is because blood is the medium for conducting the pulse force or Yang Qi throughout the body. When blood is vacuous, then Qi has nothing to act on and so Qi cannot interact physically with the pulse, and pulse force (Yang) is consequently felt diminished. As is often the case when blood levels fall, pulse pressure also falls and this is subsequently felt as a decrease in pulse amplitude and subsequently decreased pulse force. Conversely, when blood is abundant then the pulse will be felt forceful so long as the Qi and Yang are also abundant.
In this context, pulse force is affected when Qi and blood are affected. Changes in pulse force occur as a result of:
• External factors affecting the inter-relationship of Qi and blood; through consumption, damage, agitation or countering Qi and blood’s intrinsic nature
• Internal factors affecting the inter-relationship of Qi and Blood; often involving dysfunction of the mechanisms associated with the production, movement, storage, function and maintenance of these.
7.6.4. Measures of pulse force: biomedical perspective
The force of the pulse refers to the impetus of the arterial pulsation striking the fingertip when the pulse is palpated. This is viewed as pulse amplitude.
7.6.4.1. Pulse amplitude as a measure of pulse force
From a biomedical perspective, the pulse amplitude is equated with pulse strength and pulse volume. The pulse amplitude is defined as the difference between the systolic and diastolic pressures (also known as the pulse pressure) (Box 7.9). On average this is about 40 mmHg (assuming an average blood pressure of 120/80 mmHg) (Box 7.10). It was suggested by O’Rourke et al (1992: p. 19), that:
The amplitude of the palpable pulse depends on the amplitude of the pressure pulse and on the size of the artery palpated … The amplitude of the pulse is thus the manifestation of force – of pressure multiplied by the area of the finger distorted by the pulse.
Box 7.9
Systole and diastole
Systolic pressure
• The pressure in the arteries as blood is pumped from the left ventricle into the aorta
• Affected by stroke volume, force of contraction and elasticity of arterial walls.
Diastolic pressure
• The pressure in the arteries as the heart relaxes and blood flows out of the main arteries and into the arterial system.
• Affected by the peripheral resistance, elasticity of blood vessels and blood viscosity (the higher the viscosity, the more resistance to flow) and also heart rate: the slower the heart rate, the more time there is for blood to flow out of the main arteries therefore decreasing diastolic pressure.
(Stables & Rankin 2005: p. 230)
Box 7.10
Objective measurements of pulse force
Walsh (2003) found that pulses recorded as being forceful using manual palpation in healthy subjects were associated with higher tonometry measurements showing a faster change in pressure with respect to time during systole. This means that maximum pulse amplitude or pulse height of the pulse wave, when achieved in a short period of time, often means more forceful pulses. For example, if the heart contracts strongly, the systolic peak is achieved more rapidly, resulting in a sharper incline to the peak. This causes a greater volume of blood to flow into the aorta at a given point in time. As a consequence, the pulse may feel ‘full’ or have increased pulse wave intensity. Alternatively, either a decrease in blood flow or ejection of the blood from the heart occurring over a longer period of time is associated with decreased arterial pressure and may be felt as either forceless or of ‘normal’ strength. In this situation, ventricular contraction determines the amount of force imparted into the blood forcing it to flow through the vessel.
7.6.5. Regulation of pulse force: biomedical perspective
In general, the greater the difference in amplitude from normal (the larger the pulse pressure) the more forceful the pulse is felt under the finger, and the less divergence from normal, the weaker the pulse.
However, pulse force is also influenced by other factors such as arterial diameter, blood volume and the condition of the arterial walls (Box 7.11). Large amplitudes result in more distinct arterial pulsation because of the large differences in pressure – the larger the difference, the more noticeable any movement in the artery will be.
Box 7.11
Factors affecting pulse pressure
Pulse pressure is affected by:
• Stroke volume (the amount of blood pumped from left ventricle into the aorta)
• Compliance of the arterial system (ability of arteries to accommodate blood flow from the heart)
• The nature of the ejection from the heart during systole.
This means the greater the stroke volume, the larger the amount of blood that needs to be accommodated in the arterial system, therefore the greater the pressure rise and fall: hence a larger pulse pressure (Guyton & Hall 2006: p 173).
When viewed from a mechanical and flow wave perspective the manifestation of pulse force is likely to be due to a number of different pathways dependent on the illness and pathological processes (Box 7.12). The amplitude of the pressure pulse should not be solely mistaken for pulse force: large pulse amplitude does not necessarily mean a forceful pulse or small amplitude a forceless pulse. For example:
• Changes in the arterial wall tension affect the ability of the arteries to expand in response to the pulse wave, so affecting the perception of pulse force. Systolic pressure is raised if the arterial walls are stiff and are unable to expand easily. Consequently pulse force is raised.
• Increased pulse force can result from arterial narrowing or vasoconstriction. When arteries constrict there is less area for the pulse wave to act on, thereby proportionally increasing the pressure exerted from within the artery.
Box 7.12
Biomedical conditions associated with changes in pulse pressure from the norm
Decreased pulse pressure may indicate:
• ↓ stroke volume due to cardiac tamponade, shock, tachycardia (decreased ventricular filling time)
• ↑ peripheral resistance due to cardiac or aortic dysfunction such as aortic stenosis, mitral valve problems, cardiac tamponade.
Increased pulse pressure may indicate:
• ↑ stroke volume due to aortic regurgitation (blood flowing back into left ventricle from the aorta after it has emptied)
• ↓ peripheral resistance and therefore ↑ peripheral vasodilation (therefore ↑ blood volume returning to the heart and ↑ cardiac output): fever, anaemia, hyperthyroidism, exercise, arteriovenous shunt (abnormal fistula between major artery and vein).
(Estes 2006: p. 263)
7.6.5.1. Other factors affecting pulse force
Duration of systole and diastole
The perception of pulse force is also affected by the proportion of time the heart is in systole and diastole, which affects the volume of blood ejected into circulation by the heart (stroke volume). It is also affected by pressure indices affecting the end-systolic volume in the ventricles and so strength of heart contraction.
Autonomic nervous system
The activation of the sympathetic or parasympathetic nervous system affects the heart, leading to changes in cardiac output (see Box 7.13 for further information).
Box 7.13
Effects of the sympathetic and parasympathetic nervous system on cardiac function
Sympathetic stimulation
• ↑ strength of heart contraction and therefore stroke volume
• ↑ heart rate up to 180-200 bpm or more
This leads to an increase in cardiac output up to 2-3 times normal.
Parasympathetic stimulation
• ↓ heart rate to 20-40 bpm
• ↓ strength of cardiac contraction by 20-30%
The overall effect is to decrease cardiac output by 50%, a milder effect than the sympathetic response.
(Guyton & Hall 2006: pp. 112-113)
Body temperature and pulse force
Changes in body temperature due to either environmental conditions or disease can affect both the heart rate and, to a degree, the contractility of the heart. Changes in body temperature alter the rate of electrical discharge in the heart (Stables & Rankin 2005: p. 225).
A moderate increase in body temperature can increase the strength of cardiac contractility, therefore increasing the perceived force of the radial arterial pulsation. However, if this is prolonged it has an adverse effect on cardiac metabolic functioning resulting in eventual impaired cardiac function and therefore weaker contractions.
If the heart rate is greatly increased, both systole and diastole are shortened. Systole duration increases to the detriment of the diastolic duration. As a result, the left ventricle will not be filled sufficiently, adversely impacting on the cardiac output and also resulting in a weaker pulsation.
Ageing
Cardiac output is regulated in proportion to metabolic activity. Guyton & Hall (2006: p. 237) note that cardiac output declines with age, however they add that this is probably reflective of declining activity with age. This is associated with decreased skeletal muscle mass and therefore reduced oxygen and blood flow requirement reflected in a decreased cardiac output.
7.7. CM pulse qualities defined by pulse force
7.7.1. Replete pulse (Shí mài)

7.7.1.1. Alternative names
Full, Excess or Strong pulse.
7.7.1.2. Requisite parameters
Five pulse parameters are involved in the formation of the Replete pulse:
• Depth: The Replete pulse can be felt equally strong at each level of depth
• Width: The arterial width is increased from that of normal, being termed ‘wide’
• Length: Pulsations can be felt at all three traditional pulse positions of Cun, Guan and Chi and beyond Chi and/or beyond Cun
• Arterial wall tension: There is a slight increase in arterial wall tension which leads to a easily palpable arterial wall that retains its shape when moderate pressure is applied by the fingers.
7.7.1.3. Clinical definition
The Replete pulse is named for its strong arterial pulsations that hit the palpating fingers with an equally increased force at all three levels of depth and at the three traditional pulse positions Cun, Guan and Chi and beyond. The pulse force expands the artery both laterally and longitudinally so the pulse presents as wide under the fingers and long, extending beyond Chi and/or beyond Cun. There is a slight increase in arterial tension.
7.7.1.4. Identifying whether the Replete pulse is present
Step 1: When the fingers are placed over the radial artery pulsation with only the pressure of the resting fingers exerting pressure, the pulse may be easily palpated and is felt strongly under all three fingertips.
Step 2: With increasing finger pressure exerted over the radial pulsation, the pulse and artery resist deformation. With increasing finger pressure towards the radial bone the pulsation can be occluded with heavy pressure, but the pulse may still be felt against the proximal side of the ring finger at the Chi position. The finger pressure is then released slowly until the pulsation can be felt once more. At this deep level, the pulse can be felt as forcefully as it was at the superficial level of depth and at all three pulse positions.
Step 3: Once the superficial and depth levels of depth have been examined, the middle level of depth is assessed. The pulse can be felt equally strongly at this level of depth and at all three pulse positions. In this way, while pulse force is an important parameter in identifying this pulse, it also primarily depends on detecting the presence of pulse force at the three levels of depth and at the three pulse positions.
Step 4: This pulse will also present with an increased arterial width and a clearly defined arterial wall usually beyond the three traditional positions.
7.7.1.5. Classical description from The Lakeside Master’s Study of the Pulse
The replete pulse is obtained both floating and sunken.
The pulse is large and also long,
Slightly bowstring.
It responds to the fingers driving, driving [description comes from the Mai Jing]
7.7.1.6. CM indications
The Replete pulse usually indicates a pathological condition, always indicating the presence of a pathogenic factor, usually Heat or Fire. The one primary pattern associated with the Replete pulse is pathogenic Heat or Fire.
Replete pathogenic Heat or Fire
The Replete pulse indicates the presence of a strong pathogenic factor, usually Heat or Fire, generally resulting in the stagnation of Qi.
In the presence of pathogenic Heat, the appearance of the Replete pulse indicates that the antipathogenic Qi (Upright or Zheng Qi) is strong. The excessive force is a reflection of the struggle between the pathogen and the body’s Zheng Qi as it attempts to overcome the pathogen. It would also be expected that the hyperactivity of Yang could also cause an increase in pulse rate, resulting in the appearance of the Rapid pulse.
The Replete pulse is formed as a result of the body’s fight against the pathogenic factor, with blood and Qi overfilling the artery. Pulse force defines the Replete pulse and is determined by a combination of the strength of Yang Qi and the Yang nature of pathogenic Heat. Therefore the pulse has an increase in overall intensity, reflecting the summative accumulation of Yang Qi.
7.7.1.7. Clinical relevance
The Replete pulse can be seen in the pattern of Heat accumulating in the Triple Heater (Lu 1996: p. 86), where the Heat pathogen systemically affects the body, throughout the upper, middle and lower sections or Heaters of the body. This is also described in the Bin Hu Mai Xue(Li, Flaws (trans) 1998: p. 83) ‘Heat brewing in the three burners produces strong fire. This is communicated to the intestines’.
Depending on what organs the Heat or Fire is affecting, the accompanying signs and symptoms will correspondingly vary. For example, the literature notes manic behaviour occurring when the Heart is affected by Heat, while in the middle Heater there may be vomiting as Heat causes the Stomach Qi to become ‘rebellious’. Heat affecting the lower Jiao causes the fluids to dry, and constipation may dominate the clinical signs and symptoms.
If the pulse can be felt of equal strength at all levels of depth and is felt neither overly forceful nor forceless in regard to the individual, the rate and rhythm are normal and there are no accompanying adverse signs and symptoms, then this can be considered a healthy pulse: a sign of abundant Qi and blood and good Yang. However, such a pulse is not specifically the Replete pulse as previously defined, as it does not have increased force as a requisite parameter.
7.7.1.8. Biomedical perspective
An extremely forceful pulse, such as the Replete pulse, may occur as a result of systemic bacterial infection. As described by Guyton and Hall (2006: p. 286) features include:
• Marked increased vasodilatation throughout body and especially in the infected tissue
• High metabolic rate caused by bacterial stimulation and high body temperature.
• High cardiac output (not in all patients).
It would be expected that there would be a resultant increase in pulse rate as well. As the severity of the bacterial infection progresses to septic shock, other processes start to occur. For example, red blood cells start to accumulate in the degenerating tissues, small blood clots begin to form throughout and, as a result of the clotting factors being consumed, haemorrhages occur in many tissues such as the intestinal tract (Guyton & Hall 2006: p. 286). This can be seen from a CM perspective as the heat injuring the fluids. If clinically significant, then the bleeding could eventually cause the pulse to form into the Vacuous pulse or Surging pulse.
7.7.1.9. ‘Replete’ and relative strength
Many authors describe the occurrence of the Replete pulse in individual pulse positions. However, by definition, as explained in the ‘Clinical definition’ section above, it is impossible for the Replete pulse to occur in a single position, as part of the requisite changes in parameters is the appearance of the pulse in all three traditional pulse positions and beyond Chi and/or Cun.
Therefore, it is presumed that the term ‘replete’ in this case simply refers to a relative difference in strength (Box 7.13). As such, the ‘replete’ or increase in force occurring in a discrete position may not necessarily reflect pathogenic Heat (as the Replete pulse does) but may reflect another pathogenic mechanism such as obstruction or stasis.
7.7.1.10. Prognostic use
While the presence of the Replete pulse in a replete (excess) type pattern is seen as a positive indication that the signs reflect the pattern (Box 7.14), Deng asserts that its presence in a vacuity pattern signifies a critical condition and indicates that the pathogenic factor is strong and the Zheng Qi is weak (1999: p. 127).
Box 7.14
The Replete pulse versus ‘replete’ as a descriptive term
It should be remembered that the term ‘replete’ is often used as a general descriptive term to describe any pulse with that presents with force (as used in the Nei Jing). This should be distinguished from its use as a specific CM pulse quality, the Replete pulse, which has distinct changes in a number of different pulse parameters (including pulse force) and which was first described in the later text devoted to pulse diagnosis, the Mai Jing.
7.7.2. Firm pulse (Láo mài)

7.7.2.1. Alternative names
The Firm pulse is also known in CM literature as the Confined, Fixed or Prison pulse.
Wiseman & Ellis (1996) note in their revised translation of a Chinese medical teaching text that the term ‘Firm pulse’ is no longer used. Instead, such a pulse is described as ‘stringlike and deep’, a composite of two other CM pulse qualities. This does not seem to be the case in other modern CM pulse literature, where the Firm pulse is still included as a CM pulse quality.
7.7.2.2. Requisite parameters
The Firm pulse is a complex pulse quality and therefore has changes in five pulse parameters:
• Force: The overall intensity of the pulsation is increased
• Depth: The Firm pulse cannot be felt at the superficial level of depth and usually not at the middle level of depth. It is felt strongest at the deep level of depth
• Width: The arterial diameter is increased in the Firm pulse
• Length: Pulsations can be felt at all three traditional positions and beyond Chi and/or beyond Cun
7.7.2.3. Clinical definition
The Firm pulse is a forceful pulse, felt strongest at the deep level of depth. It cannot be felt at the superficial level of depth. It has a wide diameter, and the arterial wall is distinct, so the artery is easily delineated from the surrounding tissue. It is perceived simultaneously by the three palpating fingers as a length of pulsating artery, extending beyond Chi and/or beyond Cun pulse positions. The Firm pulse probably develops from a ‘drawing in’ of the arterial structure so it sits deeper within the flesh.
7.7.2.4. Identifying whether the Firm pulse is present
Step 1: The pulse is best identified by firstly placing the fingers gently on the skin overlying the radial artery, with only the weight of the palpating fingers exerting downward pressure. At this superficial level of depth the radial pulsation cannot be felt.
Step 2: As finger pressure is exerted downwards the radial artery pulsation begins to be palpable, and with increasing finger pressure (pushing down towards the radial bone) the pulsation becomes more obvious. The arterial wall should be examined at this stage; it is distinctive and can be distinguished from the surrounding connective tissue. The arterial diameter can also be examined at this time; it should cause a broad area of the palpating finger to be indented, and is therefore classified as wide.
Step 3: Next, the deep level of the pulse is examined by increasing finger pressure so that the radial artery is occluded for a few seconds. The pulsation may still be felt at the proximal side of the ring finger, from the direction of the arterial blood flow, signifying a forcible pulsation. The finger pressure is then gently and slightly eased so that the pulsation can once again be felt. This is the deep level of depth and the pulsation will appear at its strongest at this level of depth. At this level of depth the pulsation hits the fingers forcefully. It can be felt under all three palpating fingers and beyond the Chi position.
Step 4: As finger pressure is released from the arterial pulsation, it decreases noticeably in force until it is imperceptible at the superficial level.
7.7.2.5. Classical description from The Lakeside Master’s Study of the Pulse
The confined pulse is similar to sunken, similar to deep-lying.
[But it is] replete, large, and also long,
Slightly bowstring.
7.7.2.6. CM indications
The Firm pulse is a pathological pulse quality, occurring only in the presence of illness and dysfunction. There are two main patterns associated with the Firm pulse, both considered to be internal Replete type patterns:
• Replete pathogenic Cold in the interior of the body
• Internal obstruction due to Qi or Blood stasis
Replete pathogenic Cold in the interior of the body
This Firm pulse can be seen when pathogenic Cold enters the body and directly lodges in the interior. This may affect the internal organs such as the stomach, the intestines or the uterus, which are considered to be particularly vulnerable to an attack of external Cold directly passing to the interior of the body (Maciocia 2004). Alternatively, this may be due to consumption of excessively cold food (such as ice cream) or cold drinks. Cold in the stomach may present with abdominal pain and vomiting of clear fluids, Cold in the intestines usually presents with lower abdominal pain and diarrhoea, and Cold in the uterus may result in pain during menstruation.
Pathogenic Cold can also enter the meridian system. An example of this is an invasion of pathogenic Cold into the Liver channel, which may present clinically as a hernia.
Lu (1996) also notes that the Firm pulse may be seen in convulsions caused by Wind.
Internal obstruction due to Qi or Blood stasis
The Firm pulse may also arise as a result of the internal stagnation of Qi or blood so that neither Qi nor blood is able to reach the exterior. Stasis may be caused by retention of food, or may be due to pathogenic factors such as Cold or phlegm. Improper diet or emotional disturbance may adversely impact on the Liver and Spleen, leading to Qi stasis that, over time, results in the stasis of Blood.
The Firm pulse is commonly associated with abdominal masses due to either Qi or Blood stasis (Lu 1996). Qi stasis can result in the formation of masses of indefinite shape that can form or dissipate at irregular intervals, influenced by the state of Qi flow. The location of the pain is not fixed. Such masses are known as ‘conglomerations’ and are usually associated with disease in the Fu (Yang) organs and problems with Qi. ‘Concretions’ are also caused by stasis and have a definite form and fixed location, usually associated with problems of the Zang (Yin) organs and blood (Wiseman & Ye 1998: p. 92). Blood stasis type pain is usually fixed, stabbing and more severe in nature.
Mechanism of pulse formation
A deeply located pulse can indicate:
• The location of disease in the interior or
• The obstruction of Yang Qi in the interior so that Qi and blood cannot move outwards.
In the case of Qi stasis, the increased arterial tension indicates disturbance to the normal Qi flow, and a resulting hyperactivity of Yang that is unable to move outwards.
In the case of pathogenic Cold, the increased arterial tension is due to the contracting nature of Cold. It also reflects the obstruction of normal flow of Qi and blood by the Cold, which has a tendency to constrain Yang.
The increased force and wide arterial diameter seen in the Firm pulse imply the presence of a pathogenic factor and reflect the resulting obstruction of Qi and/or blood.
7.7.2.7. Clinical relevance
Pain is one of the most obvious symptoms that a patient will present with in cases of obstruction of Qi or blood. Pain is often accompanied by an increase in arterial wall tension in the pulse, reflecting the obstructed flow. The nature of the pain may differ according to its cause. Blood stasis will present as fixed and boring pain and abdominal masses associated with it will be hard. Qi stasis, on the other hand, has a more diffuse area of involvement, the pain tends to have a distending feel and may also change in location.
The pain can be quite severe in the case of the EPA of Cold entering directly into the interior, and will have an acute onset.
Interestingly, while Li (Flaws (trans) 1998) describes the pathogenesis relating to the presence of many of the other pathological CM pulse qualities in individual pulse positions, there is no discussion of the appearance of the Firm pulse (or Confined pulse, as it is known in The Lakeside Master’s Study of the Pulse) in individual pulse positions. This may be because the Firm pulse usually arises due to pain due to the strong obstruction of Qi and/or blood, which will generally tend to have a systemic effect on the pulse, as occurs in all situations in which arterial tension is increased (Box 7.16).
Box 7.16
The Firm pulse as a prognostic indicator
Both Li (trans. Flaws 1998) and Lu (1996) assert that the appearance of the Firm pulse in a patient who has suffered a severe blood loss denotes a poor prognosis. This is a situation in which the pulse is contradictory to the individual’s actual state of health. That is, because blood is vacuous, the pulse should be easy to compress, and so the Firm pulse should not occur. Thus if the Firm pulse is occurring when blood is vacuous then this indicates that an EPA is residing in the vacuous space, falsely causing the pulse to present as strong. For an EPA to have done this indicates the Zheng Qi (Upright or antipathogenic Qi) is weak, implying that the pathogenic factor is strong.
7.7.3. Vacuous pulse (Xū mài)

7.7.3.1. Alternative names
Empty, Deplete, Feeble, Deficiency or Weak pulse.
7.7.3.2. Requisite parameters
The Vacuous pulse is a complex CM quality with changes in four pulse parameters:
• Force: The Vacuous pulse has a decreased pulse force. The perceived pulse force decreases with increasing finger pressure
• Depth: The Vacuous pulse is felt strongest at the superficial level of depth. (The pulsation actually disappears before we can palpate to the deep level of depth.)
• Width: The arterial width is increased from that of normal, resulting in a wide pulse
• Pulse occlusion: This pulse is easily occluded. There are also no perceived pulsations at the side of the finger when the pulse is occluded.
7.7.3.3. Clinical definition
The Vacuous pulse has a lack of intensity in the radial pulsation hitting the palpating fingers. The pulse is easily perceived with light pressure at the superficial level of depth and is also wide (due to vasodilatation). However, although the arterial wall can be felt, this is due to a relative hyperactivity of Yang caused by an underlying vacuity and so the artery is easily occluded when finger strength is increased into the deeper levels of depth. Accordingly, the arterial wall loses its definition, becoming indistinct, and the pulsation is absent with heavy pressure (at the deep level of depth).
7.7.3.4. Identifying whether the Vacuous pulse is present
Step 1: The fingers are placed gently over the radial artery pulsation, with only the pressure of the resting fingers on the skin. The pulsation should be easily felt at this level of depth, although the overall strength is forceless. The arterial diameter is wider than would normally be expected. Moving the fingers side to side (medially and laterally) across the arterial wall may assist in identifying this pulse.
Step 2: With increasing finger pressure downwards towards the middle level there should be a noticeable decrease in overall force, with little resistance by the arterial wall to deformation.
Step 3: With an increasing amount of finger pressure the pulse will be easily occluded, before reaching the deep level of depth. No pulsation can be felt either under the palpating fingers or on the proximal side of the ring finger (positioned over the Chi position). The definition of the arterial wall decreases so that it cannot be felt.
7.7.3.5. Comparison of definitions
A number of pulse texts include the term ‘slow’ in their descriptions of the Vacuous pulse (Belluomini & Cheung 1982, Flaws 1997, Li (Flaws trans) 1998, Wang (Yang trans) 1997). Although mentioning the term ‘slow’ in the general description of the Vacuous pulse, Flaws (1997: p. 25), qualifies this by saying he does not include it in his personal definition, noting pulses that are ‘floating, large and forceless’ are commonly seen in his clinical practice.
In Huynh’s 1981 translation of the Bin Hu Mai Xue, the Vacuous pulse (termed the Empty pulse) is described as having ‘slow beats’ but is not included in the section on the Slow pulse and its related types, nor is it accorded a number of beats per respiration. Deng (1999) includes the term ‘arrives slowly’ in his definition of the Vacuous pulse but also does not include the Vacuous pulse in the section on slow pulses, instead classifying it under pulses that are based on abnormal changes in strength.
A decreased rate (hence a Slow pulse) would suggest the presence of pathogenic Cold or a deficiency of Yang, accompanied by Cold signs and symptoms. However these patterns are not usually included in the indications for the Vacuous pulse. Rather than being an actual decrease in heart rate, the term ‘slow’ could possibly be interpreted as referring to the actual beat itself, the proportion of time that systole and diastole occur within each beat (see Chapter 2 for further information). That is, the actual pulse wave peak or time taken to full amplitude occurs over a relatively longer time, thus systole (which is perceived as the actual beat) is perceived as happening more slowly rather than a decrease in the pulse rate. As the intensity or strength of the pulse is also influenced by the both the force of the heart’s contraction and how quickly this occurs, the pulse wave intensity will also feel less forceful than it would if the contraction happened at a quicker rate. This, in conjunction with the wider than normal arterial diameter, further diluting pulse force. Overall, this means that the pulsation is perceived as forceless.
7.7.3.6. Classical description from the Mai Jing
The vacuous pulse is a slow, large, and limp pulse, impotent when felt with pressure applied and giving the (feeling) fingers an impression of wide hollowness
7.7.3.7. Specific definition versus descriptive terminology
It should be remembered that the term ‘vacuous’ is not only utilised as the name of a specific CM pulse quality but also as a generic term to describe any pulse that presents with a lack of force or is associated with a vacuity pattern. The terms ‘vacuous’ and ‘weak’ are often used interchangeably.
When the Vacuous pulse is used as a specific CM pulse quality, this refers to a pulse that is defined by changes in four pulse parameters, resulting in a pulse that is relatively strongest at the superficial level of depth, has a wide arterial diameter, hits the fingers without force and is easily occluded.
7.7.3.8. CM indications
The Vacuous pulse is, by nature and name, a vacuity-type pulse and therefore is the result of vacuity-type patterns, usually of both Qi and blood. Two patterns are associated with the formation of the Vacuous pulse:
• Vacuity patterns of Qi and blood
• EPA of summer heat.
Vacuity patterns of Qi and Blood
Blood and Qi have a mutual relationship; blood is considered to be the mother of Qi, and Qi engenders blood (Wiseman & Ye 1998). Blood vacuity is often accompanied by Qi vacuity signs, therefore the signs and symptoms accompanying the Vacuous pulse may include both blood and Qi vacuity signs: generally these include lethargy, shortness of breath, spontaneous sweating, pale complexion, low voice, dizziness, ‘floaters’ in eyes and pale tongue. Specific signs and symptoms will of course depend on the specific organs involved.
Mechanism of pulse formation
Qi, particularly the Yang aspect, works to maintain arterial wall tension; when Qi is vacuous the tension in the arterial wall is not maintained and the arterial diameter widens. Blood vacuity results in the decreased viscosity of the blood due to the decreased numbers of red blood cells. This results in decreased oxygen supply to the tissues and the resultant hypoxia causes the peripheral blood vessels to dilate in order to increase the blood flow through the tissues and back to the heart. This contributes to the increase in arterial diameter.
EPA of summer Heat
Clinically, the Vacuous pulse may be seen in heat exhaustion or heat stroke. This would be expected to have an acute onset and may occur during periods of extreme climatic heat. An EPA of summer Heat causes excessive heat in the body, consuming Qi and Yin fluids. This causes dehydration and causes the pulse to become forceless and easily occluded due to a decreased fluid volume in the arteries (decreased plasma volume). Li (Flaws trans 1998: pp. 81-82) describes the accompanying signs and symptoms as spontaneous sweating, very rapid pulse and fright palpitations (Box 7.17). He advises to ‘nourish the constructive, boost the Qi’, referring to the need to rehydrate, replenish fluids (an essential part of blood) and strengthen depleted Qi.
Box 7.17
Signs and symptoms of heat exhaustion
• Fever
• Sweating
• Thirst
• Dizziness
• Hypotension
• Weakness
• Nausea
• Vomiting
• Tachycardia
• Decrease in urination
When severe, dehydration may lead to the cessation of sweating and if the core temperature continues to rise then changes in neurological status such as delirium, confusion or loss of consciousness may occur if the temperature is not decreased.
The elderly and very young are the most susceptible to this type of pattern, as both groups are prone to difficulties with thermoregulation.
Mechanism of pulse formation
Heat exhaustion/heat stroke is characterised by fluid and electrolyte loss, especially sodium, causing dehydration. There is a consequent reduction in arterial volume (loss of plasma) and a corresponding decrease in blood pressure.
From a CM perspective, the loss of Yin fluids deprives Yang of its stabilising anchor. As a result, Yang ‘floats’, moving upwards and outwards; the pulse becomes superficial, forceless and wide. The loss of both fluid and Qi results in the lack of pulse force and its easy occlusion. The vacuous Yin means that Yang becomes relatively hyperactive and may also result in a Rapid pulse.
7.7.3.9. Differentiation of similar pulses
Both the Vacuous pulse and the Floating pulse are felt relatively strongest at the superficial level of depth. However, the Vacuous pulse is very easily occluded with minimal finger pressure whereas the Floating pulse may still be felt at other levels (although not as strong as the superficial level) with increased finger pressure.
Maciocia (2004: p. 474) prefers to use the term ‘Empty pulse’ to describe the Vacuous pulse and defines it as having:
No strength and disappears with a light pressure, feeling empty; it is soft but also relatively big and distended at the superficial level.
There are differences in opinion about the severity of the Vacuous pulse. Maciocia (2004) describes it as indicating an early or middle stage of Qi vacuity, progressing in a more severe form to the Weak pulse (defined as deep, soft and without strength). Interestingly, he does not consider changes in arterial width to be an essential feature in his definitions of the Weak or Soggy pulses.
Lu (1996) also compares the Vacuous pulse (which Lu labels Deplete) and Weak pulse. However, while he agrees that they are both indicative of vacuity-type syndromes of Qi and blood, Lu considers the Vacuous pulse to reflect a more severe deficiency condition. This manifests in what he terms the ‘more severe destruction of the mutual restriction of Yin and Yang or Qi and Blood’, signified by the superficial location and increase in diameter. (See Chapter 8 for further discussion of the evolution of CM pulse qualities.)
Li (Flaws trans 1998) also identifies damage to essence and blood via ‘bone-steaming’. This could be equated to Kidney Yin vacuity leading to consumption of Yin fluids and consequently Qi.
In spite of these difference there appears to be general consensus in the pulse literature about the pathogenesis leading to the development of the Vacuous pulse. A dual vacuity of Qi and Blood is hypothesised to be responsible for this pulse quality, and is usually associated with impaired organ functioning.
7.7.4. Faint pulse (Wēi mài)

7.7.4.1. Alternative names
Minute, Feeble, Minute, Indistinctive, Subtle, Diminutive or Evanescent pulse.
7.7.4.2. Requisite parameters
The Faint pulse is a complex CM pulse quality that has changes in four pulse parameters:
• Force: The Faint pulse has a greatly decreased intensity that further diminishes with increasing finger pressure; it is a difficult pulse to palpate because of the extreme lack of pulse force
• Width: The arterial width is greatly decreased, resulting in a very narrow arterial wall
• Pulse occlusion: This pulse is very easily occluded with slight finger pressure
• Arterial wall tension: The Faint pulse has a greatly decreased arterial wall tension.
The parameter of pulse depth is not specifically mentioned in traditional pulse literature concerning the Faint pulse. It is therefore assumed that depth does not play an important role in the formation of the Faint pulse and as such, it may be located at any level of depth depending on the pathogenesis. Of more importance is its extreme lack of force, extremely narrow width and its tendency to disappear with minimal finger pressure.
7.7.4.3. Clinical definition
The notable feature of the Faint pulse is the extreme presentation of changes in the pulse parameters, reflecting extreme vacuity. It is an extremely thin, forceless and easily occluded pulse. While easy occlusion and lack of force are descriptors of the Faint pulse, it is also defined in the literature as being a difficult pulse to locate due to its extreme lack of force. As such, the arterial pulsation may seem to ‘fade’ in and out of perception because of a small pulse amplitude.
Because of the lack of internal pressure force, the Faint pulse is easily obliterated by external finger pressure and so careful use of discrete pressure changes is required to locate the pulse. The arterial wall has little tensile force when finger pressure is applied so that it is perceived as having a lack of definition.
7.7.4.4. Identifying whether the Faint pulse is present
Step 1: Using the radial styloid process for guidance, the fingers are placed over the three traditional positions to locate the radial pulsation. The pulsation may be difficult to locate because of the greatly decreased force and lack of arterial tension.
Step 2: All levels of depth need to be examined in order to locate the pulsation. Once the pulsation is obtained, with slight finger pressure it should be easily occluded. The arterial width is very narrow, and it is also difficult to perceive because of the lack of vasomotor tone.
Step 3: If the arterial pulsation is very difficult to ascertain or seems to disappear then reappear, then this signifies the Faint pulse.
7.7.4.5. Classical description from the Mai Jing
The faint pulse is a very fine, soft pulse possibly bordering on expiry, sometimes there and sometimes not [said in another version to be small; in still another to be quick under the fingers, in yet another to be floating and thin; in still another to come to almost an end when pressure is applied].
7.7.4.6. CM indications
The Faint pulse is a pathological pulse quality representing an extreme vacuity of both Yang and Qi as well as blood. It always indicates a critical condition. Two main patterns are associated with the Faint pulse:
Severe Qi and Blood vacuity (chronic)
The severe vacuity of Qi and blood is usually due to chronic disease. This is known as ‘vacuity desertion’ (Wiseman & Ye 1998). The appearance of the Faint pulse denotes a critical worsening of a disease. Such severe vacuity usually indicates long-term hypofunctioning of the organs and may be caused by chronic lifestyle issues such as overexertion, insufficient sleep, poor diet and emotional disharmony.
Yang collapse or shock (acute)
From a CM perspective, this could refer to any acute situation where the separation of Yin and Yang occurs. This may be seen with high fever or massive blood and fluid loss such as haemorrhage, profuse sweating or severe vomiting and diarrhoea. The extreme and sudden loss of Yin means that Yang is no longer nourished and supported, leading to the collapse of Yang. (This is could be associated with hypovolemic shock.) This is reflected in signs and symptoms such as cold limbs, profuse beadlike sweating, no thirst, loose stools or incontinence of urine or stools, or unconsciousness.
7.7.4.7. Biomedical perspective
The Faint pulse is termed the ‘weak and thready pulse’ and can be seen in circulatory shock: that is, any condition where blood vessels are inadequately filled and blood is unable to circulate properly, such as heart failure. As a result of the decrease in circulating blood flow, initial compensatory mechanisms help to resolve the resulting decrease in blood pressure, such as vasoconstriction of peripheral blood vessels. This may occur in severe haemorrhage, profuse sweating or severe repeated vomiting. Acute trauma such as extensive burns can also contribute to loss of water and plasma, resulting in a reduced blood circulation (hypovolemic shock) and greatly increased blood viscosity (see section 7.4.2 for the stages of hypovolemic shock).
As noted earlier, shock generally progresses in three stages, with the third stage being irreversible and leading to death. The Faint pulse, as a critical pulse, may be equated with either the progressive or irreversible stage of circulatory shock. By this stage, positive feedback mechanisms have been initiated and perpetuate continuing damage to the heart and other tissues, further impairing cardiac output and leading to irreparable tissue and organ damage. As such, the Faint pulse is associated with severe exhaustion in critical conditions, and may be seen in dying patients.
The Faint pulse has a poor prognosis when it appears in chronic conditions, indicating further critical decline in homeostasis.
7.7.5. Weak pulse (Ruò mài)

7.7.5.1. Alternative names
Frail, Infirm pulse.
7.7.5.2. Requisite parameters
The Weak pulse is a complex pulse quality characterised by changes in four pulse parameters:
• Force: The Weak pulse has a decreased overall intensity of pulsation
• Depth: It is found strongest at the deep level of depth and it cannot be felt at the superficial level
• Width: The arterial width is decreased from that of normal
• Ease of occlusion: With increasing finger pressure down to the deep level of depth, the pulse is easily occluded.
7.7.5.3. Clinical definition
The Weak pulse can only be palpated with medium to heavy pressure, being relatively strongest at the deep level of depth. Overall the pulsation is forceless, hitting the fingers with little intensity. It is easily occluded with increasing finger pressure and is unlikely to be still felt at the proximal side of the ring finger with pulse occlusion. It has a narrow but distinct pulse width (commonly described as ‘threadlike’).
7.7.5.4. Identifying whether the Weak pulse is present
Step 1: The fingers are placed gently over the radial artery pulsation, with only the pressure of the resting fingers on the skin. The pulsation should not be able to felt at this superficial level of depth.
Step 2: With increasing finger pressure downwards towards the middle level the pulsation may be able to be felt but with little intensity hitting the fingers.
Step 3: With an increasing amount of finger pressure, heading towards the deep level of depth, the pulsation should become apparent, although with a lack of overall intensity. The pulse has a narrow arterial width, displacing only a small area on the palpating finger. With heavier pressure, as the external pressure exerted on the arterial wall equals the internal pressure, the pulsation ceases so that no pulsation can be felt either under the palpating fingers or on the proximal side of the ring finger (positioned over the Chi position). Simultaneously, the definition of the arterial wall decreases so that it cannot be felt.
7.7.5.5. Classical description from the Mai Jing
The weak pulse is a very soft, deep, and fine pulse bordering on expiry under the (feeling) fingers when pressure is applied [said in another version to be impalpable unless pressure is applied and absent when pressure is released]
7.7.5.6. CM indications
The Weak pulse occurs in vacuity patterns and is generally seen as a pathological pulse quality. The occurrence of the Weak pulse at the deep level of depth indicates the inability of Yang to circulate Qi to the exterior of the body. It also specifies that the problem is located in the interior of the body, involving organ involvement. The Weak pulse can occurs as the result of vacuity of both Qi and Blood, particularly Yang. The circumstances in which the pulse manifests include:
• Pathology
• Age-related changes.
The diagnostic meaning of the pulse is further differentiated on the basis of:
• Constitutional health and age of the patient
• Presence or absence of other illnesses.
Vacuity of both Qi and Blood, particularly Yang Qi
While the Weak pulse reflects a dual vacuity of Qi and blood, Yang Qi vacuity is the predominating feature. Yang Qi vacuity signifies hypoactivity of physiological functioning, exhibiting signs and symptoms that reflect the damage to the warming and moving aspects of Yang Qi. Cold signs and symptoms accompany the Weak pulse, such as aversion to cold, cold extremities, pale complexion, lethargy, loose stools, a desire for warm drinks, increased urinary output and spontaneous sweating.
Constitutional health
If the Weak pulse occurs in someone who is young, Lu (1996) considers this to be a sign of a weak constitution, inherited from parents. This constitutional weakness may predispose the individual to increased attack by EPAs. In this case, the pulse may not present as the Floating pulse in response to the presence of an EPA because of the body’s already depleted Qi. Pre-Heavenly Essence or Jing represents the inherited energy from each parent at the time of conception and cannot be replenished.
Long-term illness
Chronic illness causes the consumption of both Yin and Yang over time. The appearance of the Weak pulse is seen as a natural reflection of this underlying vacuity. This may be the result of organ hypofunction and can be seen in vacuity patterns of the Kidney (sore knees, tinnitus, aching bones) and Spleen (digestive problems, tiredness, muscle weakness).
Age-related changes
Qi and blood are traditionally considered to diminish with the natural progression of age, and the Weak pulse is said to appear in older people as a reflection of this decline. However, a vacuity of Qi and blood is considered to be pathological, whether age related or not, and it would be expected that there would be accompanying abnormal signs and symptoms associated with Qi and blood, depending on which predominates.
7.7.5.7. Biomedical perspective
From a biomedical perspective, the Weak pulse may indicate problems with the heart affecting the cardiac output and resulting in decreased pulse amplitude. Clinically, the Weak pulse can be seen in prolonged chronic illness.
7.7.5.8. Comparison of similar CM pulse qualities
The Weak pulse and Soggy pulse both have decreased pulse force and pulse width. They are differentiated by the level of depth at which the arterial pulsation can be felt relatively strongest. The Weak pulse is felt relatively strongest at the deep level of depth, while the Soggy pulse is felt relatively strongest at the superficial level of depth. As such, these are in fact similar pulse types, albeit found at different levels of depth. Accordingly, the underlying pathogenesis of each pulse quality reflects both the similarities and differences between them.
Both the Weak and Soggy pulses are considered to be indicative of Qi and blood vacuity, reflected in the overall lack of intensity in pulsation and the decrease in arterial width. However, it is the level of depth that further differentiates the causal background, with the Weak pulse reflecting the predominance of Yang Qi vacuity. The Soggy pulse, on the other hand, is mainly indicative of either Yin vacuity or an EPA of Damp. Therefore, the Soggy pulse is felt relatively strongest at the superficial level of depth, which reflects involvement at the exterior of the body. The vacuity of Yin means that the Soggy pulse cannot be felt at the deep (or organ/Yin) level of depth.
7.7.6. Soggy pulse (Rú mài)

7.7.6.1. Alternative names
Soft, Weak, Floating or Frail pulse.
7.7.6.2. Requisite parameters
The Soggy pulse has changes in four pulse parameters:
• Force: The Soggy pulse has a decreased pulsatile force
• Depth: This pulse is relatively strongest at the superficial level of depth, decreasing in force with increasing finger pressure
• Width: The arterial width is decreased, resulting in a narrow pulse
• Ease of occlusion: The Soggy pulse is easily occluded with increasing finger pressure.
7.7.6.3. Clinical definition
The Soggy pulse lacks force in the arterial pulse pressure wave, hitting the finger with little intensity. It has a thin but distinct arterial diameter (often described as thread-like), felt strongest at the superficial level of depth and easily occluded when further pressure is applied (before the deep level of depth can be reached).
7.7.6.4. Identifying whether the Soggy pulse is present
Step 1: The fingers are placed gently over the radial artery pulsation, with only the pressure of the resting fingers on the skin. The pulsation should be easily felt at this level of depth, although the overall strength is forceless. The arterial wall is defined so that the arterial width can be described as thin, displacing a narrow area of skin on the palpating fingertips.
Step 2: With increasing finger pressure downwards towards the middle level there should be a noticeable decrease in overall force, with little resistance by the arterial wall to deformation. As finger pressure is increased the arterial pulsation is easily occluded so that no pulsation can be felt either under the palpating fingers or on the proximal side of the ring finger (positioned over the Chi position).
The pulse cannot be felt at the deep level of depth, as it is occluded well before reaching this level of depth.
7.7.6.5. Classical description from the Mai Jing
The soft pulse is a very soft pulse as well as floating and thin [said in another version to be absent when pressure is applied but potent when pressure is released; in still another to be small and soft; soggy instead of weak in yet another, where the soggy pulse is said to be like the clothes in water which are reachable only to a gentle hand.]
7.7.6.6. CM indications
The Soggy pulse is a pathological CM pulse quality and is associated with vacuity-type patterns. The Soggy pulse usually indicates vacuity of Qi and blood or Yin; however, an EPA of Damp may complicate this pattern. Two main patterns associated are with the Soggy pulse:
• Vacuity of Qi and blood or Yin
• Vacuity of Qi and blood complicated by an EPA of Damp
Vacuity of Qi and Blood or Yin
The Soggy pulse may arise due to vacuity of Qi and the concurrent vacuity of either blood or Yin. Blood vacuity may arise due to loss of blood through abnormal bleeding from the nose, stomach or throat known as ‘flooding invertedly’ (Li, Flaws (trans) 1998: p. 107). Alternatively, Yin vacuity signs such night sweating and ‘steaming of the bones’ (tidal fever, restless sleep and agitation) may occur, a sign that the body’s nourishing and cooling abilities have been compromised.
• Mechanism of pulse formation: The inadequate expansion of blood vessels due to deficient Yin (fluid) or blood inadequately filling the vessel, the pulse is consequently forceless, decreased in width and easily occluded. As Yin is depleted, Yang is no longer anchored and so moves upward, resulting in a superficially located artery.
Vacuity of Qi and Blood complicated by an EPA of Damp
Exogenous damp can enter the body through the pores of the skin, settling in the flesh. As Clavey (1995: p. 124) notes:
Even just locally, however, in the surface tissues, the pathogenic damp can interrupt normal fluid movement and cause edema.
The Damp EPA enters the body whose physiological processes are already impaired by Qi and blood vacuity. Qi vacuity compromises the body’s ability to defend itself from external attack and may also enhance the effect of the pathogen. If the Spleen is affected this may impact on the body’s ability to further transform and move fluids throughout the body.
The Dampness trapped in the tissue both impairs and consumes Yang Qi, leading to a forceless pulse. It compresses the pulse, resulting in an arterial diameter that is narrow, already depleted by Qi and blood vacuity.
Other authors mention that the Soggy pulse is indicative of chronic Dampness such as ‘postviral fatigue syndrome’ (Maciocia 2004: p. 481).
7.7.6.7. Body types and the Soggy pulse
It is noted in some pulse texts that the Soggy pulse is the pulse most likely to be felt in thin individuals. This appears to come from the Mai Jing (Wang, Yang (trans) 1997: p. 10) which claimed that ‘The pulses in females are inclined to be more soggy and weaker than in males’ and ‘if the person is small, a female, or thin, the pulse is (accordingly) small and limp.’ However this is contradicted in a modern CM text that notes ‘Obese people tend to have fine and deep pulses, while thin people have large pulses’ (Wiseman & Ellis 1996: p. 118).
Because of the contradictory nature of the information pertaining to body and pulse width and in the absence of demographic information, instead of generalising about this relationship, it is necessary to evaluate the pulse width within the context of the other presenting signs and symptoms, as well as the changes in other pulse parameters.
7.7.6.8. Comparison of similar CM pulse qualities
The Weak pulse and Soggy pulse are similar in their presentation, differentiated by the level of depth they are located (Table 7.2). The Weak pulse is strongest at the deep level of depth, while the Soggy pulse is strongest at the superficial level of depth. This is symbolic of their pathogenesis, with the Weak pulse generally indicating Yang vacuity and therefore being vacuous at the Yang level, and the Soggy pulse indicating Yin vacuity and therefore not found at the deep level of depth (which represents Yin).
| -not a requisite pulse parameter for this CM pulse quality. | ||||||
| Replete pulse | Firm pulse | Vacuous pulse | Weak pulse | Soggy pulse | Faint pulse | |
|---|---|---|---|---|---|---|
| Pulse force | ↑↑ force | ↑↑ force | ↓ force | ↓ force | ↓ force | ↓↓ force Difficult to feel |
| Pulse occlusion | Retains form with increasing finger pressure due to increased internal resistance within artery. | Retains form with increasing finger pressure due to increased internal resistance within artery. | Easily occluded before reaching the deep level of depth. | Easily occluded due to the lack of internal resistance (decreased volume and force) | Easily occluded due to the lack of internal resistance (decreased volume and force) | Very easily occluded due to the lack of internal resistance (decreased volume and force) |
| With significant pressure, pulse is occluded. May still pulsate at side of finger while occluding pulse. | With significant pressure, pulse is occluded. May still pulsate at side of finger while occluding pulse. | |||||
| Pulse depth | Felt at all levels of depth | Deep level of depth. | Superficial level of depth | Deep level of depth. | Superficial level of depth | May be seen at any level, depending on underlying pattern |
| Cannot be felt at the superficial level | Cannot be felt at the superficial level | Cannot be felt at deep level of depth | ||||
| Arterial width | ↑ width | ↑ width | ↑ width | ↓ width | ↓ width | ↓↓ width |
| Pulse length | Long | Long | – | − | – | – |
| Arterial wall tension | Slight ↑ tension | ↑ tension | ↓ tension, the arterial wall is easily deformed with finger pressure | − | – | Significantly ↓↓ tension. Difficult to feel arterial pulsation. |
7.7.6.9. Clinical relevance
The Soggy pulse is often seen in Yin vacuity patterns, the exact signs and symptoms of which may depend on the organ(s) affected (Fig. 7.5). The Soggy pulse is commonly noted as the CM pulse quality seen in Damp patterns, particularly associated with underlying Spleen Qi vacuity and digestive dysfunction (Kaptchuk 2000, Maciocia 2004, Wiseman & Ellis 1996).
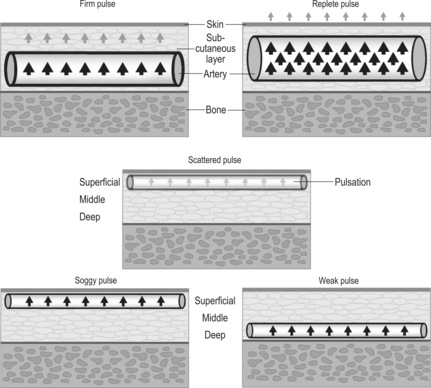 |
| Figure 7.5Schematic representations of the Replete, Firm, Soggy, Weak and Scattered pulses. |
Lu (1996) asserts that the Soggy pulse can be seen in postpartum women, signifying both Qi and blood vacuity.
7.8. Pulse contour and flow wave
The final parameter of pulse contour and flow wave primarily encompass the actual longitudinal movement of blood flow through the radial artery and its interaction with the arterial wall. Together these contribute to the formation of the contour or shape of the pulse.
7.8.1. Classifying CM pulse qualities according to pulse contour
There are four specific CM pulse qualities that are defined by the shape of the pulse contour and flow wave. The contour pulses include one of the most commonly diagnosed pulses in clinical practice, the Slippery pulse, and one that is rarely seen, the Stirred (or Spinning Bean) pulse. They are:
• Slippery pulse (section 7.9.1)
• Rough pulse (section 7.9.2)
• Surging pulse (section 7.9.3)
• Stirred (Spinning Bean) pulse (section 7.9.4).
7.8.2. Definition of pulse contour and flow wave
The contour of the pulse refers to the shape of the pulsation that can be felt by the palpating fingers. It is formed by the pressure wave as it moves through the artery, deforming the arterial wall and propagating the longitudinal forward movement of blood (the flow wave). The pulse contour and the flow wave are influenced by a number of interacting factors including:
• Flexibility of the arterial walls and their relative tension
• Volume of blood/fluids within the circulatory system
• Blood viscosity (flow varies inversely with the viscosity of the blood; McCance & Huether 2006)
• Condition of the lumen of the arterial wall, which influences the nature of the movement of the flow wave through the artery.
7.8.3. Assessment of pulse contour and flow wave
The assessment of pulse contour and flow wave involves two aspects:
• Evaluation of the consistency of the blood flow
• Evaluation of the pressure and flow wave and their impact on the arterial wall.
7.8.3.1. Evaluation of the tactile sensation of the flow wave contour
This involves assessing the nature or texture of the movement of blood as it passes through the radial artery underneath the fingers. There are number of questions that must be addressed when assessing this parameter:
• Does the blood flow feel smooth or turbulent? Is the blood flow consistent?
• Are there changes in the intensity of pulse force? This may make the pulsation appear stronger or weaker at times.
• Is the contour formed by each pulsation distinctly uniform or does it seem to change in shape?
7.8.3.2. Evaluation of the interaction of the pressure wave and flow wave on the arterial wall
We need to assess how the pulse wave feels:
• On arrival at the fingers
• As it passes underneath the fingers
• As it moves away from the fingers
This relates to the upward rise of the pressure pulsation, the peak and then the receding pressure (preceding the arrival of the next pulsation) and its interaction with the arterial wall. Different segments of the pulse wave may be more distinctive than others. For example, the arrival of the pulsation may be more distinctive than its departure. Alternatively, both the arrival and departure of the pulsation may be clearly felt.
7.8.4. Regulation of pulse contour and flow wave: CM perspective
The smooth flow of Qi and blood depends on four important factors. Lu (1996) notes that if any of these factors are compromised, pathological changes in the pulse contour may occur. These factors are:
• The presence of sufficient Qi and Yang
• The quantity and quality of Yin fluids
• The internal condition of the arterial wall (the tunica intima): a smooth arterial lumen ensures unimpeded laminar blood flow
• The external environment surrounding the arteries (connective tissue, organs, peritoneum, etc.): compression of arteries may adversely affect the distensibility of the artery.
7.8.4.1. Presence of sufficient Qi and Yang
Qi is the commander of the blood (Fig. 7.6). In this capacity, it produces, moves and keeps the blood within the blood vessels (specifically a function of Spleen Qi). Therefore Qi vacuity may affect the normal flow of blood, ultimately leading to sluggish flow or even stagnation of blood. In particular, Yang Qi is important to provide the Heart with the sufficient control over the blood and the vessels so that blood has the momentum to be propelled through the arterial system. Therefore Heart Yang has an important role in the circulation of Qi and blood not only in the chest but also throughout the body. If sufficient blood cannot reach the vital organs, then this can lead to functional problems with the transformation and transportation of Qi, blood and body fluids. This in turn may perpetuate or exacerbate the vacuity of Qi and blood. If Spleen Qi is vacuous, this may affect the production and consequently quantity of both Qi and blood.
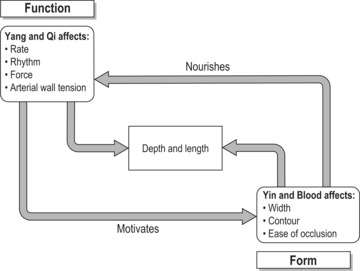 |
| Figure 7.6The mutual relationship between Qi and Blood. |
7.8.4.2. Quantity and quality of Yin fluids
Blood is the mother of Qi, nourishing Qi and enabling its functional activity throughout the body (Wiseman & Ye 1998). Because of this close relationship between Qi and blood, the volume of blood or Yin fluids in any of its forms may impact on the tangible manifestation of Qi on blood flow, affecting pulse contour, pulse force, pulse width and the depth at which the pulse is most readily located. Therefore the quantity and quality of Yin fluids, encompassing blood, body fluids and Essence, also influences how blood moves through the arterial system (Fig. 7.7).
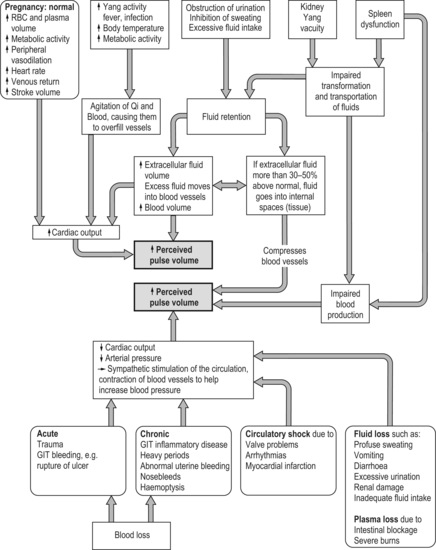 |
| Figure 7.7Factors affecting pulse volume. |
The pulse is affected by increases and decreases in blood/fluid volume in the following ways:
Increased volume
An increase in the volume of body fluids can affect the flow wave and pulse contour, depending on where the increase in volume occurs in the arterial system or in the connective tissue.
Increased fluid volume can develop as a result of abnormal fluid transformation and transportation involving the Spleen, Lung and Kidney and the Triple Heater. Fluid retention can occur due to normal water loss being inhibited, for example the inhibition of sweating or urination, and this can result in excess fluid moving into the blood vessels, leading to increased blood volume. Alternatively, fluid can accumulate in the limbs as oedema, in the lungs as phlegm or in the abdomen causing distension.
Clavey (1995: p. 134) notes that the close relationship between blood and fluids means that accumulated fluids can also interrupt normal blood flow, impacting on other bodily functions. For example the Shui Fen (water separation) syndrome illustrates what happens when oedema disperses menstrual blood ‘separating it pathologically into water and Qi so that blood cannot flow into the uterine vessels, thus causing amenorrhoea’.
Conversely, increased production of fluids may not necessarily be pathological but may happen routinely as the result of normal increased metabolic demands, such as those occurring during pregnancy.
Decreased volume
Decreased fluid volume may occur as the result of the damage or loss of blood, body fluids, Yin or Essence. This can influence the radial arterial pulsation in the following ways:
• Insufficient filling of the artery so that it feels ‘hollow’ and is therefore very easily occluded
• The artery fails to be expanded and therefore the arterial diameter is narrower than it should be
• Insufficient fluids may lead to turbulent flow through the arteries, causing changes in both the pulse contour (shape) and pulse force
• Decreased Yin may lead to the relative hyperactivity and outward movement of Yang, due to the loss of the anchoring effect of Yin.
7.8.4.3. Internal environment of arteries
The smooth flow of Qi and blood requires unimpeded access to arteries that have smooth walls to encourage the laminar flow of blood. Obstruction of the flow of Qi, blood or both through the arteries leads to irregular changes in the pulse contour, as blood moves turbulently through the arteries (for example, the Rough pulse). The aetiology behind the obstruction to Qi and blood flow may be varied, encompassing both replete and vacuity patterns. For example, the presence of pathogenic factors may adversely affect Yang Qi and its ability to move blood. Damp has a congealing, sticky effect, resulting in the sluggish flow of Qi and blood. Heat or Fire, on the other hand, can dry up body fluids causing them to congeal over time, leading to the formation of Phlegm, and consequently the impaired flow of blood and Qi.
7.8.4.4. External environment surrounding the arterial system
The arterial system is extensive, with the arteries passing through connective tissue, muscles, organs, the gastrointestinal system and numerous other tissues to supply oxygen and nutrients throughout the body. The arteries may be partially compressed by the tissues through which they pass, so that blood flow through part of the arterial system is compromised. This may result in blood flow varying in intensity as it makes its way through the affected tissue.
Possible causes of arterial compression include:
• Oedema: Fluids accumulating in the connective tissue and flesh may also compress blood vessels, so that normal expansion and contraction of the artery walls in response to the pulse and flow wave from the heart is inhibited.
• Trauma: Physical trauma may also result in disruption to blood flow through tissues.
7.8.5. Regulation of pulse contour and flow wave: biomedical perspective
There are numerous factors that can affect the pulse contour and flow wave. These are integrally related to the factors that affect pulse force and pulse width such as blood volume. As with the CM perspective, it is the interaction of these following factors that form the pulse contour and flow wave:
• Cardiac output, in particular stroke volume (the amount of blood expelled from the left ventricle into the aorta during systole) and resulting pulse amplitude
• Blood viscosity; flow varies inversely with the viscosity of the blood (McCance & Huether 2006, Tortora & Grabowski 2000)
• Compliance of the arterial walls and their relative tension
• The condition of the lumen of the arterial wall, which influences the nature of the blood flow.
7.8.5.1. Smooth versus turbulent flow
The pulse contour and flow wave can be interpreted in terms of the smoothness of the blood flow and its relative state of turbulence. McCance & Huether (2002: p. 962) note that ‘Where flow is obstructed, or the vessel turns, or blood flows over rough surfaces, it becomes turbulent … Resistance increases with turbulence’.
The condition of the lining of the arteries influences the fluidity of the blood flow. A rough lumen encourages turbulent flow. Atherosclerotic plaques inside the arteries may also impede flow, decreasing the arterial diameter and also causing disruption to the smooth surface lining the inner surfaces of the arterial wall.
7.8.5.2. Blood viscosity
Viscosity may also impact on blood flow. The viscosity of blood depends on the ratio of plasma volume and the number of circulating red blood cells. The more viscous the blood, the more sluggish the blood flow. Conversely, the lower the blood viscosity the faster and more turbulent the blood flow (Fig. 7.8).
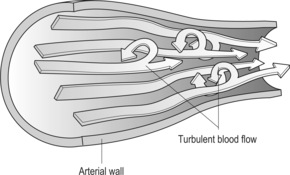 |
| Figure 7.8Turbulent blood flow.(Adapted from Part B of Figure 29.33 of McCance & Huether 2006, with permission of Elsevier Mosby.) |
Factors affecting blood viscosity include anaemia (decreased viscosity due to decreased size or numbers of red blood cells), dehydration (increased viscosity due to loss of body fluids through severe sweating, diarrhoea or vomiting) and plasma loss (increased viscosity due to loss of blood volume but not red blood cells).
7.8.5.3. Pregnancy
A number of changes in the cardiovascular system occur very early during pregnancy, one being a decrease in peripheral vascular resistance. It is hypothesised that this provides the stimulus for the activation of the renin-angitensin-aldosterone axis, responsible for the increase in plasma volume and cardiac output (Chapman et al 1998, cited in Poston & Williams 2002). These changes are apparent at about 5 weeks after conception. During normal pregnancy the increase in blood volume (on average about 1.5 litres) is due to both an increase in red blood cells (by 15-18%) and plasma volume (about 40-50%). This results in physiological anaemia and represents hypervolaemia or haemodilution, which is deemed a necessary adaptation of pregnancy in order to accommodate for cardiovascular changes and expected loss of blood at delivery (Coad & Dunstall 2005). The increased plasma/blood volume also provides increased systemic oxygen supply, increased renal filtration and helps to disperse increased heat production due to increased metabolic activity (Estes 2006).
7.9. CM pulses defined by pulse contour
7.9.1. Slippery pulse (Huá mài)

The Slippery pulse is defined by changes occurring in a single pulse parameter. However, despite its seeming simplicity, the parameter of pulse contour encompasses a number of diverse variables associated with blood flow and the arterial wall structure. It should be noted that although the indications of the Slippery pulse all point towards repletion patterns and therefore by association, increased pulse force, this is not a requisite pulse parameter.
7.9.1.1. Alternative names
Although the name ‘Slippery pulse’ is most commonly used, it is also known in CM literature as the Smooth or Rolling pulse, which also aptly describe the shape of the pulse contour and how the flow wave moves under the palpating fingers.
7.9.1.2. Requisite parameters
• Pulse contour and flow wave: The Slippery pulse has a rounded shape or contour to the palpating finger. As the pressure wave travels along the radial artery, the arterial wall expands and contracts with ease as blood is pushed through the artery (the flow wave).
7.9.1.3. Clinical definition
The Slippery pulse is characterized by the smooth fluidity of blood flow under the palpating finger. The pulsation can be clearly felt expanding the arterial wall: the flow wave hitting and passing under the palpating finger, resulting in a distinct dilatation and contraction of the arterial wall so that a relatively large surface area of the artery is affected. The arterial wall returns to a normal resting state once the pressure wave departs, until the next wave arrives. This sensation is often described as giving the impression of ‘smoothness’ or a ‘rolling’ type of action and is characterised by a lack of friction between the flow wave and the palpating fingers. The pulse relates primarily to the longitudinal flow of blood and its interaction with the arterial wall (Fig. 7.9).
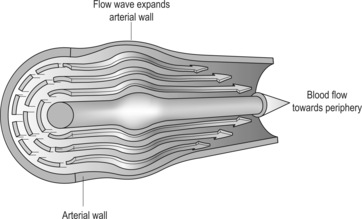 |
| Figure 7.9Schematic representation of the flow wave and contour contributing to the formation of the Slippery pulse.(Adapted from Part A of Figure 29.33 of McCance & Huether 2006, with permission of Elsevier Mosby.) |
7.9.1.4. Classical description from The Lakeside Master’s Study of the Pulse
A slippery pulse goes and comes, advances and retreats
Flowingly, uninhibitedly, unfurled, revolving
It responds to the fingers like a pearl (or bead) Mai Jing]
7.9.1.5. CM indications
The Slippery pulse can represent health, or may be considered to be a pathological pulse quality, depending on the accompanying signs and symptoms. There are five main conditions that can result in the Slippery pulse:
• Health
• Pregnancy
• Presence of pathogenic factors such as Phlegm, Damp or Heat
• Food retention
• Menstrual cycle: Occurs at certain times during the cycle
Health
The Slippery pulse can be an indication of good health, signifying abundant Qi and blood filling out the blood vessels. This signifies that Yin and Yang are well balanced and harmonious. The Mai Jing notes (Wang, Yang (trans) 1997: p. 21):
(A pulse) emerging swiftly followed by falling is called slippery. What does this imply?
The master answers: Falling is pure Yin, while emerging is righteous Yang. When Yin and Yang are in harmony and cooperate, the pulse is slippery.
Pregnancy
The Slippery pulse is traditionally associated with a healthy pregnancy. It reflects the normal production of the extra blood and Qi that is required to supply the developing fetus with sufficient nutrients to grow and develop. This pulse is said to occur in the first trimester and is considered to be a healthy sign of a normally progressing pregnancy.
The Slippery pulse is also considered to be a diagnostic indicator of pregnancy. If the pulse is identified as Slippery and there is amenorrhoea (no periods) in someone whose periods are usually regular (Li, Flaws (trans) 1998: p. 76), then this may be a sign of pregnancy. In addition to the overall Slippery quality, an increased force in both Chi positions and the left Cun position is also deemed necessary by Maciocia (1998: p. 76). However, this theory in general should be used with some degree of caution, as the Slippery pulse can also occur in someone who is not pregnant, as the result of a pathological process such as pathogenic Damp, Phlegm or Heat.
Pathogenic factors such as Phlegm, Damp or Heat
The Slippery pulse is commonly associated with pathogenic Phlegm, Damp or Heat. These pathogens may occur individually or in varying combinations.
• Phlegm: This has a varied aetiology due to either external pathogens or endogenous causes, often involving vacuity (see Box 7.18). Many of these factors ultimately result in stasis or obstruction that congeals fluids. Phlegm may also arise due to the prolonged retention of Damp in the body, as a further progression of Damp. The presence of Heat may lead to the congealing of fluids or Damp, producing Phlegm.
Box 7.18
Underlying causes of Phlegm production
• EPA of Wind
• Dysfunction of Spleen, Lung or Kidney’s transformation and transportation functions
• San Jiao dysfunction of Qi transformation and fluid movement
• Stress or emotional imbalance leading to Liver Qi stagnation
• Constitutional Yin vacuity
• Dietary: consumption of cold/ raw foods or overeating
• Lung Yin deficiency
• Kidney Yang deficiency: due to ageing or excessive sexual activity.
(Clavey 1995: Ch. 7)
Because Phlegm has multiple causes and pathogenic mechanisms, this may be reflected in the varying changes in pulse parameters. In other words, Phlegm may manifest in differing pulse qualities, not necessarily only the Slippery pulse. As noted previously in section 7.3, phlegm may also result in the Stringlike (Wiry) pulse, which would tend to reflect the underlying stagnation of Liver Qi as the causal factor. There may also be changes in rate or the level of depth at which the pulse can be found depending on the nature of the Phlegm.
• Endogenous (internal) Damp: Internal Damp may be the result of Spleen or Kidney dysfunction, leading to impaired transformation and transportation of fluids. Alternatively Damp may arise due to dietary indiscretions such as the overconsumption of Damp-forming foods such as dairy (cheese, ice cream, milk) cold, raw food, citrus fruits and oily, fried or greasy foods. This can impact on the function of the Spleen and stomach, impairing transformation of food and drink and the distribution of fluids. Damp is greasy or sticky in nature and associated with the presence of excess fluids in the circulatory system or fluids trapped in the tissue. (See Box 7.19 for common Damp signs and symptoms.)
Box 7.19
Signs and symptoms commonly associated with Damp
• Feeling of heaviness
• Lethargy
• Loose stools
• Nausea
• Abdominal distension
• Chest distension
• No appetite or thirst
• White greasy tongue coat.
• Exogenous(external) Damp: Alternatively, the Slippery pulse may be caused by external pathogenic Damp due to climatic, environmental or living conditions ‘If one is affected by the dampness Qi of the earth, then this harms the skin, the flesh, the sinews, and the vessels’ (Unschuld 2003: p. 197). This would be seen as a replete-type pulse. However, the Moderate pulse and Soggy pulse are also associated with an EPA of Damp. The Soggy pulse may arise instead of the Slippery pulse if the individual has an underlying deficiency that may predispose them to external attack. The pathological Moderate pulse, with its slow rate, may be associated with pathogenic Cold Damp.
• Heat: The Slippery pulse may arise due to pathogenic Heat causing hyperactivity of both Qi and Blood, leading to excessive filling of arteries. Heat may have the additional effect of causing fluids to congeal, leading to the formation of Damp or Phlegm.
Food retention
Retained food may be caused by the regular consumption of Damp-inducing foods and alcohol which impact adversely on the Spleen and Stomach. This leads to impaired digestive function, and the retained food may transform into phlegm. As noted by Clavey (1995: p. 184), this is termed ‘food phlegm’ and is linked to Phlegm-Damp.
The Slippery pulse may be seen at different times during the menstrual cycle. Maciocia (1998: p. 77) describes the normal pulse during menstruation as ‘somewhat Slippery, Big and slightly rapid’.
It may be expected that at other times during the menstrual cycle the building up of blood and Yin in expectation of potential fertilisation (around mid-cycle, approximately days 11-15) may be reflected in the Slippery pulse. At this time of the cycle Yin is described as being ‘at the peak of its cycle, the Chong vessel is full of Blood’ (Lyttleton 2004: p. 36). From a physiological perspective, oestrogen is at its peak. There appears to be some limited initial biomedical support for this, with research showing increased radial artery distensibility (related to the ability of the artery to expand and contract and peripheral vasodilatation) occurring around ovulation (days 13-15) (see Box 7.20 for more information).
Box 7.20
The menstrual cycle and possible hormonal effects on radial artery distensibility
In a study undertaken to look at radial artery distensibility during the menstrual cycle, it was found that fluctuations did indeed occur during different phases of the menstrual cycle. Giannattasio, Failla, Grappiolo et al (1999) found that radial artery distensibility was increased markedly in the ovulatory phase (days 13-15) compared with the luteal phase (days 21-29) and follicular phase (days 3-5), which were decreased. Blood hormonal measurements showed that during the ovulatory phase oestradiol (oestrogen) was at its highest level, along with luteinising hormone (LH) and follicle-stimulating hormone (FSH). During the luteal phase, progesterone and antidiuretic hormone (ADH) were at their peak.
It is suggested that the variation in radial artery distensibility appears to be at least partially dependent on the sex hormones. The authors suggest that previous studies showing the existence of oestrogen receptors in vascular smooth muscle cells and the vasodilatory effects of oestrogen administration in animals, and the effects of increased oestrogen during pregnancy leading to an increase in arterial distensibility in both animals and humans, all point towards increased oestrogen levels in the ovulatory stage causing arterial distensibility.
The arterial stiffness of the luteal phase is due to an increase in the contraction of vascular smooth muscle in the arterial wall. While this may be due to a decrease in oestrogen levels during the luteal phase, it is likely to include other factors such the effects of increased progesterone and ADH levels that may reinforce the effect of decreased oestrogen levels or potentially have additional effects on the distensibility of the vascular wall.
7.9.1.6. Biomedical perspective
Recent research has shown possible support for the manifestation of the Slippery pulse during pregnancy, revealing differences in radial arterial blood flow in pregnant women compared to non-pregnant women (Chen & Clarke 2001) (Fig. 7.10). However, while it is hypothesised that this may be reflected in changes leading to the possible formation of the Slippery pulse (Fig. 7.11), unfortunately a manual palpation component to identify possible CM pulse maladies was not included in the study to allow for correlation of objective pulse changes with manually assessed CM pulse qualities (see Box 7.21).
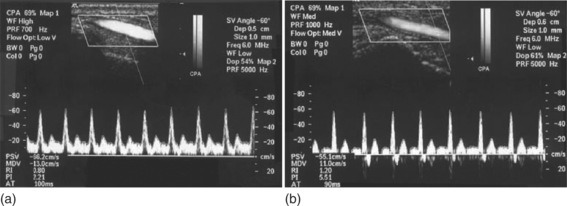 |
| Figure 7.10Typical Doppler wave forms in the radial artery of (a) pregnant and (b) non-pregnant women.(From Chen & Clark 2001, with permission of Blackwell Publishing.) |
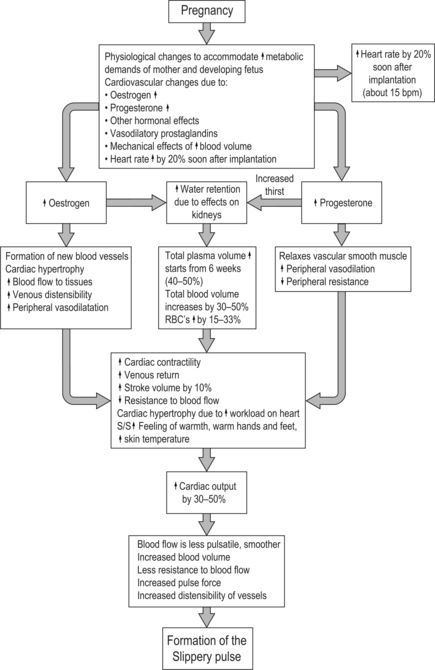 |
| Figure 7.11Likely effects of pregnancy on the cardiovascular system and the development of the Slippery pulse. |
Box 7.21
Pregnancy and changes in radial arterial blood flow
A research study has found that ‘the physical properties of the blood flow pattern in the radial artery are different between pregnant and non pregnant women’ (Chen & Clarke, 2001). It is hypothesized that oestrogen plays a role in the peripheral vasodilatation in two ways: inhibiting movement of calcium ions into vascular smooth muscle cells and stimulating nitric oxide, both of which cause relaxation of the smooth muscle.
This study also showed that blood flow pattern in pregnant women is believed to be less pulsatile than in non-pregnant women, ‘throughout the entire cardiac cycle, whereas reversal flow and an absence of flow were detected in the non-pregnant women’ (Chen & Clarke, 2001). They surmised that the decreased fluctuation of blood flow impact on the radial artery wall may contribute to the presentation of the CM ‘smooth’ pulse, described as feeling like ‘a group of small glass balls running underneath the fingertips’. This is a reference to the Slippery pulse.
This is mirrored in CM thought, which has traditionally believed that pregnancy may be recognised, even at early stages, by the changes in certain characteristics such as the pulse contour in the radial artery pulse that occur during pregnancy (Maciocia 1998).
7.9.1.7. Comparison of the Slippery pulse with other CM pulse qualities
The Slippery pulse should not be confused with a Rapid pulse, which is defined as having an increase in heart rate. While the Slippery pulse may appear to be rapid due to the ease with which it slips beneath the finger, when the actual rate is calculated, the rate should fall within the normal range of 60-90 bpm. If the Slippery pulse is caused by Heat, then the pulse rate may be rapid as well.
The Slippery pulse is also commonly mistaken for the Stringlike (Wiry) pulse, even though their respective descriptions are quite different (see Box 7.22). The Stringlike and Slippery pulses are probably some of the most commonly seen pulse qualities in clinical practice.
Box 7.22
Slippery pulse versus Stringlike pulse
• Slippery pulse: Blood flow forms the artery around itself: blood flow dominates arterial structure
• Stringlike (Wiry) pulse: The arterial wall is constricting blood flow: arterial structure dominates the contour of blood flow
Often in CM case studies, the pulse will be explained as being both Slippery and Stringlike (Wiry). As these are quite different pulse qualities in terms of the pulse parameters involved, how are these two pulse qualities seen in combination? If we examine what the main focus of each pulse is, we can see that they are actually concerned with different aspects of the pulse (see Box 7.23). The Stringlike (Wiry) pulse is mainly focused on the physical characteristics of the arterial wall (external aspect), while the Slippery pulse is primarily concerned with the flow wave and the forward longitudinal movement of blood (internal aspect). The Slippery pulse may sometimes be accompanied by increased arterial wall tension, but this would be seen as a relative increase, as the rounded contour of the pulse still dominates the pulse. As such, the tension would not be retained on increased finger pressure, indicating that the increased arterial wall tension is not the definitive Stringlike (Wiry) pulse. For example, this may be seen in conditions where Liver Qi encroaches on the Spleen and Stomach, leading to digestive disturbances. If we understand that increased arterial tension usually means obstruction, this may give us a clearer understanding of the underlying aetiology behind the pulse or alternatively, the extent of the pathogenesis.
Box 7.23
Pulse terminology
Unschuld (2003: p. 262) talks about the possibility of the terms such as ‘rough’ or ‘smooth’ being perhaps ‘remnants of a time when the condition of the skin above the vessels, rather than the movement in the vessels below the skin, was considered a valuable parameter’. In this context, the term ‘smooth’ would reflect that the skin has been moistened and nourished, a sign of that there is sufficient Blood and body fluids. Conversely, skin that feels overly moistened or ‘waterlogged’ (oedema) may reflect fluid pathology. Similarly ‘rough’ may refer to the skin’s lack of nourishment or moistening, reflecting a vacuity of blood or fluids. The interpretation of this terminology continues to resonate with the current indications of the both the Slippery and Rough pulses as defined today.
The Moderate pulse, although known for its change in pulse rate (it is defined as slow), is also commonly described as having a rounded pulse contour similar to the Slippery pulse. It can reflect health, as a sign of abundant Qi or blood, or as a pathological pulse quality it often occurs as a result of impaired Spleen Qi, particularly of Yang. Therefore the Moderate pulse may perhaps be considered to be a vacuity version of the Slippery pulse, with the Yang Qi vacuity affecting not only Spleen function but also slowing down metabolic activity generally, hence the decreased pulse rate. The accompanying signs and symptoms will also help to further differentiate the pattern. It must be remembered that pulse diagnosis is only one of the four examination procedures and that the other diagnostic indicators are also essential when formulating a diagnosis.
7.9.2. Rough pulse (Sè mài)

The Rough pulse is a complex pulse quality that is primarily concerned with the nature of the blood flow through the radial artery and the effect that this has on the pulse contour. It is often contrasted with the Slippery pulse, described as its opposite in terms of the fluidity of the blood flow through the radial artery.
7.9.2.1. Alternative names
The Rough pulse is also known throughout the CM literature such as the Choppy, Dry, Hesitant, Uneven, Grating or Difficult pulse. The differing interpretations of the various terms used to name the Rough pulse may be responsible for the diverse range of descriptions for this pulse quality between CM texts and even within individual pulse definitions (see Box 7.24).
Box 7.24
The Three Five pulse: a subcategory of the Rough pulse
The Three Five pulse is a subcategory of the Choppy pulse that is mentioned in a number of modern CM texts (Kaptchuk 2000, Maciocia 2004, Townsend & De Donna 1990). It refers to the frequently changing rate of the pulsation so that sometimes it beats three times per respiration and sometimes five times per respiration (it does involve misted beats). Townsend & De Donna (1990) note its link to Heart or circulatory disease, but the other authors do not elaborate on its meaning.
This should be distinguished from normal sinus arrhythmia that is noted for its increased pulse rate during inspiration and decreased pulse rate on expiration and may be seen in healthy young adults, particularly men (see section 6.6 for more information.)
7.9.2.2. Requisite parameters
The Rough pulse is a complex pulse quality with changes in two pulse parameters:
• Pulse contour: This has an irregular shape to the palpating finger, lacking a feeling of fluidity of flow
• Pulse force: This may vary in intensity and the timing of systole and diastole.
7.9.2.3. Clinical definition
The Rough pulse is marked by variations in pulse force and, accordingly, pulse contour. The pulse wave appears to change in intensity, resulting in a pulse that sometimes feels forceful and at other times seems to decrease in force. This impacts on the palpating fingers as a change in pulse amplitude so that, with an even amount of pressure exerted on the artery, the pulse sometimes is felt forcefully and at other times it presents as forceless.
The term ‘irregular’ is often used to describe the Rough pulse. However, the irregularity described is associated with the changing intensity of pulse force. This may be caused by a change in the duration of systole and diastole or an inconsistency in blood flow, resulting in intra-arterial turbulence and poor propagation of the pulse pressure wave. This is perceived as an ‘unevenness’ by the palpating fingers.
The Rough pulse does not have missed beats, has a regular rhythm and is within the normal rate parameters.
7.9.2.4. Classical description from The Lakeside Master’s Study of the Pulse
Fine and slow, going and coming difficult, short and scattered. Possibly one stop and again comes (Mai Jing).
Uneven, not regular (Su Wen).
Like a light knife scraping bamboo (Mai Jue: Pulse Knacks).
Like rain wetting sand.
Like a diseased silkworm eating a leaf
7.9.2.5. CM indications
A slippery pulse shows abundant blood but scanty Qi. A choppy pulse shows scanty blood but abundant Qi. A large pulse shows abundance of both blood and Qi.
(From the Mai Jing (Wang, Yang (trans) 1997:p. 24).
The Rough pulse is associated with two main patterns, vacuity and repletion, further differentiated by manual palpation using the parameter of pulse force:
• Vacuity of Yin fluids such as body fluids, blood or Essence
• Repletion causing stasis or obstruction of blood.
The Rough pulse may be seen in body fluid loss, blood vacuity or the consumption of Kidney Essence (Fig. 7.12). Vacuity of Yin fluids leads to impaired blood flow through the arteries, resulting in an unsmooth flow of blood.
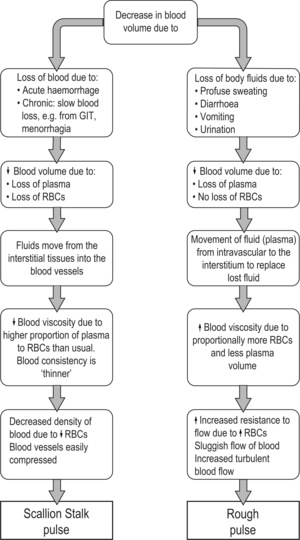 |
| Figure 7.12Fluid loss versus blood loss and the effects on the pulse. |
• Yin fluid loss: Fluid loss may occur due to profuse sweating or severe vomiting, leading to dehydration. Acute trauma such as severe burns or tissue damage may also result in loss of plasma volume. Intestinal obstruction may also result in large loss of plasma into the intestinal lumen (Guyton & Hall 2006: p. 285). If fluid loss is severe, plasma may move from the circulatory system to replace the severely depleted fluid. This results in increased blood viscosity, which can lead to the sluggish flow of blood and increased turbulence, hence the appearance of the Rough pulse (see Box 7.6 and Box 7.7).
• Vacuity of blood or Kidney Essence in pregnancy: From a CM perspective, the appearance of the Rough pulse in pregnancy is always pathological. At the beginning of pregnancy the Rough pulse indicates possible miscarriage and towards the end of pregnancy it may indicate an increased risk of eclampsia (Maciocia 1998).
During pregnancy various cardiovascular changes occur naturally, accounting for the increased force and ‘slipperiness’ of the pulse, including dramatic increases to blood volume, particularly plasma volume. The increase in plasma volume correlates positively with both birth weight and placental weight. An unusually low increase in plasma volume is associated with low birth weight, stillbirth and recurrent miscarriages (Coad & Dunstall 2005: p. 263). This correlates with the CM perspective of the appearance of the Rough pulse, in its vacuous form, which implies that the normal increase to blood volume has been impaired, resulting in insufficient blood to nourish and support the rapidly growing fetus. As Lyttleton (2004: p. 319) notes, if there is dual vacuity of blood and Qi then this may result in decreased fetal growth.
Lu (1996) states that Kidney impairment may lead to the Kidney Essence (also an important component in the production of blood) being consumed and this may also lead to infertility or in the case of pregnancy, miscarriage.
• Obstruction with underlying vacuity: Li (Flaws (trans) 1998: p. 80) also links the Rough pulse with an invasion of cold dampness into the ‘constructive’, an aspect of the blood, causing ‘blood impediment’. Wiseman & Ye (1998: p. 32) define this as a bi(blockage) pattern occurring in patients with underlying Qi and blood vacuity, resulting in numbness and painful limbs. While the pulse is described as ‘faint, rough’, other changes such as ‘fine and tight at the cubit’ are also mentioned. ‘Tight’ may refer to the increased tension that arises due to the obstruction (signified by pain) while ‘fine’ may reflect the underlying vacuity, although this is difficult to know without further clarification by the author.
Replete patterns associated with stasis of Qi and Blood
The Rough pulse is also related to the stasis of normal Qi and blood flow. Some authors consider this pulse quality to be a sign of unhealthy lifestyle, seen in physically unfit people with an erratic lifestyle and diet, leading to stagnant Liver Qi with Damp (Townsend & De Donna 1990). As a result, Qi stasis eventually leads to the sluggish flow of the blood. However, other types of blood stasis may occur as the result of obstruction due to pathogenic factors or retained food.
• Cold Damp: The Rough pulse may occur with pathogenic Cold Damp, as the Cold contracts the vessels while Damp also causes stasis leading to obstruction of blood. In the Mai Jing, a discussion of the various causes of the ‘internal binding (of evils)’ giving rise to masses in the lower abdomen notes that ‘If the pulse arrives choppy, it points to the disease of cold dampness’ (Wang, Yang (trans) 1997: p. 23). This pattern is also described by Lu (1996: p 71).
• Retained food: Food retention may result in a Rough pulse because of its physical compression of the blood vessels due to the accumulation of undigested food in the stomach. However, the undigested food may exacerbate the pathogenesis by the transformation of the retained food into Damp and eventually Phlegm, which further impacts on Qi and blood flow.
• Blood stasis affecting fertility and pregnancy: The Rough pulse may occur in patterns of blood stasis associated with the menstrual cycle, impacting on both the ability to become pregnant and also the viability of the pregnancy. Blood stagnation may impact on the endometrium and also the Chong Mai (also called the ‘Sea of Blood’), one of the Eight Extra meridians associated with the menstrual cycle and fertility.
Endometriosis is a condition where endometrial tissue is found outside the uterus in the pelvic cavity. This can range from tiny spots to masses that distort the pelvic organs and can be found on or inside the ovaries, tubes, bladder or bowel (Lyttleton 2004: p. 167). For some women this may be non-symptomatic, but for others it may be the source of pain, menstrual problems and infertility. During pregnancy, the damage to the endometrium from endometriosis may affect the blood supply to the placenta, affecting its development and therefore increasing the risk of miscarriage (Lyttleton 2004).
Endometriosis is commonly associated with Blood stasis in terms of signs and symptoms such as stabbing pain, clotted menstrual blood and abdominal masses. It should be noted that if the pain associated with the blood stagnation is strong, then the overriding pulse quality that may be felt is the Tight pulse (Lyttleton 2004: p. 95). Lyttleton notes that endometriosis is also associated with Phlegm Damp and Kidney Yang vacuity, with the production of mucus secretions that obstruct to normal functioning of the reproductive system. All of these patterns may result in the obstruction of normal flow of Qi and thus Blood, reflected in the appearance of the Rough pulse.
7.9.2.6. Biomedical perspective
From a biomedical perspective, irregularities in pulse force may indicate a lack of smooth muscle tone in the arteries or changes in the force of the cardiac contraction (Tortora & Grabowski 1996: p. 631). Therefore cardiovascular dysfunction may potentially also result in the Rough pulse.
Conditions such as polycythemia vera, a genetically based disease that results in the overproduction of red blood cells and blood volume (sometimes twice as much as normal), may result in very sluggish blood flow due to the greatly increased viscosity of the blood (Guyton & Hall 2006: p. 428). This may cause increased turbulence of blood flow.
7.9.2.7. Comparison of definitions
There is a wide divergence of descriptions and indications for the Rough or Choppy pulse. It is traditionally described as ‘fine and slow’ (Li, Flaws (trans) 1998, Wang, Yang (trans) 1997) in the classical texts. Within these definitions, there are references to the pulse ‘coming and going with difficulty’ as well as terms such as ‘short’ and ‘scattered’. There are also references to an irregularity of rhythm ‘possibly one stop and again comes’ or ‘with an interruption but the ability to recover’.
When examining the individual parameters of the pulse the following points can be noted:
• Pulse rate: When authors do include ‘slow’ in their definitions of the Rough pulse, it is often then categorized with other pulses associated with a decrease in pulse rate, for example Li Shi zhen (Huynh (trans) (1985) and Deng (1999)). However, many modern CM definitions do not include change of rate in their interpretations of the Rough pulse. The term ‘slow’ could possibly be interpreted as a decrease in the rate at which systole and diastole occur within a cardiac cycle, which may also account for the phrase ‘coming and going with difficulty’ or the indication that the pulse feels ‘hesitant’ rather than slow (Lu 1996: p. 71).
• Pulse rhythm: The reference to the interruption of pulse rhythm is not expanded on in the traditional definitions; therefore it is difficult to be sure of their nature or the context in which they occurred. An interpretation of its use may have been to signify the severity of the underlying pathological process of blood vacuity or stasis, as was commonly attributed to the Rough pulse; in particular, the use of ‘possibly’ may imply that this was not the normal occurrence. As the presence of rhythm irregularities often indicate heart organ involvement, the appearance of dysrhythmias, in conjunction with the other changes in parameters that signify the Rough pulse, would seem to indicate the progressive severity of the condition.
Modern CM texts do not usually include the parameter of pulse rhythm in their definitions of the Rough pulse. Rather, the focus is on the texture of the blood flow and the changing pulse intensity.
• Pulse width: The term ‘fine’ continues to be used in modern definitions of the Rough pulse but is usually used in the context of the vacuity patterns only, particularly of blood or Essence (Jing). Therefore, it is not considered an essential part of the CM pulse definition.
Other pulse terms used to describe the Rough pulse
The terms ‘short’ and ‘scattered’ are sometimes utilised in the description of the Rough pulse. It is described as short by Maciocia (2004: p. 477) who notes that the pulse lacks ‘continuous movement between the three positions and does not feel like a wave’. However, this description is not a common component of other definitions for the Rough pulse.
‘Scattered’ is used in the traditional pulse definitions of the Rough pulse in the Mai Jing and The Lakeside Master’s Study of the Pulse. However it is poorly defined, if at all, and the possible interpretations of ‘scattered’ are too varied for this term to be of clinical use.
Hammer discusses the Choppy pulse as having ‘small ‘hills’ and ‘valleys’ as one rolls one’s finger along the pulse’ and ‘the varying heights are static’ (2002: p. 63). He further describes it as ‘like rubbing it [the finger] across a washboard’. Although these descriptions imply a variation in pulse wave height, he notes that the Choppy quality is ‘relatively stable and fixed in terms of the vertical movement and has little of the restive wave activity associated with Changing Intensity and Amplitude [a specific and separate pulse quality as defined by Hammer and his colleague, Dr Shen]’.
A common interpretation of the Rough pulse encompasses varying pulse force. However, Hammer identifies a distinctly separate pulse quality defined as a pulse having a change in intensity and amplitude (see above), and says that the Choppy pulse is not this type of pulse. It is therefore unclear whether the ‘hills’ and ‘valleys’ Hammer is referring to are a result of the actual arterial pulsation or alternatively, perhaps part of the physical structure of the artery wall, possibly referring to a tortuous arterial wall that is not smooth.
There are distinctive pulse qualities in biomedicine that could possibly be equated with the Rough pulse. For example, pulsus alternans is defined by pulse beats that alternate in strength. This can palpated as alternating increase and decrease in amplitude, hence a distinctive change in pulse amplitude despite having a regular rhythm. This is due to the alternating force of left ventricular contraction and is commonly indicative of severe impairment of left ventricular function. It can also occur during or after paroxysmal tachycardia (sudden increase in heart that may last from a few seconds to a number of hours). However, pulsus alternans can also be seen in individuals without heart disease for several beats following a premature or ectopic beat (a heart contraction that occurs before the normal contraction is expected (O’Rourke & Braunwald 2001: p. 1256). See section 6.6 for more information about ectopic beats and tachycardia.
It is possible that the Rough pulse was used to describe a number of pulses that exist but do not fit easily into any of the other standard CM pulse quality definitions. For example, a forceless pulse that has a slow rate of pressure increase, leading to a delayed systolic peak and subsequent slow collapse, correlates well with the description of the pulse as slow and going and coming with difficulty. This will also result in a forceless pulse due to the low volume (small pulse pressure), further fulfilling the descriptions of its decreased width. From a biomedical perspective, this is recognised as the pulsus parvus et tardus which often occurs with discrete obstruction to left ventricular output, for example occurring in aortic valve stenosis (O’Rourke et al 1992: p. 74).
7.9.3. Surging pulse (Hóng mài)

7.9.3.1. Alternative names
Flooding, Overflowing, Full, Tidal or Vast pulse.
7.9.3.2. Requisite parameters
The Surging pulse is a complex pulse quality with changes in three pulse parameters:
• Pulse contour and flow wave: The Surging pulse has a distinctive flow pattern, hitting the fingers distinctly but then pulse pressure decreases slowly.
• Pulse width: The arterial diameter is increased, resulting in a wide pulse.
• Force: There is an increase in pulse force
7.9.3.3. Clinical definition
The Surging pulse is a wide pulse. The initial part of the pulse wave pushes strongly against the side of the finger (in contrast to the Replete pulse, which pushes strongly upwards displacing the fingers vertically) but this is not sustained for the duration of the pulsation, continuing underneath the fingers with relatively diminished intensity. The most noticeable aspect of the pulsation is the initial forceful longitudinal movement of the pressure and flow wave, resulting in an expansion of the arterial wall.
7.9.3.4. Classical description from the Nei Jing and the Mai Jing
The surging pulse is a very large pulse [floating and large in another version] under the fingers.
When the pulse comes with much strength but goes completely weak, this is called the flooding pulse.
(Ni trans 1995: p. 32).
7.9.3.5. CM indications
The Surging pulse is now considered a pathological CM pulse quality associated with febrile disease, but it was traditionally described as the normal pulse for summer in the Nei Jing.
As a pathological pulse quality, the Surging pulse may be caused by either a replete external pathogen (Cold or Heat) or vacuity Heat pattern. These patterns include:
• Yang Ming stage of Six Division channel pattern identification
• Qi level of the Four Levels pattern identification
• Deficiency of Yin with hyperactivity of Yang.
Yangming stage of Six Division channel pattern identification
This theory deals with externally contracted febrile disease. The Yangming stage is the second stage and is associated with the progression of an external Cold pathogen into the interior of the body, transforming into extreme Heat. This pattern is usually accompanied by severe thirst and agitation, high fever, profuse sweating and the Surging pulse.
The Six Division pattern identification was initially mentioned in the Nei Jing but was described in greater detail in the Shan Han Lun, the classic text on externally contracted febrile disease.
From a CM perspective, high fever is a sign of that the body’s Zheng Qi is strong and fighting off a very strong pathogen. Subsidence of the fever is a sign that the Zheng Qi is overcoming the pathogenic factor (Wiseman & Ellis 1996: p. 226).
The Surging pulse reflects the transformation of the Cold pathogen into Heat, the subsequent increase in Yang and the struggle with the Zheng Qi. It also reflects the damage to fluids by the strong heat. This may be the cause of the pulsation’s tendency to hit the fingers strongly at first (increased Yang Qi) but then drop off gradually, as the fluids have been damaged and cannot sustain support for the Yang Qi (Yang is exuberant but Yin is weak).
Qi level of the Four Levels pattern identification
This theory also deals with externally contracted febrile diseases but is concerned with Heat pathogens and the effect of their progression into the interior of the body. In this particular pattern, an EPA of Heat transforms into severe heat and is very similar to the Yangming pattern described above. Signs and symptoms include high fever, severe thirst, agitation and profuse sweating. However, the Heat pathogen is able to transform into more severe heat much more rapidly than the previous pattern (Wiseman & Ellis 1996: p. 239).
As in the previous pattern, the Surging pulse is the result of the struggle between the Heat pathogen and the body’s Zheng Qi (Upright Qi).
Deficiency of Yin with hyperactivity of Yang
This is a severe vacuity-type pattern that results from the consumption of Yin and the resulting hyperactivity of Yang. This version of the Surging pulse is usually found in patients with very weak constitution due to chronic illness (leading to consumption of Yin) or complicated by severe loss of blood (Lu 1996: p. 104). In such circumstances the appearance of the Surging pulse signifies a bad prognosis.
Townsend & De Donna (1990) ascribe ageing, poor diet and excessive consumption of alcohol or drugs as possible factors responsible for diminished Yin and the manifestation of the Surging pulse. The severe vacuity of Yin can no longer control the Yang, which becomes hyperactive.
7.9.3.6. Biomedical perspective
Febrile disease has systemic effects on the circulation, increasing metabolic activity, regardless of the cause. Fever also causes certain mechanisms to place in order to reduce the body temperature. These include:
• Sweating
• Vasodilatation, which transfers heat to the skin to be dispersed.
Sweating increases greatly when the body’s core temperature rises above 37°C. A further increase of 1°C in temperature causes ‘enough sweating to remove 10 times the basal rate of body heat production’ (Guyton & Hall 2006: p. 895).
The vasodilatation may account for the increased width of the Surging pulse, and the increased metabolism may account for the perceived increase in pulse force. However, as noted in the clinical definition, this perceived force increase is not maintained for the duration of the pulsation. This may be the result of the injured fluids, depleted because of the increased fluid loss through compensatory sweating.
7.9.3.7. Comparison of similar CM pulse qualities
The Replete pulse is a pulse that is long and associated with either abundant Qi and blood (health) or Heat which agitates Qi and blood. Although both the Replete and Surging pulses are associated with Heat, the Surging pulse also signifies damage to fluids, which may occur concomitantly or may be pre-existing.
7.9.4. Stirred pulse (Spinning Bean pulse) (Dóng mài)

The Stirred pulse is not commonly seen. In some CM texts it is included as one of the ten ‘Unusual’ or ‘Death’ pulses and is generally considered to be associated with critical illness.
7.9.4.1. Alternative names
Spinning Bean, Stirring or Tremulous Pulse.
7.9.4.2. Requisite parameters
The Stirred pulse is a complex pulse quality that has changes in four pulse parameters:
• Pulse contour and flow wave: The pulse contour is rounded. It has a tendency to vibrate in its position, with a lack of smooth motion.
• Length: The Stirred pulse is a short pulse, occupying only one position, usually the Guan position.
• Rate: The pulse rate is rapid, >90 bpm.
• Force: There is an increase in pulse force.
7.9.4.3. Clinical definition
The Stirred pulse is rapid (>90 bpm) and short (occurring only in one position, usually the Guan position) and forceful, hitting the finger with intensity. It is noted for its quick succession of pulse pressure waves (‘vibrating’: rapid heart rate), with the pulse amplitude causing the arterial wall to be palpated by the finger as a ‘curved’ surface.
7.9.4.4. Classical description from the Mai Jing
The Shan Han Lun (Treatise on Cold Damage) says ‘Contention between Yin and Yang is called stirring … A rapid pulse that is perceptible only in the Guan with no ends in the upper or lower position. (i.e., the Cun or Chi) and which is large as a bean stirring and rotating in a small way is called a stirring pulse’
7.9.4.5. CM indications
The Stirred pulse usually occurs in an acute context, resulting from severe heat, trauma, pain, severe fright or cardiac-related dysfunction.
The Stirred pulse is associated with the severe disruption to the normal flow of Qi and blood and is considered to be the result of ‘Yin and Yang wrestling’ (Li, Flaws (trans) 1998: p. 116). The idea of two opposing yet interactive forces in dynamic motion has been an integral part of the philosophical theory underlying Chinese medicine, reflected by information in the Book of Changes (Yi Jing) which stated that ‘It is because hard and soft push each other that changes and transformations occur’ (Unschuld 2003: p. 85). Therefore the Stirred pulse may occur in sudden fright due to adverse flow of Qi and blood, whereas in physical trauma there may be severe obstruction of Qi and blood in the local area causing severe pain.
7.9.4.6. Clinical relevance
The Spinning Bean pulse is said to occur in reaction to sudden and extreme shock, fright, pain or physical trauma. It may be seen in severe fevers, myocardial infarction (heart attack), and shock (disturbance to normal circulation). Modern CM practitioners do not expect to see this pulse often in clinical practice, as these situations are more likely to be dealt with in an intensive care unit or other hospital settings.
7.9.4.7. Biomedical perspective
When the heart’s ability to pump blood becomes impaired, for example from myocardial infarction (decreased blood flow to heart muscle), circulatory reflexes are activated to restore cardiac output. This involves stimulation of the sympathetic nervous system and inhibition of the parasympathetic nervous system. Strong sympathetic stimulation has the dual effect of increasing the myocardial contraction and increasing the ability of blood to flow back to the heart. This greatly increases cardiac output. Heart activity also increases, increasing heart rate.
Circulatory shock similarly activates sympathetic reflexes to in an attempt to restore cardiac output, which may account for the increase in pulse rate and increased force.
7.10. Revision of the 27 CM pulse qualities
| Defining pulse parameter | CM pulse quality | Specific pulse parameters involved | Changes in pulse parameters present |
|---|---|---|---|
| Rate | Slow pulse (Chí mài) | Rate | Decreased ≤60 bpm |
| Rapid pulse (Shuò mài) | Rate | Increased ≥90 bpm | |
| Moderate pulse (Hūan mài) | Rate | 60 bpm | |
| Depth | Floating pulse (Fú mài) | Depth | Strongest at the superficial level |
| Sinking pulse (Chén mài) | Depth | Strongest at deep level | |
| Hidden pulse (Fú mài) | Depth | Strongest at deep level, deeper than Sinking pulse | |
| Length | Long pulse (Cháng mài) | Length | Extends beyond Cun, Guan and Chi |
| Short pulse (Dua.n mài) | Length | Cannot be felt in all three pulse positions | |
| Width | Fine pulse (Xì mài) | Width | Decreased width: narrow diameter |
| Rhythm | Skipping pulse (Cò mài) | Rhythm | Irregular interval between beats at irregular intervals |
| Rate | Increased ≥90 bpm | ||
| Bound pulse (Jié mài) | Rhythm | Irregular interval between beats at irregular intervals | |
| Rate | Decreased ≤60 bpm | ||
| Intermittent pulse (Dài mài) | Rhythm | Regularly irregular: consistently misses a beat in a distinctive pattern. No rate change |
| Defining pulse parameter | CM pulse quality | Specific pulse parameters involved | Changes in pulse parameters present |
|---|---|---|---|
| Arterial wall tension | Stringlike pulse (Xián mài) | Arterial wall tension | Increased arterial tension |
| Pulse occlusion | Retains form with increasing finger pressure | ||
| Length | Increased length: long | ||
| Tight pulse (Ji.n mài) | Arterial wall tension | Increased arterial tension | |
| Force | Increased force | ||
| Width | Increased diameter: wide | ||
| Length | Increased length: long | ||
| Scallion stalk pulse (Kōu mài) | Arterial wall tension | Increased arterial tension | |
| Force | Decreased force | ||
| Width | Increased diameter: wide | ||
| Depth | Strongest at the superficial level | ||
| Pulse occlusion | Easily occluded | ||
| Drumskin pulse (Gé mài) | Arterial wall tension | Increased arterial tension | |
| Force | Decreased force | ||
| Width | Increased diameter: wide | ||
| Depth | Strongest at the superficial level | ||
| Pulse occlusion | Easily occluded | ||
| Scattered pulse (Sàn mài) | Arterial wall tension | Greatly reduced arterial tension-little definition of arterial wall | |
| Force | Decreased force | ||
| Width | Increase in diameter: wide | ||
| Depth | Relatively strongest at the superficial level | ||
| Pulse occlusion | Very easily occluded | ||
| Force | Replete pulse (Shí mài) | Force | Increased force |
| Depth | Felt equally at all three levels of depth | ||
| Width | Increased diameter: wide | ||
| Length | Extends beyond Cun, Guan and Chi | ||
| Arterial wall tension | Increased arterial tension | ||
| Firm pulse (Láo mài) | Force | Increased force | |
| Depth | Strongest at the deep level | ||
| Width | Increased diameter: wide | ||
| Length | Extends beyond Cun, Guan and Chi | ||
| Arterial wall tension | Increased arterial tension | ||
| Vacuous pulse (Xū mài) | Force | Decreased force | |
| Depth | Strongest at the superficial level | ||
| Width | Increased diameter: wide | ||
| Pulse occlusion | Very easily occluded | ||
| Faint pulse (Wēi mài) | Force | Extreme lack of force | |
| Width | Very narrow | ||
| Pulse occlusion | Very easily occluded | ||
| Weak pulse (Ruò mài) | Force | Decreased force | |
| Depth | Strongest at the deep level | ||
| Width | Decreased diameter: narrow | ||
| Pulse occlusion | Easily occluded | ||
| Soggy pulse (Rú mài) | Force | Decreased force | |
| Depth | Strongest at the superficial level | ||
| Width | Decreased diameter: narrow | ||
| Pulse occlusion | Easily occluded | ||
| Pulse contour and flow wave | Slippery pulse (Huá Mài) | Pulse contour and flow wave | Smooth and rounded contour with a distinct expansion and contraction of arterial walls, conforming to flow wave. Can feel the pulse both arrive and depart smoothly. |
| Rough pulse (Sè mài) | Pulse contour and flow wave | Contour feels irregular or has uneven texture to the palpating fingers | |
| Force | Irregular: changes in intensity | ||
| Surging pulse (Hóng mài) | Pulse contour and flow wave | The flow wave has a distinct arrival under the finger and an indistinct departure. | |
| Width | Increased diameter: wide | ||
| Force | Increased force | ||
| Stirred (Spinning bean) pulse (Dòng mài) | Pulse contour | Rounded | |
| Flow wave | Vibrating due to quick succession of beats | ||
| Length | Usually felt in only one position | ||
| Rate | Increased: ≥90 bpm | ||
| Force | Increased force |
7.11. Using the pulse parameter system
Although much is made of the complexity of the pulse taking process, some CM authors believe that it should not be a difficult skill to learn, if both the theories and standard textbook definitions of each pulse quality are learnt and memorised (Porkert 1983, Flaws 1997). As discussed extensively in Chapter 4, the difficulties experienced in pursuit of this goal are usually due to the wide range of varying definitions that exist for the CM pulse qualities. The main aim of the pulse parameter system of pulse assessment is to limit the subjectivity of the process by providing a consistent methodology and concrete pulse definitions. As such, the integral components of the pulse parameter system are:
• Learning and memorising which pulse parameters are involved in the formation of each CM pulse quality and the nature of the changes occurring
• Understanding the theory and mechanisms underlying each of the pulse parameters
• Following a consistent methodology for examining the pulse, collecting and interpreting the pulse information.
A comprehensive knowledge of the clinical definitions and specific changes to pulse parameters for each of the 27 CM pulse qualities will enhance your ability to recognise them when they manifest themselves.
7.11.1. The appearance of multiple CM pulse qualities
As often noted in various CM pulse texts, it is not unusual for CM pulse qualities to appear in combination. However, in Chapters 6 and 7, an examination of the pulse parameter profiles reveals that there are some CM pulse qualities that simply cannot coexist. The Floating pulse and Sinking pulse cannot, by definition, appear simultaneously, likewise with the rate-related pulses. Another example of this was presented in Chapter 4 in the discussion of two complex pulse qualities, the Stringlike (wiry) pulse and Slippery pulse, which are primarily defined by two distinct pulse parameters. In this case, while a pulse may present with degrees of changes in both of these pulse parameters, neither is definitive enough to allow the pulse to be designated as either traditional CM pulse quality. To do so would lose valuable pulse information.
Pathogenic factors can often trigger changes in multiple pulse parameters that do not normally appear together as a particular CM pulse quality profile. For example, pathogenic Heat results in hyperactivity of Yang. This has the effect of agitating Qi and blood, resulting in an expansive movement of blood flow so that it can be felt in the radial artery as a length of pulsation, hence termed ‘long’. If the Heat is enough to elevate the body temperature then this results in an increased pulse rate. Therefore the pulse may be identified equally as both the Long and Rapid pulses. However, a Rapid pulse may occur without the Long pulse and vice versa.
Although changes in simple pulse parameters do occur together, it is usually a combination of these that lead to the identification of a specific CM pulse quality. For example, for a pulse that is found at the deep level of depth and cannot be felt at the superficial level, and is forceless and narrow, instead of identifying it as a forceless Sinking and Fine pulse, we would identify this as the Weak pulse.
Common combinations of CM pulse qualities often include a simple and a complex pulse quality. For example, assessment of the pulse during the onset of a cold or flu following exposure to cold climatic conditions may reveal pulse parameter profiles for both the Floating and Tight pulses, which may appear simultaneously in an EPA of Wind Cold. This would be described as a pulse that is forceful, has increased tension in the arterial wall that leads to a slight sideways movement and is found to be strongest a the superficial level of depth. The appearance of the pulse strongest at the superficial level of depth can be an indication that the exterior of the body is the focus of pathogenesis. In this particular case, the EPA has activated the Zheng Qi of the body so that Qi and blood rush to the surface as a defensive mechanism. The over-forceful nature of the pulsation indicates an excess within the body and signifies that both the Zheng Qi and pathogenic factor are strong, while the increased arterial tension reflects the effect of the Cold causing contraction of the muscles and blood vessels.
As such, these changes in the pulse parameters represent the pathological processes currently taking place in the body and signify specific changes in pulse parameters that are not normally linked together in any of the single traditional CM pulse qualities. Therefore, more than one CM pulse quality may be present.
Sometimes a pathogenic factor triggers changes in normal function (reflected in changes in pulse parameters) that, over time, can lead to changes in other pulse parameters and the transition of one CM specific pulse quality into another. Using the example above, the invasion of Wind Cold into the body presents with a Floating and Tight pulse. As the body’s defensive Qi struggles with the pathogen, this causes Heat, which agitates Qi and blood; but as the struggle progresses the Heat increases and this causes fluids to be depleted. This results in a progression of the pulse into the Surging pulse, still forceful but starting to slightly reflect the damage to Yin fluids. The increased arterial tension in the pulse has receded due to the transformation of the Cold pathogen into Heat. The concept of progression of illness and its effect on the pulse is explored further in Chapter 8.
7.11.2. Practical application of the pulse parameter system
In terms of applying this system to diagnostic practice, we need to ensure that we examine the pulse in a methodical way, looking at each one of the parameters. Table 7.5 outlines the aspects of the pulse that need to be examined each time. This is the first step in identifying any changes in pulse parameters.
| Pulse parameter | Factors to consider | Pulse assessment findings: Change in the pulse parameters Relevant diagnostic information |
|---|---|---|
| Rate | Beats per minute (bpm) | |
| Extraneous factors: exercise levels, medication, stress, caffeine intake, prior exertion (for example, exercise or hurrying)? | ||
| Rhythm | Is the rhythm regular (even intervals between each beat)? | |
| If there are irregularities, do these occur erratically or regularly? | ||
| How often? When? Accompanied by stress? | ||
| Does the person suffer from palpitations? | ||
| Depth | At what level of depth is the pulse the strongest? | |
| Can it be felt at all levels of depth? | ||
| Does the strength vary between levels? | ||
| Width | Is the pulse narrow or wide? | |
| Neither? Appropriate width? | ||
| Length | Can you feel the pulse at Cun, Guan and Chi? | |
| Can you feel it beyond Cun? | ||
| Can you feel it beyond Chi? | ||
| Does the artery wall have a continuous feel beneath the three fingers? That is, like a length of artery rather than having to feel the pulsation at each individual position? | ||
| Arterial wall tension | Can you feel the arterial wall clearly? | |
| Is there increased tension in the artery? Does the arterial wall feel hard? | ||
| Is it difficult to feel the arterial wall? | ||
| Force | Does the pulse strike the finger: | |
| Forcefully; | ||
| Without force; | ||
| With moderate force? | ||
| Ease of occlusion | Does the pulse occlude easily with little pressure? | |
| Does it feel ‘empty’ or lacking substance? | ||
| Does the artery feel solid, as though it is full? | ||
| Can you still the arterial distinctly wall even though the pulsation has been occluded? | ||
| Pulse contour and flow wave | Can you feel the both the ascending and descending change in pressure? | |
| Are they even in strength? | ||
| Can you feel the expansion and contraction of the artery walls? | ||
| Does the artery move side to side laterally? | ||
| Does the pulse move smoothly or unevenly under the finger? Does it have a particular shape? | ||
| Rounded, or does it vary in shape? |
With a clear understanding of the mechanisms that result in changes to individual pulse parameters, the appearance of CM pulse qualities in certain disease states or ill health may be better understood. This is important because often the presenting pulse does not fit any of the criteria of the 27 CM pulse qualities (Box 7.25). This does not necessarily mean that the pulse information cannot be used, as the changes in individual pulse parameters can be used to shed light on the pathogenic process that is taking place. For full details of the pulse taking procedure, see section 5.11.3.
Box 7.25
Hints for assessing pulse information
Sometimes we may find that the pulse we are palpating does not seem to fulfil all the parameter requirements of any of the specific TCM pulse qualities, or that the changes in parameters may be occurring in varying degrees. The decision then needs to be made whether another pulse assessment system may be more applicable, for example, Eight Principle, Five Phase or the Three Jiaos (see Chapter 9). Alternatively, we can utilise this pulse information by relating the changes in pulse parameters back to the theoretical effects on Yin, Yang, Qi and blood.
The general pulse assessment process is outlined in Figure 7.13. It is recommended that you make use of the checklist for the CM pulse qualities (Table 7.6) and the summary of the CM pulse qualities in Table 7.3 and Table 7.4 when you are initially starting to learn the pulse parameter system. These will help you to familiarise yourself with the terminology, pulse parameters and definitions for each of the CM pulse qualities, simplifying the identification process from the pulse information you have collected in Table 7.5. These tables are included for convenience but are not meant to be limiting, so include more information if you feel it is necessary.
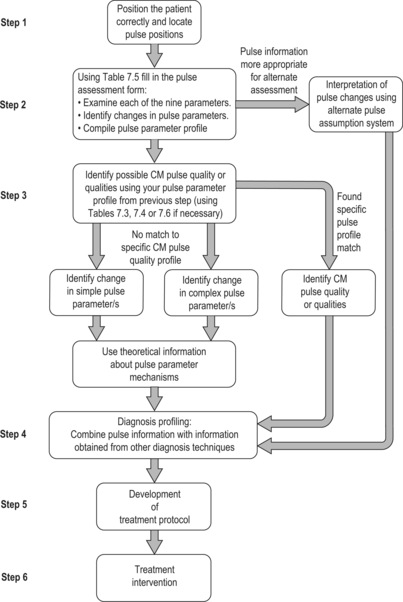 |
| Figure 7.13Pulse parameter assessment process. |
| TCM pulse quality | Rate | Rhythm | Depth | Length | Width | Arterial tension | Pulse contour and flow wave | Pulse occlusion | Force |
|---|---|---|---|---|---|---|---|---|---|
| Slow pulse (Chí mài) | ✓ | ||||||||
| Rapid pulse (Shuò mài) | ✓ | ||||||||
| Moderate pulse (Hūan mài) | ✓ | ✓ | |||||||
| Racing pulse (Jí mài) | ✓ | ||||||||
| Floating pulse (Fú mài) | ✓ | ||||||||
| Sinking pulse (Chén mài) | ✓ | ||||||||
| Hidden pulse (Fú mài) | ✓ | ||||||||
| Long pulse (Cháng mài) | ✓ | ||||||||
| Short pulse (Dua.n mài) | ✓ | ||||||||
| Fine pulse (Xì mài) | ✓ | ||||||||
| Skipping pulse (Cò mài) | ✓ | ✓ | |||||||
| Bound pulse (Jié mài) | ✓ | ✓ | |||||||
| Intermittent pulse (Dài mài) | ✓ | ||||||||
| Stringlike (Wiry) pulse (Xián mài) | ✓ | ✓ | ✓ | ||||||
| Tight pulse (Jin mài) | ✓ | ✓ | ✓ | ✓ | |||||
| Scallion Stalk pulse (Kōu mài) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Drumskin pulse (Gé mài) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Scattered pulse (Sàn mài) | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Replete pulse (Shí mài) | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Firm pulse (Láo mài) | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Vacuous pulse (Xū mài) | ✓ | ✓ | ✓ | ✓ | |||||
| Weak pulse (Ruò mài) | ✓ | ✓ | ✓ | ✓ | |||||
| Faint pulse (Wē i mài) | ✓ | ✓ | ✓ | ✓ | |||||
| Soggy pulse (Rú mài) | ✓ | ✓ | ✓ | ✓ | |||||
| Slippery pulse (Huá mài) | ✓ | ||||||||
| Rough pulse (Sè mài) | ✓ | ✓ | |||||||
| Surging pulse (Hóng mài) | ✓ | ✓ | ✓ | ||||||
| Stirred (Spinning Bean) pulse (Dòng mài) | ✓ | ✓ | ✓ | ✓ |
7.11.3. Using the CM theory underlying the pulse parameters
Having identified the pulse parameters involved, use the checklist (Table 7.3) to note whether your parameter profile correlates with any of the 27 CM pulse qualities. You may find more than one CM pulse quality, as it is common for them to occur in conjunction with one another. For example, if the pulse rate is 95 bpm and equally strong at all three levels of depth, hits the fingers forcefully, is felt beyond Chi and is wide with a well-defined arterial wall, we would identify both the Rapid and Replete pulses.
However, what do you do if, having evaluated the pulse, you find that the pulse profile does not fit any of the specific CM pulse qualities? Rather than trying to fit any changes in pulse parameters into a specific pulse quality profile, and risk losing valuable pulse information, another way of utilising the information obtained from radial pulse palpation is to relate the changes occurring in the pulse and accompanying signs and symptoms, to the effect on the different substances, such as Qi, Yang, Yin, and Blood, involved in the formation of the pulse. The mechanisms behind the pulse parameters have been discussed in detail throughout Chapters 6 and 7, in the accounts of the specific CM pulse qualities. Table 7.3 and Table 7.4 briefly summarise this information, noting the effect on the pulse parameters. Note that this is a theoretical construct, so although this information may generally apply in most cases, occasionally there may be some contradictory findings. Remember that pulse diagnosis is only part of the holistic diagnostic procedure employed in order to gain a complete understanding of the patient’s presenting problems and, as such, was not intended as a solitary diagnostic technique.
This concludes our account of the pulse parameter assessment system. The next chapter explores the connections that exist between many of the CM pulse qualities in terms of their shared pathological mechanisms and progression of disease.
References
R Amber, A Babey-Brooke, Pulse diagnosis: detailed interpretations for eastern and western holistic treatments. (1993) Aurora Press, Santa Fe, NM .
D Chen, J Clarke, Analysis of a clinical sign in traditional Chinese medicine using Doppler ultrasound, Australasian Radiology 45 (2001) 452–456 .
S Chen, Y Lin, Q Meng, et al., Comparative study on the mechanism of formation of pulse manifestations in coronary heart disease and hematopathic patients, Journal of Traditional Chinese Medicine June 16 (2) (1996) 143–146.
JR Cockcroft, IB Wilkinson, DJ Webb, Age, arterial stiffness and the endothelium, Age and Aging 26-S4 (1997) 53–60.
S Clavey, Fluid physiology and pathology in traditional Chinese medicine. (1995) Churchill Livingstone, South Melbourne .
J Coad, M Dunstall, Anatomy and physiology for midwives. 2nd edn. (2005) Elsevier, Edinburgh .
T Deng, Practical diagnosis in traditional Chinese medicine. (1999) Churchill Livingstone, Edinburgh .
ME Estes, Health assessment and physical examination. 3rd edn. (2006) Thomson Delmar Learning, Southbank, Vic .
B Flaws, The secret of Chinese pulse diagnosis. 2nd edn. (1997) Blue Poppy Press, Boulder, CO .
C Giannattasio, M Failla, A Grappiolo, et al., Fluctuations of radial artery distensibility throughout the menstrual cycle, Arteriosclerosis, Thrombosis & Vascular Biology 19 (1999) 1925–1929.
A Guyton, J Hall, Textbook of medical physiology. 11th edn. (2006) Elsevier Saunders, Philadelphia .
Guangzhou Chinese Medicine College April, 1991 Inspection of the tongue and pulse taking. April. Guangzhou, China
L Hammer, Workshop: tradition and revision, Clinical Acupuncture and Oriental Medicine 3 (2002) 59–71.
TJ Kaptchuk, Chinese medicine: the web that has no weaver. (2000) Random House, London .
BA Kelly, P Chowienczyk, Vascular compliance, In: (Editors: BJ Hunt, L Poston, M Schachter, AW Halliday) An introduction to vascular biology: from basic science to clinical practice 2nd edn (2002) Cambridge University Press, Cambridge.
E King, D Cobbin, S Walsh, et al., The reliable measurement of radial pulse characteristics, Acupuncture in Medicine 20 (4) (2002) 150–159.
SZ Li, B Flaws, The lakeside master’s study of the pulse. (1998) Blue Poppy Press, Boulder, CO .
SZ Li, HK Huynh, GM Seifert, Pulse diagnosis by Li Shi Zhen. (1985) Paradigm, Brookline, MA ; (translator) (editor).
Y Lu, Pulse diagnosis. (1996) Science and Technology Press, Jinan .
J Lyttleton, Treatment of infertility with Chinese medicine. (2004) Churchill Livingstone, Edinburgh .
KL McCance, SE Huether, Pathophysiology: the biologic basis for disease in adults and children. (2006) Elsevier Mosby, St Louis .
G Maciocia, The foundations of Chinese medicine. (1989) Churchill Livingstone, Edinburgh .
G Maciocia, Obstetrics and gynaecology in Chinese medicine. (1998) Churchill Livingstone, Edinburgh .
G Maciocia, Diagnosis in Chinese medicine: a comprehensive guide. (2004) Churchill Livingstone, Edinburgh .
M Ni, The Yellow Emperor’s classic of medicine: a new translation of the neijing suwen with commentary. (1995) Shambala, Boston ; (translator).
MF O’Rourke, RP Kelly, AP Avolio, The arterial pulse. (1992) Lea & Febiger, Philadelphia .
R O’Rourke, E Braunwald, Physical examination of the cardiovascular system, In: (Editors: E Braunwald, A Fauci, D Kaspar, et al.) 15th edn Harrison’s principles of internal medicine, Volume 1 (2001) McGraw-Hill, New York; Ch 225.
M Porkert, The essentials of Chinese diagnostics. (1983) Acta Medicinae Sinensis Chinese Medicine Publications, Zurich .
L Poston, D Williams, Vascular function in normal pregnancy and preeclampsia, In: (Editors: BJ Hunt, L Poston, M Schachter, AW Halliday) An introduction to vascular biology: from basic science to clinical practice 2nd edn. (2002) Cambridge University Press, Cambridge.
C Rogers, The five keys: an introduction to the study of traditional Chinese medicine, 3rd edn revised. (2000) Acupuncture Colleges Publishing, Sydney .
In: (Editors: D Stables, J Rankin) Physiology in childbearing with anatomy and related biosciences (2006) Elsevier, Edinburgh.
GJ Tortora, SR. Grabowski, Principles of anatomy and physiology. 9th edn. (2000) John Wiley & Sons, Inc., New York .
G Townsend, Y De Donna, Pulses and impulses. (1990) Thorsons, Wellingborough .
P Unschuld, Huang di nei jing su wen. (2003) University of California Press, Berkerley .
S Walsh, The radial pulse: correlation of traditional Chinese medicine pulse characteristics with objective tonometric measures [PhD]. (2003) University of Technology, Sydney .
SH Wang, S Yang, The pulse classic: a translation of the mai jing. (1997) Blue Poppy Press, Boulder, CO ; (translator).
N Wiseman, A Ellis, Fundamentals of Chinese medicine, revised edn. (1996) Paradigm, Brookline, MA ; (translators and editors).
N Wiseman, F Ye, A practical dictionary of Chinese medicine 2nd edn. (1998) Paradigm, Brookline, MA .