Complementary Therapies as Cardiovascular and Pulmonary Physical Therapy Interventions
What Are Complementary Therapies?
The goal of most of these therapies is to “unblock” obstructed body energy so that the body can heal itself.1 It is hypothesized that homeostasis, balance, and self-regulation (the highly advanced ability of the body/mind to supply optimum conditions for metabolism, such as proper pH, body temperature, etc.) result from the unrestricted flow of body energy, along with molecules from breathing, fluid, and nutrition.2,3 A system out of balance becomes vulnerable to early mortality. A system in balance becomes resistant to inflammation. Some suggest that inflammation is the foundation of all diseases and disorders.4 Two large studies, one in men and one in women, demonstrated that higher levels of C-reactive protein correlate with a higher risk for heart attack and stroke and treatments that reduce C-reactive protein level reduce heart disease risk.5,6 Therefore complementary therapies are used to facilitate the flow of body energy (or chi) and thus help the body restore balance and return to a healthier state.
Examples of Complementary and Alternative Therapies
The following are examples of complementary and alternative therapies that have been found to be useful in health care. A list and brief description of these therapies can be found in Appendix E.
Manual Therapies
Manual therapies, also known as body work, include myofascial release, craniosacral therapy, Rosen method, Rolfing, Hellerwork, soma, neuromuscular therapy, massage, and osteopathic and chiropractic medicine. The manual therapies involve the use of hands on the body/mind surface to stimulate bioelectromagnetic force. How this occurs remains a mystery. Research by Hunt and others is currently being conducted to measure energy flow from the body.7–9 Perhaps both mechanical and energetic forces stimulate response from the tissue in several ways. It has been hypothesized that mechanical force may be transformed into a chemical response within the collagen of the myofascia, causing a flow of the polyglycoid layer of the collagen by way of a piezoelectric effect.10 For patients with cardiovascular and pulmonary pathology, the manual therapies can assist in opening up the ribcage and vertebral spine to allow increased ventilation and better posture, thereby supporting cardiorespiratory health.
Mind/Body Interventions
Mind/body intervention include psychotherapies, support groups, meditation, imagery, hypnosis, dance and music therapy, art therapy, prayer, neurolinguistic psychology, biofeedback, yoga, Pilates, and tai chi. These interventions are examples of how movement and verbal and nonverbal communication with the mind/body can open up new pathways for thought and thereby unblock potentially blocked energy flow or chi. Likewise, with the new understandings of epigenetics (see discussion below), the energy (or vibration) of one’s perception or belief drives DNA function, either for means of growth or for means of protection/survival.2,3 These interventions are quite prevalent in the treatment of cardiorespiratory and pulmonary disorders. Stress is positively affected when the person is aware of thoughts and habits that affect the mind/body in a negative way. These interventions put the patient back in control of negative behaviors, and focusing on the breath is often an integral part of furthering relaxation.
Energy Work
Bioelectromagnetics
Bioelectromagnetics include thermal applications of magnets and nonionizing radiation such as radiofrequency hyperthermia laser and pulsed electromagnetic field therapy. Credible research exists on the effects of electromagnetic energy for wound healing and bone repair. Biomicroelectromagnetics is the term applied to the energy that seems to emanate from the hands of people who have been accepted as healers.8 Ultrasound and diathermy have been used in physical therapy for decades as deep heat mechanisms, and although there is not a clear understanding of the mechanism of action, it undoubtedly involves a stimulation of energy flow; therefore this therapeutic approach falls in the bioelectromagnetic category. The use of magnets in physical therapy is quite controversial, but there are some very compelling results from case studies that make it important to include in this category.
Herbal Approaches
Naturopathy and homeopathy represent the use of plants and animal substances to fight off disease and the use of wise nutrition to combat illness. Naturopathy, like osteopathic medicine, represents an entire system of health care that uses homeopathy, osteopathy, proper nutrition, and other means to bring about healing. Naturopathic physicians complete 4 years of medical school. Homeopathy involves the use of minute chemicals in diluted solution to resolve chemical imbalances in the body. Proper nutrition has long been associated with cardiac and pulmonary health, especially in Dean Ornish’s plan for healing from cardiac pathology.11
Mind/Body Link
Mind/body health care has brought about a way of linking the traditional linear research methods with the more contemporary, complementary, and alternative health care practices. The influence of the mind on the body was first introduced in the Western hemisphere by Herbert Benson, a well-known Harvard cardiologist, through his research on Tibetan monks who were able to control their autonomic nervous system to the extent that they could lower their body temperatures and respiration rates and enter a wakeful, hypometabolic physiological state by will.12 This information shocked the Western world, and Benson presented his data most dramatically by videotaping the actual sessions of the monks taking control of their bodies with their minds.
The proof that the mind and body are inextricably linked has since been well documented in various studies. Indeed, there is a basic science devoted to the study of the effect of the mind on the body: psychoneuroimmunology, a term that Ader and Cohen are credited with creating. Studies have shown that the mind affects the immune system by way of the autonomic nervous system and by way of the “fluid” nervous system, or the nonadrenergic and noncholinergic nervous system.13
Candice Pert has clearly articulated the physiological functioning of the fluid nervous system, which manifests by way of the effects of thought on the neurotransmitters, the neuropeptides, and the steroids of the body.14 The neurotransmitters and the neuropeptides communicate with most of the cells of the body. This science has been termed psychoneuroendocrinology. It is no longer correct to assume that the mind resides only in the cranium or the brain. In truth, the mind has been shown to reside in every cell in the body. According to Pert and others, the science clearly reveals that all cells have memory.14 The biochemistry of psychoneuroendocrinology reflects a flow that is different from that of microelectro-potentials or the exchange of energy from the hands of the therapist, but which illustrates, nonetheless, that the mind and the body are inseparable and the mind communicates with every cell of the body.
Complementary and alternative therapies are energy-based therapies that require an understanding that there is such a phenomenon as vital flow of energy in the body and that the natural state of the body is to be healthy.15 Cells are constantly in a state of flux, with old cells dying off and new cells being created continuously. But the body/mind persists in continuously working toward fighting off disease and healing cells whose loss would threaten the thriving of the entire system. With this awareness, illness is understood as an aberration set up by an imbalance caused by restriction in flows. The body has many energies, or vibrations, and the ways that we can observe energy at work in the body are varied. For example, electrocardiograms, electroencephalograms, and electromyograms all measure the energy output from various body organs. The piezoelectric effect, another energy phenomenon, enables osteoblastic activity, which keeps our bones strong. Mechanical energy in gravity is transformed to chemical energy to allow the osteoblasts to deposit calcium appropriately in our skeleton. But now we understand that perhaps the most powerful of the many vibrations our cellular receptors respond to is the vibration of perception.
The science of epigenetics posits that the genes in our cells respond to vibrational signals. For the cells to function, receptors on the surface of the cell wall must respond to the vibration to which they are attuned, resulting in a cascade of actions that lead to the DNA ordering the appropriate protein chain linkage to result in the needed function.2,14 Basic to the understanding of the mind and body being inseparably linked is the fact that one of the most powerful vibrations that cells respond to is the vibration of perception or belief.2,14 The more a person perceives threat, stress, or danger, the more there is a resulting vibration to which cells respond with an autonomic fight or flight response—the hypothalamic-pituitary-adrenal (HPA) axis.16 It has been long understood that chronic stress contributes to pathology in the cardiovascular and pulmonary systems. The DNA of cells is responding in a “digital” (on-or-off) way either to signals vibrating for growth needs or signals vibrating for protection needs. When protection needs take over, blood is shunted to life-sustaining viscera and to the extremities for flight or fight. Thus some organs are not being nourished in a health-producing manner. Over time, immune system function is also diminished and this can lead to inflammation and disease of the heart and lungs.17 A system out of balance becomes vulnerable to early mortality. A system in balance becomes resistant to inflammation. As stated previously, some suggest that inflammation is the foundation of all diseases and disorders.4
Biomicroelectro-potentials, or the subtle energies in electromagnetic fields that emanate from the hands of “healers,” are currently being researched.8,18 It is believed that complementary and alternative therapies have an effect on patients by way of the energy that emanates from the healer’s hands. This energy is of a frequency of 0.3 to 30 Hz, which is usually centered around 8 to 10 Hz.19,20
Most current diseases, especially the chronic diseases that affect people, do not lend themselves to single-purpose cures. Chronic illness is most adequately addressed when the patient is involved in the healing process as an active partner, when the patient is willing to make certain lifestyle changes to eliminate choices that interfere with wellness, and when illness is perceived by patients and practitioners not as a simple biophysiological event but as a system or contextual event. We are all consciously and unconsciously influenced by a variety of systems that we are embedded within and that mandate our reactions to inflammation and illness. No two people react to illness in the exact same way, and no two people heal from illness in the exact same way. Practically any physical therapist or health care professional will admit that how a person thinks or perceives has an enormous amount to do with how he or she responds to health and illness. A vast range of systems affect all of us at any given time—just a few examples are our birth order, our identity, how we feel about ourselves and our family members, how well we enjoy our work and our recreation, how meaningful our relationships are, what the weather is like, who won the Super Bowl, and what we ate for breakfast.21
Traditional Therapies Applied from a Holistic Approach—Intention
Researchers confirm the importance of hope and faith in one’s physician and practitioners, including physical therapists.22 It has been established that a patient’s belief that the practitioner has hope for the patient’s recovery seems to help, but exactly how this facilitates healing remains unclear. It seems to be related to the concept of intention and the effects of consciousness and nonlocal mind.22
To ignore the positive effect of therapeutic presence is to neglect a powerful intervention. How practitioners interact with their patients, not just what they do, is vitally important.1 Time and again, patients mention that a critical factor in their healing response was the positive effect of being truly listened to by their care provider. Now research is finally documenting the effects of positive intention and the therapeutic exchange of energy.22
The Problem of Scientific Evidence
Complementary therapies such as tai chi, acupuncture, biofeedback, meditation, cognitive behavioral therapy, music therapy, hypnosis, electrical stimulation, prayer and distant healing efforts, yoga, and qi gong have been shown to be effective in the relief of pain and anxiety and in the improvement of balance by way of the randomized controlled trial (RCT).23 Literature reviews of mind/body therapies in the treatment of musculoskeletal disorders with implications for older adults have been conducted.24,25 Still, the fact remains that many complementary therapies, especially those manual therapies designed to assist in the release of fascial restrictions in order to restore the flow of the body’s self-regulating energy, do not lend themselves to study by the RCT because energy itself cannot be measured or seen. Only the results of energy can be measured (heat, work, movement, etc.), and we cannot yet validate what results occur from what intervention, except by way of anecdote and measuring the effects of treatment on impairments and function. However, scientists such as Valerie Hunt, James Oschman, Gary Schwartz, Linda Russek, Candace Pert, and others are busy working out the biochemical, quantum physics, and systems theories that postulate physiological and biochemical mechanisms of action, which will allow us to hypothesize basic cellular energy theory.10,26–28 This basic cellular energetic theory can then be tested to describe the evidence that we need. If we can hypothesize a basic mechanism of action of myofascial release, for example, then we can examine whether that action does indeed take place in the way that the theory postulates. However, we will never be able to see energy, any more, for instance, than we can see velocity.
Demonstration of efficacy and safety is paramount to professional care. But is this goal actually achievable to the satisfaction of the scientific community? Not as long as reductionism remains the gold standard in the search for reality. In 1997, the Council on Scientific Affairs of the American Medical Association suggested that “physicians should evaluate the scientific perspectives of unconventional theories for treatment and practice, looking particularly at potential utility, safety and efficacy of these [holistic] modalities.”23
Use of Specific Complementary Therapy Interventions in Cardiovascular and Pulmonary Conditions
As described throughout Part III of this book, the goal of physical therapy intervention is to improve the efficiency of the oxygen transport and gas exchange systems. The decision to use a specific complementary therapy and integrate it into more traditional cardiovascular and pulmonary treatments is often dependent on the practitioner’s familiarity with the intervention. Rehabilitation practitioners without specialized training in a complementary therapeutic intervention frequently do not realize that they are already incorporating components of complementary therapies in established, traditional therapeutic interventions. Patient education, including behavioral and biofeedback techniques used to alter breathing patterns and reduce sympathetic nervous system stimulation, are forms of mind/body therapies. These interventions have been studied extensively, reported in the literature, and are widely used and accepted in clinical practice.29–31
Physical therapy practitioners with expertise in a specific complementary intervention may decide to focus their treatment on cardiovascular and pulmonary impairments. Tai chi and yoga are mind/body therapies that emphasize coordinated breathing with movement. These interventions may be used as the primary approach to treat the impairment, or they may complement traditional physical therapy. The body of evidence addressing the usefulness of these interventions in improving oxygen transport has expanded in both quantity and quality in recent years.32–36
Other interventions that have not been subjected to rigorous, scientific study may still be worthy of clinical application. For example, the Alexander technique, which emphasizes posture and movement, intuitively suggests an improvement in oxygen transport. An improvement in posture optimizes muscle function, thoracic cage efficiency, and hence oxygen transport; however, there is limited research published on this technique in relation to the cardiovascular and pulmonary systems.37
The increasing consumer demand for complementary and alternative medical (CAM) therapies has occurred despite the lack of rigorous or acceptable scientific investigation into many of them. In an attempt to protect the general public from unethical and unsafe practices, the National Heart, Lung, and Blood Institute and the National Center for Complementary and Alternative Medicine (NCCAM) have proposed that large-scale clinical trials be performed to determine standards of practice and safety standards.38 NCCAM proposed initiatives to support research and the development of specialized centers to study cardiovascular disease and also reported a 96% increase in funding for these initiatives in 2005.39,40 It is important for all health care practitioners to become familiar with some of the more popular CAM therapies, recognize that our patients are using them, and be especially aware of the effects of these therapies on the cardiovascular and pulmonary systems.
Cardiovascular and Pulmonary Responses to Complementary and Alternative Medical Therapies
Tai Chi
Tai chi is one of the most well-studied mind/body therapies. During sessions of the many forms of tai chi (see Appendix E), cardiovascular responses have been documented in novices as well as in master practitioners. In several of these studies, responses have been compared to cardiovascular and pulmonary responses observed in other forms of exercise (e.g. bicycle ergometry and treadmill ambulation). Most investigations are small and have methodological shortcomings. A brief sampling of the results of several studies addressing the cardiovascular and pulmonary responses found during tai chi practice can be found in Table 27-1. In general, in these studies of healthy individuals, gender and experience level do not seem to influence the responses. It is reasonable to conclude that tai chi is a low- to moderate-intensity exercise that emphasizes the oxygen transport system. Investigators generally conclude that tai chi is a safe activity for healthy individuals. Prescreening for mind/body interventions is recommended, however, just as would be expected for any other exercise intervention.37
Table 27-1
Cardiovascular and Pulmonary Responses Found During Continuous Tai Chi Exercise
| Study Authors | Tai Chi Form | Sample Characteristics and Methods | Cardiovascular and Pulmonary Responses |
| Schneider, 199141 | Wing chun (WG) Tai chi chuan (TCC) |
Experienced practitioners measured on treadmill measured on treadmill |
TCC: 36.4%  , 59.8% HRmax, , 59.8% HRmax,  21.7 21.7WG: 52.4%  , 70.5% HRmax, , 70.5% HRmax,  24.2 24.2 |
| Lan, 200142 | Yang tai chi chuan | 15 men Age 26-56 years Experienced practitioners (>1 year)  measured on cycle ergometer measured on cycle ergometer |
TCC: 58% HRmax (max on cycle was 186 ± 8), 55%  (max on cycle was 39.1 ± 7.7) (max on cycle was 39.1 ± 7.7) |
| Brown, 198943 | Tai chi chuan (long form Yang style, Cloud H) | 6 men Experienced practitioners  measured on cycle ergometer measured on cycle ergometer |
TCC: Vf 11.3,  23.47, VD/VT 20% Cycle: Vf 15.7, 23.47, VD/VT 20% Cycle: Vf 15.7,  27.41, VD/VT 27% 27.41, VD/VT 27%Cardiac output, stroke volume, and HR were not significantly different between TCC and ergometry at the same  |
| Fontana, 200044 | Tai chi in slow and fast movements in sitting and standing | 26 healthy adults Age 21-50 years Convenience sample Novice and experienced practitioners |
METs: Sitting 1.5 ± 0 .2, Slow standing 2.3 ± 0.3, Fast standing 2.6 ± 0.5, Breathing exercises 3-3.6, 43%-49% predicted HRmax |
| Chao, 200245 | Tai-chi/qi-gong (54 motions divided into 3 sets) | 47 adults Age 32-76 years Experienced practitioners (mean 3.6 ± 2.6 years) |
50%  in older adults (≥65 years) 60% in older adults (≥65 years) 60%  in women in womenEach motion ± 3 METs |
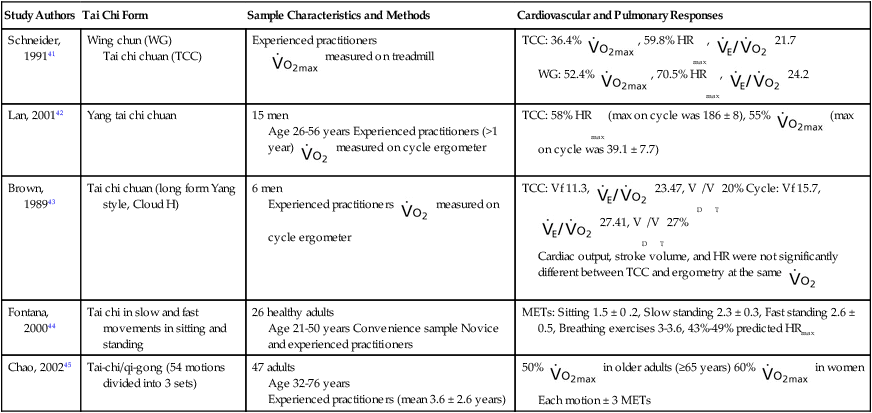
Several authors have investigated the cardiovascular and pulmonary benefits of a prolonged program of tai chi. In contrast to the studies reported in Table 27-1, several others demonstrate that experienced tai chi chuan practitioners achieve significantly higher maximum oxygen consumption ( ) levels than do sedentary subjects.46–52 These authors conclude that tai chi is a form of aerobic exercise, it has benefits for health-related fitness, and it may slow the decline in cardiorespiratory fitness in older, healthy individuals.
) levels than do sedentary subjects.46–52 These authors conclude that tai chi is a form of aerobic exercise, it has benefits for health-related fitness, and it may slow the decline in cardiorespiratory fitness in older, healthy individuals.
In a small study (n = 32), Wang and colleagues (2002)34 studied endothelium-dependent dilation in skin vasculature in healthy, older (69.9 ± 1.5 years), male tai chi practitioners and a control group. Their results demonstrate that when compared with older sedentary men (67.0 ± 1.0 years), long-time, experienced practitioners of tai chi have more favorable arterial and venous hemodynamics. In some cases these vascular findings were comparable to a group of younger, healthy, sedentary men (23.5 ± 0.68 years).
Young and colleagues (1999)53 compared the effects of aerobic exercise and tai chi on blood pressure responses in older individuals (79% women). In this RCT of 62 sedentary older adults (66.7 ± 5.2 years), subjects participated in 12 weeks of either aerobic exercise or tai chi. Baseline systolic blood pressure (BP) was 130 to 159 mm Hg. Subjects were not on antihypertensive medication, and results indicated similar statistically significant reductions in systolic BP occurred in both intervention groups. Of note, the aerobic exercise group demonstrated a significant increase in predicted  , whereas the tai chi group did not. The authors concluded that both light- and moderate-intensity exercise programs can have an important effect on systolic blood pressure. Thornton and colleagues (2004)54 found similar reductions in BP in normotensive sedentary women, ages 33 to 55 years. In contrast, Chen and colleagues (2006)55 found no reduction in BP in older adult residents of long-term care facilities when they participated in a 6-month simplified tai chi program. Their program was customized for deconditioned subjects, and the authors concluded that the lack of significant changes in BP was due to the very low intensity of the exercise.
, whereas the tai chi group did not. The authors concluded that both light- and moderate-intensity exercise programs can have an important effect on systolic blood pressure. Thornton and colleagues (2004)54 found similar reductions in BP in normotensive sedentary women, ages 33 to 55 years. In contrast, Chen and colleagues (2006)55 found no reduction in BP in older adult residents of long-term care facilities when they participated in a 6-month simplified tai chi program. Their program was customized for deconditioned subjects, and the authors concluded that the lack of significant changes in BP was due to the very low intensity of the exercise.
Yoga
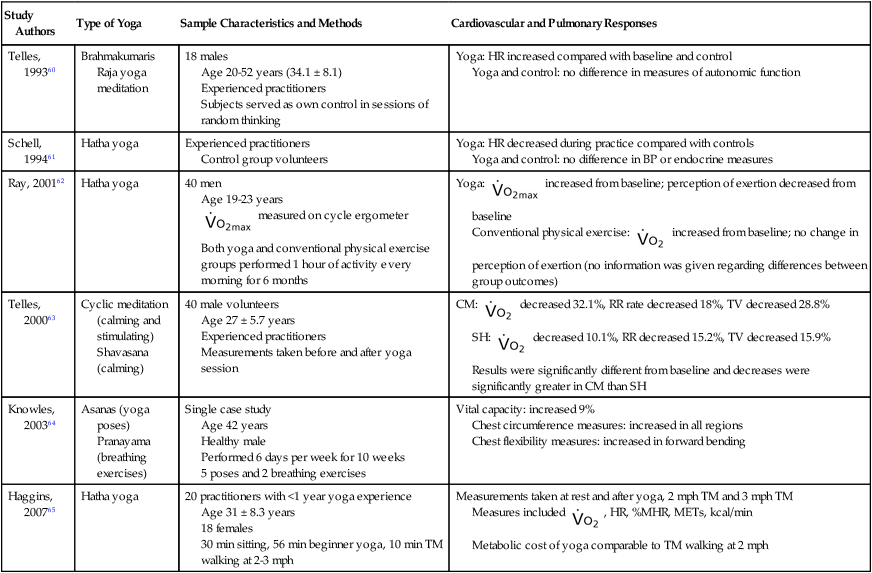
Another popular mind/body intervention is yoga. The cardiovascular responses to several types of yoga in healthy children and adults have been investigated.56–59 General conclusions are difficult to make, given the weaknesses of the studies and the different characteristics of the types of yoga studied. Table 27-2 lists cardiovascular and pulmonary responses before and after a single yoga session or a period of yoga practice. Overall it appears that those forms of yoga that primarily involve meditation show minimal changes in cardiovascular and pulmonary parameters when compared with those forms that include stimulation phases.
Table 27-2
Cardiovascular and Pulmonary Responses to Yoga Practices in Healthy Individuals
| Study Authors | Type of Yoga | Sample Characteristics and Methods | Cardiovascular and Pulmonary Responses |
| Telles, 199360 | Brahmakumaris Raja yoga meditation | 18 males Age 20-52 years (34.1 ± 8.1) Experienced practitioners Subjects served as own control in sessions of random thinking |
Yoga: HR increased compared with baseline and control Yoga and control: no difference in measures of autonomic function |
| Schell, 199461 | Hatha yoga | Experienced practitioners Control group volunteers |
Yoga: HR decreased during practice compared with controls Yoga and control: no difference in BP or endocrine measures |
| Ray, 200162 | Hatha yoga | 40 men Age 19-23 years  measured on cycle ergometer measured on cycle ergometerBoth yoga and conventional physical exercise groups performed 1 hour of activity every morning for 6 months |
Yoga:  increased from baseline; perception of exertion decreased from baseline increased from baseline; perception of exertion decreased from baselineConventional physical exercise:  increased from baseline; no change in perception of exertion (no information was given regarding differences between group outcomes) increased from baseline; no change in perception of exertion (no information was given regarding differences between group outcomes) |
| Telles, 200063 | Cyclic meditation (calming and stimulating) Shavasana (calming) |
40 male volunteers Age 27 ± 5.7 years Experienced practitioners Measurements taken before and after yoga session |
CM:  decreased 32.1%, RR rate decreased 18%, TV decreased 28.8% decreased 32.1%, RR rate decreased 18%, TV decreased 28.8%SH:  decreased 10.1%, RR decreased 15.2%, TV decreased 15.9% decreased 10.1%, RR decreased 15.2%, TV decreased 15.9%Results were significantly different from baseline and decreases were significantly greater in CM than SH |
| Knowles, 200364 | Asanas (yoga poses) Pranayama (breathing exercises) |
Single case study Age 42 years Healthy male Performed 6 days per week for 10 weeks 5 poses and 2 breathing exercises |
Vital capacity: increased 9% Chest circumference measures: increased in all regions Chest flexibility measures: increased in forward bending |
| Haggins, 200765 | Hatha yoga | 20 practitioners with <1 year yoga experience Age 31 ± 8.3 years 18 females 30 min sitting, 56 min beginner yoga, 10 min TM walking at 2-3 mph |
Measurements taken at rest and after yoga, 2 mph TM and 3 mph TM Measures included  , HR, %MHR, METs, kcal/min , HR, %MHR, METs, kcal/minMetabolic cost of yoga comparable to TM walking at 2 mph |
Other Mind/Body Therapies
Although social support is not typically considered a mind/body therapy, part of the success of many of the CAM interventions has been attributed to group interactions or those interactions between subject and practitioner. In a review of 81 studies, Uchino and colleagues (1996)66 investigated the benefits of social support on the cardiovascular, endocrine, and immune systems. Social support includes individual, family, or group interactions. There is strong evidence correlating a decrease in cardiovascular reactivity in healthy individuals when social support is increased.
Manual Therapies/Body Work Therapies
There is a paucity of literature addressing cardiovascular and pulmonary responses to body work interventions in healthy individuals. One study of therapeutic massage demonstrated statistically significant reductions in cardiovascular parameters after a 3-day intervention of slow-stroke back massage on individuals in a rehabilitation setting.67 Twenty-four adults (age range 52 to 88 years) underwent daily intervention. Statistically significant decreases in systolic and diastolic BP were noted each day; this was true for heart rate (HR) and respiratory rate (RR) only on days 1 and 3. Subjects also reported improved perception and less anxiety.
Cottingham and colleagues (1988b)68 investigated the effects of the Rolf method of soft tissue mobilization on parasympathetic nervous system (PNS) tone in 32 young, healthy men. This RCT compared a group that performed 45 minutes of Rolfing with pelvic mobilization (pelvic lift) with a control group that received a 45-minute durational touch without Rolfing (pelvic lift intervention). At baseline all subjects had an anterior pelvic tilt. PNS tone was measured before, immediately after, and 24 hours after intervention. Results demonstrated a significant increase in PNS tone and decreased standing pelvic tilt angle in the intervention group. Earlier, Cottingham and colleagues (1988a)69 demonstrated an increase in PNS tone with the pelvic lift technique unrelated to the durational touch used simultaneously in the technique. The authors concluded that this intervention of soft tissue pelvic manipulation (i.e., durational touch plus pelvic lift) can help individuals with muscle dysfunction and conditions associated with reduced PNS activity and increased sympathetic nervous system activity. Reduced PNS and increased SNS can be representative of deconditioning.
In a small study of 12 children and adults, investigators attempted to examine the reliability of craniosacral intervention interpretation among three expert practitioners of craniosacral therapy.70 They also investigated the relationship of the craniosacral rate to HR and BP of subject and practitioner. Results demonstrated no interrater reliability among the three practitioners. Results also demonstrated no relationship between HR and BP and the craniosacral rates. Although this study did not attempt to report on the effects of craniosacral therapy on cardiovascular parameters, the results do shed light on potential considerations for future study design.
Green and colleagues (2004)71 conducted a rigorous review of the evidence for using craniosacral therapy. Nine of the 34 studies reviewed looked at whether movement of cranial bones was possible, and 10 of the 34 studies looked at whether cerebrospinal fluid moves rhythmically. The authors concluded that evidence supports the belief that there is a cranial “pulse” or rhythm that is separate from the cardiac or respiratory rhythms.
Energy Work Interventions
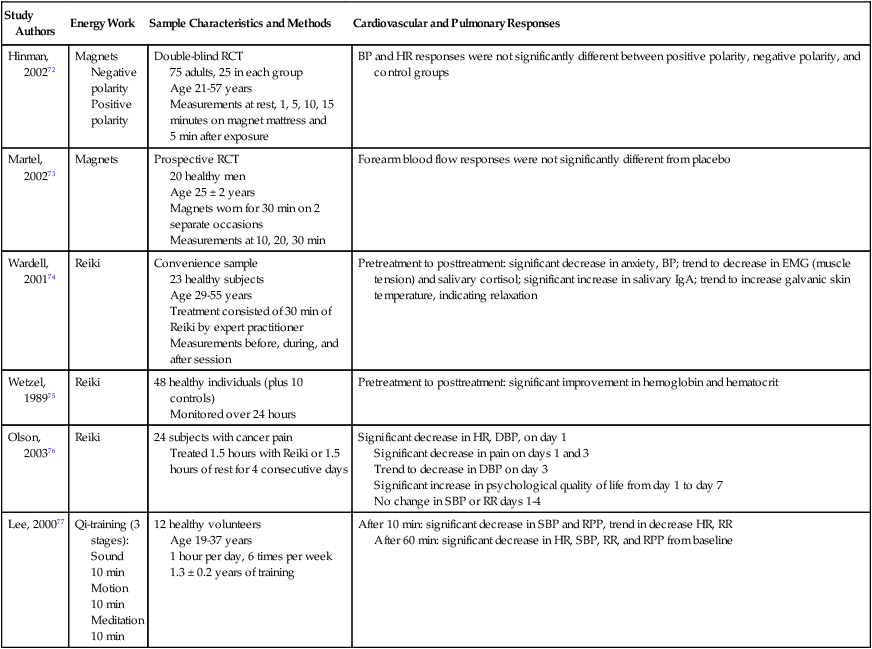
A few studies addressing the cardiovascular and pulmonary responses to energy work in healthy subjects have been conducted. Some of these are summarized in Table 27-3. In most cases, methodological weaknesses limit generalizations about the results. Studies of Reiki demonstrate trends toward increased relaxation and improved immune system markers.74–76 In a study of qi-training, the authors provide a detailed description of the intervention facilitating replication of the study with a larger sample.77 The two studies investigating responses to magnets demonstrate no significant differences from control.72,73 Of interest, in a study investigating the safety of prosthetic mini-magnets in individuals with cardiac pacemakers, the authors found no electrocardiographic changes in 9 of 12 subjects. When the magnets were moved at least 1 cm away from the pacemaker implant, the changes in the other 3 subjects no longer existed.78
Table 27-3
Cardiovascular and Pulmonary Responses to Energy Work in Healthy Individuals
| Study Authors | Energy Work | Sample Characteristics and Methods | Cardiovascular and Pulmonary Responses |
| Hinman, 200272 | Magnets Negative polarity Positive polarity |
Double-blind RCT 75 adults, 25 in each group Age 21-57 years Measurements at rest, 1, 5, 10, 15 minutes on magnet mattress and 5 min after exposure |
BP and HR responses were not significantly different between positive polarity, negative polarity, and control groups |
| Martel, 200273 | Magnets | Prospective RCT 20 healthy men Age 25 ± 2 years Magnets worn for 30 min on 2 separate occasions Measurements at 10, 20, 30 min |
Forearm blood flow responses were not significantly different from placebo |
| Wardell, 200174 | Reiki | Convenience sample 23 healthy subjects Age 29-55 years Treatment consisted of 30 min of Reiki by expert practitioner Measurements before, during, and after session |
Pretreatment to posttreatment: significant decrease in anxiety, BP; trend to decrease in EMG (muscle tension) and salivary cortisol; significant increase in salivary IgA; trend to increase galvanic skin temperature, indicating relaxation |
| Wetzel, 198975 | Reiki | 48 healthy individuals (plus 10 controls) Monitored over 24 hours |
Pretreatment to posttreatment: significant improvement in hemoglobin and hematocrit |
| Olson, 200376 | Reiki | 24 subjects with cancer pain Treated 1.5 hours with Reiki or 1.5 hours of rest for 4 consecutive days |
Significant decrease in HR, DBP, on day 1 Significant decrease in pain on days 1 and 3 Trend to decrease in DBP on day 3 Significant increase in psychological quality of life from day 1 to day 7 No change in SBP or RR days 1-4 |
| Lee, 200077 | Qi-training (3 stages): Sound 10 min Motion 10 min Meditation 10 min |
12 healthy volunteers Age 19-37 years 1 hour per day, 6 times per week 1.3 ± 0.2 years of training |
After 10 min: significant decrease in SBP and RPP, trend in decrease HR, RR After 60 min: significant decrease in HR, SBP, RR, and RPP from baseline |
RCT, Randomized control trial; DBP, diastolic BP; SBP, systolic BP; RPP, rate-pressure product.
In a well-written and well-designed paper, investigators reported on the effects of acupuncture on autonomic nervous system (ANS) function.79 Twelve healthy volunteers, six men and six women, ages 23 to 48 years, underwent randomized needle insertion into three distinct acupuncture sites. Measures of ANS function were monitored during the 25-minute intervention period and for the 60 minutes after intervention at each insertion site. An interesting combination of results was found, depending on the needle insertion site. Stimulation of the ear site resulted in increased PNS activity during both the needle insertion and the poststimulation periods. Stimulation of the skin over the left thenar muscle resulted in increased sympathetic nervous system (SNS) and PNS activity during both measurement periods. Stimulation of the right thenar muscle resulted in an increase in SNS and PNS activity during the poststimulation period, but no changes were seen during the needle insertion period. These results begin to shed light on which acupuncture interventions may be cardiosuppressive and possibly account for the calmness and relaxation often reported after treatment. Delayed responses may have a therapeutic effect as well.
In a controversial study by Rosa and colleagues (1998),80 the investigators failed to demonstrate that those practitioners of noncontact therapeutic touch were able to perceive a “human energy field.” Significant limitations to the study have been noted, including experimenter bias, inconsistent conclusions, and incomplete statistical analysis.81 Although this study does not address cardiovascular and pulmonary responses to therapeutic touch, it does provoke discussion about the difficulties of conducting research on this intervention.
A study by Haas and colleagues (1986)82 is worthy of mention in this discussion of energy interventions. These authors were able to demonstrate the ability of musical rhythm to “pace” respirations. In a sample of 20 healthy volunteers (half of whom were musically trained), breathing rhythms were correlated with metronome and tapping rhythms. This ability of musical rhythms to entrain respiration may have potential benefits in managing stress-induced respiratory patterns.
Risk Factors for Coronary Artery Disease
Numerous complementary therapies have been studied and shown efficacious in the management of known risk factors for coronary artery disease (CAD).83–85 Specifically, interventions addressing psychological stress and hypertension have been extensively examined.
Stress Reduction
First studied in the late 1970s and early 1980s, the benefits of meditation and the “relaxation response” have been recognized by Benson and colleagues (1977).86 They postulated that when properly applied, these interventions facilitated downregulation of the SNS and upregulation of the PNS.
During 15 to 30 minutes of practicing the relaxation response, changes in cardiovascular and pulmonary parameters have been noted. These include a decrease in RR and oxygen consumption ( ) and an increase in cardiac output (CO) without a concurrent increase in BP, reflecting a reduction in peripheral vascular resistance. In addition, skilled practitioners of the relaxation response demonstrate a decrease in
) and an increase in cardiac output (CO) without a concurrent increase in BP, reflecting a reduction in peripheral vascular resistance. In addition, skilled practitioners of the relaxation response demonstrate a decrease in  at a constant workload during treadmill activity.87
at a constant workload during treadmill activity.87
In an important paper addressing the impact of psychological factors on the development of cardiovascular disease, researchers related CAD to depression, anxiety, personality factors and character traits, social isolation, and chronic life stress.88 Several authors have addressed behavioral interventions effective in the management of these psychosocial stresses.
In a comprehensive metaanalysis of 70 articles, the treatment of trait anxiety with transcendental meditation (TM), progressive relaxation, relaxation response, and electromyographic (EMG) biofeedback were reviewed. Sources for the reviewed articles included journals, dissertations, and books. All interventions had a positive effect on self-reports or physiological measures of anxiety. Transcendental meditation had the strongest effect of the four interventions studied. In general, subjects who received more frequent interventions initially and who were followed the longest received the most benefit. It was recommended that future studies measure performance outcomes and that subjects be closely followed in an attempt to reduce loss due to attrition.89
Miller and colleagues (1995)90 reported on 22 subjects with anxiety disorders who participated in a noncontrolled clinical trial. Subjects were trained in mindfulness meditation, participated in a once-a-week group program for 8 weeks, and were followed-up for 3 years. Significant reductions in medications and counseling requirements were noted. The authors concluded that “mindfulness training … may be able to provide medical patients suffering from anxiety with a set of tools for achieving effective long-term non-pharmacological self-regulation … and be used as a complement to more conventional medical interventions.”90 Conversely, Astin (2003)30 reported an increase in anxiety levels in 17% to 31% of subjects practicing relaxation interventions and an increase in anxiety levels in up to 53.8% of subjects practicing TM. No negative medical consequences were reported as a result of the increased anxiety levels. Several causes for this negative response were postulated, including subjects’ fear of losing control, general restlessness, intrusive thoughts, and feelings of vulnerability.
Several small, noncontrolled clinical studies examining the effects of TM on blood levels related to cardiovascular disease have been reported. Infante and colleagues (2001)91 measured plasma catecholamine levels (epinephrine, norepinephrine, and dopamine) in 19 skilled practitioners of TM. Resting values were compared with catecholamine levels in nonmatched controls. Results demonstrated lower values in the skilled practitioners when compared with the controls. The authors concluded TM may have been responsible for the lower catecholamine levels and consequent downregulation of the SNS. Similarly, Schneider and colleagues (1998)92 concluded that TM may have been responsible for lower serum lipid peroxide levels found in 18 practitioners of TM compared with higher levels found in 23 nonmatched, nonpracticing control subjects. Lipid peroxide has been implicated in the pathophysiology of atherosclerosis.
Cognitive approaches to the reduction of stress have been subjected to clinical study. McCrone and colleagues (2001)93 compared the effectiveness of psychoeducational interventions on 33 male subjects with risk factors for CAD. In addition to nutrition counseling and exercise training, educational sessions addressing cardiovascular disease, risk factors, and stress reduction were offered to 25 participants. These subjects were also trained to use specific skills to improve their responses to stress and were given audiotapes to practice progressive muscle relaxation. Eight subjects in the nonrandomized control group received weight management counseling and health education only and did not participate in any discussions related to stress management. All subjects, ranging in age from 57 to 79 years, participated in the interventions for 6 months. Although both groups showed improvements in risk factor profiles, improvement was greater in the group trained in stress management interventions. Significant improvements were noted in BP, lipid profile, obesity indices, and fitness level.
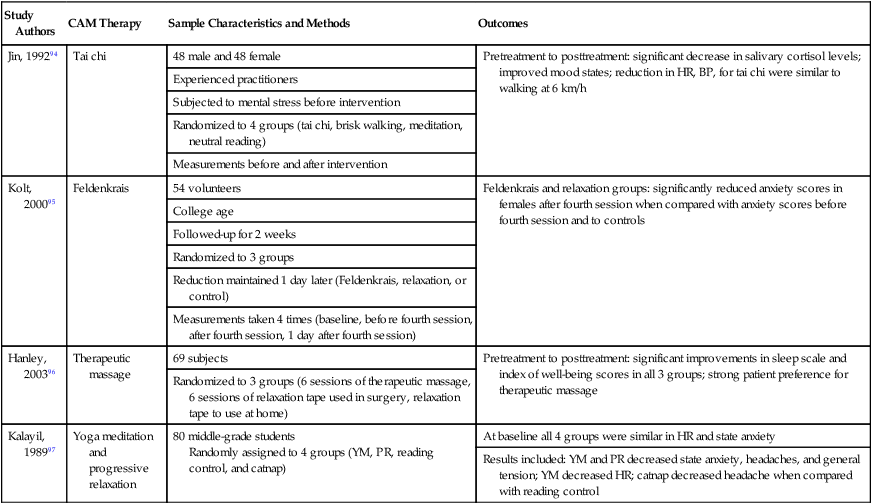
In spite of a positive theoretical basis for the use of CAM therapies in stress management, many interventions have not been subjected to systematic investigation. Table 27-4 summarizes the effects of tai chi, Feldenkrais method, yoga, and therapeutic massage in stress management. Although these four studies have significant methodological weaknesses, the number of subjects participating in each study is formidable. These initial attempts at providing efficacy of the respective intervention help suggest a launching ground for future study.
Table 27-4
Effect of Selected CAM Therapies in Stress Management in Healthy Individuals
| Study Authors | CAM Therapy | Sample Characteristics and Methods | Outcomes |
| Jin, 199294 | Tai chi | 48 male and 48 female | Pretreatment to posttreatment: significant decrease in salivary cortisol levels; improved mood states; reduction in HR, BP, for tai chi were similar to walking at 6 km/h |
| Experienced practitioners | |||
| Subjected to mental stress before intervention | |||
| Randomized to 4 groups (tai chi, brisk walking, meditation, neutral reading) | |||
| Measurements before and after intervention | |||
| Kolt, 200095 | Feldenkrais | 54 volunteers | Feldenkrais and relaxation groups: significantly reduced anxiety scores in females after fourth session when compared with anxiety scores before fourth session and to controls |
| College age | |||
| Followed-up for 2 weeks | |||
| Randomized to 3 groups | |||
| Reduction maintained 1 day later (Feldenkrais, relaxation, or control) | |||
| Measurements taken 4 times (baseline, before fourth session, after fourth session, 1 day after fourth session) | |||
| Hanley, 200396 | Therapeutic massage | 69 subjects | Pretreatment to posttreatment: significant improvements in sleep scale and index of well-being scores in all 3 groups; strong patient preference for therapeutic massage |
| Randomized to 3 groups (6 sessions of therapeutic massage, 6 sessions of relaxation tape used in surgery, relaxation tape to use at home) | |||
| Kalayil, 198997 | Yoga meditation and progressive relaxation | 80 middle-grade students Randomly assigned to 4 groups (YM, PR, reading control, and catnap) |
At baseline all 4 groups were similar in HR and state anxiety |
| Results included: YM and PR decreased state anxiety, headaches, and general tension; YM decreased HR; catnap decreased headache when compared with reading control |
Hypertension
There is a significant body of literature that addresses the benefits of CAM interventions in the management of hypertension (HTN). The majority of the larger studies address mind/body interventions, with most demonstrating positive effects on BP. In 1999 the Canadian Hypertension Society and the Heart and Stroke Foundation of Canada published guidelines recommending “individualized cognitive behavior modification to reduce the negative effects of stress.”98
Eisenberg and colleagues (1993)99 performed a metaanalysis addressing the effectiveness of cognitive behavioral therapies on HTN. Interventions accepted in this review were biofeedback, meditation, the relaxation response, progressive relaxation techniques, and stress management interventions such as imagery. They collected more than 800 published papers; however, because of methodological problems in the majority of papers, their limited inclusion criteria of adult subjects with diastolic BP of 90 to 114 mm Hg, lack of randomized control design, weak description of the study, and poor reporting of BP values, only 26 studies were entered for detail review. Results of this comprehensive analysis of 1264 patients indicated superior outcomes in the group receiving cognitive intervention techniques when compared with controls. No one intervention demonstrated more favorable outcomes than any other. In addition, when control groups were subjected to a placebo intervention (i.e., sham biofeedback), no significant differences in outcomes were noted. This is consistent with the belief that an intervention effect is inherent in the concept of placebo.31
In two RCTs of African American subjects, investigators examined the effects of stress reduction approaches on HTN. In one study, 111 males and females with mean BP of 147/92 mm Hg and mean age of 67 years were randomized to a 3-month trial of TM and progressive muscle relaxation (PMR) or a lifestyle modification education control program.100 Results demonstrated that TM had a greater effect at lowering both systolic and diastolic BP than did PMR and that both intervention groups demonstrated a significantly greater impact on BP reduction than did the control group. In a small but well-designed study, Barnes and colleagues (2001)101 recruited 34 African American adolescents (ages 15 to 18 years) with high-normal BP (>85th and <95th percentile for age and sex, respectively. After randomization, 17 subjects participated in 2 months of daily, 15-minutes sessions of TM. The control group attended seven weekly, 1-hour lessons on health education. Measures of cardiovascular function were collected at rest and during performance of a stressful activity (at baseline and again at the end of the intervention period). Although no significant changes were noted in resting values, results indicated that individuals in the TM group responded more favorably to stressor activities. Blood pressure increased appropriately during the activity in both groups; however, the degree of elevation was reduced in the TM group when compared with controls.
Reduction in antihypertensive medication requirements has been reported when mind/body therapies are added to the management regimen of HTN. In an RCT, Shapiro and colleagues (1997)102 studied 39 individuals with medically treated HTN. Subjects trained in cognitive behavior therapies (i.e. PMR, biofeedback, deep diaphragmatic breathing, and imagery) showed a 73% reduction of BP medication requirements during the study follow-up period compared with a 35% reduction in the control group. In addition, 55% of subjects in the intervention group were completely free of medication compared with only 30% of subjects in the control group. The reduction in BP levels was consistent across clinical, ambulatory, and home settings.
Yucha and colleagues (2004)103 reviewed 20 RCTs investigating the effects of biofeedback on HTN. Several forms of biofeedback, including thermal, EMG, and electrodermal, resulted in reductions in blood pressure when the intervention was combined with related cognitive therapy and relaxation training. When biofeedback was the sole intervention, significant reductions in BP were not demonstrated. Wang and colleagues (2004)104 performed a systematic review of the effects of tai chi on chronic conditions, including HTN. They reported on four moderate-sized studies: two randomized controlled trials and two nonrandomized controlled trials. Outcomes of all four studies indicated significant reduction in BP in older individuals and in those recovering from acute MI.
In addition to the mind/body therapies discussed above, several additional studies investigating the effects of select CAM therapies in individuals with HTN are summarized in Table 27-5. Although the evidence presented in these studies is weak, these investigations provide valuable insights to consider when structuring future research protocols. Several review articles addressing effects of other interventions are summarized in Table 27-6. In general, the results of these investigations assist in providing evidence for the benefit of the intervention in the management of HTN. In one review, Levin and Vanderpool (1989)110 consider the beneficial effects of religious commitment and affiliation in the management of HTN. Possible explanations offered for lower blood pressure in individuals with HTN include the psychosocial effects of membership in an organized religious community, the inherent health promotion behaviors and preferences often supported by religious traditions, and the psychodynamics of religious rites, faith, and belief systems.
Table 27-5
Effect of Selected CAM Therapies in the Management of HTN
| Study Authors | CAM Therapy | Sample Characteristics and Methods | Outcomes |
| Paran, 1996105 | Biofeedback | 38 patients (15 white-coat HTN; 23 essential HTN) Random assignment Biofeedback given 1 time per week for 4 weeks |
Pretreatment to posttreatment: both groups had statistically significant reductions in BP in the clinic; white-coat HTN had significantly lower SBP and DBP at home than essential HTN |
| Patel, 1975106 | Yoga (and biofeedback), “psychophysical relaxation exercise” | 40 patients with HTN Followed-up for 9-12 months 20 received intervention; 20 remained as controls |
Statistically significant reductions in BP and anti-HTN medication requirements in intervention group |
| Brownstein, 1989107 | Yoga relaxation | Case report Age 46 years Male History of mild essential HTN 6-week program |
Discontinuation of anti-HTN medications; normalization of DBP; return to full flight status (aviator in U.S. Air Force) |
| Zucker, 1997108 | Qi gong (breathing, meditation, movement) | 22 patients with HTN (15 in intervention group, 7 control) Intervention classes 2 times per week for 8 weeks |
Pretreatment to posttreatment: significant decreases in SBP, DBP, MAP, RR in intervention group; significant increases in QOL in intervention group |
| McCraty 2003109 | Stress reduction (Inner Quality Management) Biofeedback |
32 information technology employees with HTN Mean age 46, 9 females; Intervention (I): three sessions totaling 16 hours over 2 weeks followed by home program with optional review session at 2 months and follow-up measures at 3 months |
Both control (C) and I reduced BP; reduction in I was significantly greater than C; 3 in I were able to reduce or terminate BP medications Compared with C, I showed significant increase in well-being and work satisfaction, and decrease in stress symptoms, depression, phobic anxiety Reduced BP was correlated with reduced stress symptoms |
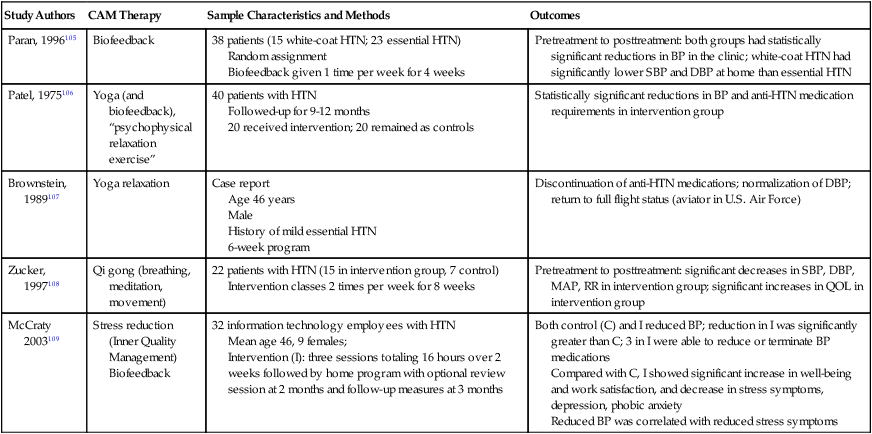
Table 27-6
Select CAM Therapies and their Effects on HTN: Summary of Review Papers
| Study Authors | CAM Therapy | Number of Articles Reviewed | Outcome Variables | Outcome |
| Levin, 1989110 | Religion*: RC, RA | 20 | SBP, DPB, HTN, heart disease mortality, HTN-related mortality, history of HTN | RC: 19 studies demonstrate intervention is associated with lower BP or lower rates of HTN; 5 studies demonstrate protective effects of intervention RA: significantly lower rates of HTN-related morbidity and mortality in highly devout, behaviorally strict groups (e.g., Mormons, Buddhists, Seventh-Day Adventists, clergy) |
| Sancier, 1999111; Mayer, 1999112 | Qi gong | 30 | BP, measures of blood flow, CHF, acute MI, stroke, total mortality rate | Decreased stroke and mortality; decreased anti-HTN medication requirements |
| Yeh 2008113 | Tai chi | 8 | SBP, DBP, compliance, medications | Tai chi groups demonstrated significant reductions in BP, higher compliance with home program, and more effective BP control |
| Lee 2010114 | Tai chi, >60 years old |
4 | BP | Two reviews reported significant reduction in BP in tai chi group when compared with control or wellness education program Two reviews reported no reduction in BP compared with resistance training, usual activity or aerobic exercise |
| Kim 2010115 | Acupuncture, traditional meridian needle insertion points | 20 | BP | Significant reductions in BP in both high- and low-quality studies; duration of reduction in BP was variable amongst studies; magnitude of BP reduction was greater when acupuncture, rather than sham treatment, was used in conjunction with anti-HTN medications |
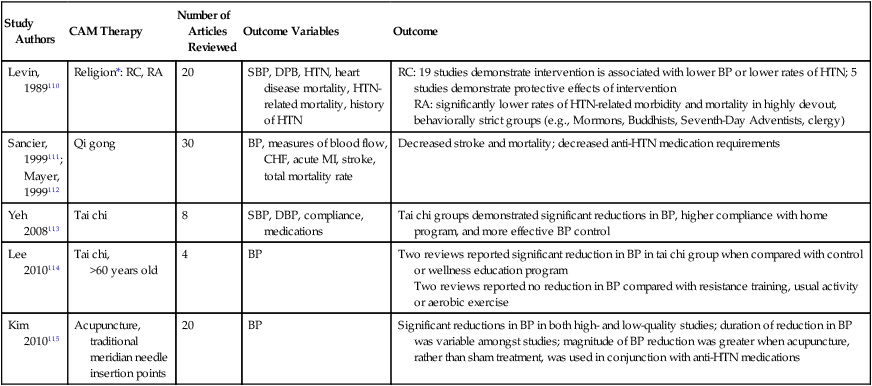
RC, Religious commitment; RA, religious affiliation.
*Measures of religion include religious attendance, church membership, religious affiliation, ethnic traditions within Judaism, monastic orders, clergy status, religious education, and subjective religiosity.
In the review articles of the effects of qi gong in HTN, authors acknowledge significant methodological weaknesses in many of the studies reviewed.111,112 Some of the reported weaknesses include selection biases, lack of randomization, noncompliance with the intervention, concerns regarding BP measurement reliability, and the differences among the many styles of qi gong, which were not typically considered. Two review articles on the effects of tai chi on HTN are included in Table 27-6. Significant improvement in BP was reported in the eight studies reviewed by Yeh and colleagues (2008).113 Lee and colleagues (2010)114 found conflicting results in their review; they attributed their inconsistent outcomes to inadequate baseline BP testing in all four of the studies reviewed (one study was common to both of these reviews). Finally, Kim and colleagues (2010)115 presented a thorough review of 20 articles on the effects of acupuncture on HTN. They acknowledged that 17 of the 20 studies were poor quality and concluded that further “rigorously designed studies” are needed.115 Of note, no significant adverse reactions were documented in any of the tai chi or acupuncture articles reviewed.
Cardiovascular Conditions
Much of the pathophysiological basis for applying CAM therapies to cardiovascular conditions rests in the relationship between the cardiovascular system and the ANS.116 Stimulation of the ANS, specifically the SNS, can cause both an increase in circulating levels of catecholamines and damage to endothelial cells lining arterial walls. Often triggered by psychological factors, the resulting increase in metabolic and myocardial oxygen demand has a negative impact on the oxygen transport system.88 Interventions that can reduce or reverse these responses to SNS stimulation have a potential positive effect on cardiovascular conditions. Recently, a number of authors have looked at the impact of various CAM interventions on heart rate variability (HRV).117–121 The variability in R-R intervals between normal sinus rhythm cardiac cycles reflects the balance of SNS and PNS cardiac control. Low HRV has been associated with disease, whereas high HRV tends to indicate cardiovascular health and improved prognosis. In addition, patterns of HRV appear to reflect alterations in emotions and have been used to further demonstrate cardiovascular physiological responses to CAM interventions.122
Coronary Artery Disease
Beneficial effects of CAM interventions in the use of CAD management are documented throughout the published literature.29,30,32,123–125 Although significant methodological problems are apparent in many papers, numerous large, well-designed studies can be found. Much of the evidence supporting the use of these interventions in individuals with CAD demonstrates improvement in exercise tolerance, reduction of ischemia, and reduction of anxiety and depression. Mind/body techniques, including cognitive behavioral interventions, yoga, tai chi, guided imagery, and music therapy, have been successfully used in patients with CAD. The benefits of energy work, including distant healing prayer and qi gong, in patients with CAD have been reported.
In 1959, Friedman and Rosenman126 first documented the relationship between certain emotional behaviors and the prevalence of CAD.127 They defined the type A behavior pattern as “an emotional syndrome characterized by a continuously harrying sense of time urgency and easily aroused free-floating hostility.”127 In subsequent decades, the study of interventions aimed at modifying the behavior of individuals with type A behavior pattern and CAD was undertaken.
In a large study of post-myocardial infarction (MI) patients with type A behavior, 1013 subjects were randomized into three groups.127 Of the total, 270 subjects received group cardiac counseling, 592 subjects received both cardiac counseling and type A behavioral counseling, and the remaining 151 individuals did not receive any counseling. Subjects were followed for  years to determine the impact of type A behavior counseling on recurrent coronary events (both nonfatal infarctions and cardiac deaths). Cardiac counseling sessions consisted of 90-minute group meetings during which diet, exercise, medications, cardiovascular pathophysiology, and possible surgical procedures were discussed. Type A behavioral counseling sessions included progressive muscle relaxation, as well as specific psychotherapeutic interventions. Results indicated statistically significant reductions in recurrence rates of cardiac events in both intervention groups, with a greater reduction in the rate of recurrent events in those subjects who received both forms of counseling.
years to determine the impact of type A behavior counseling on recurrent coronary events (both nonfatal infarctions and cardiac deaths). Cardiac counseling sessions consisted of 90-minute group meetings during which diet, exercise, medications, cardiovascular pathophysiology, and possible surgical procedures were discussed. Type A behavioral counseling sessions included progressive muscle relaxation, as well as specific psychotherapeutic interventions. Results indicated statistically significant reductions in recurrence rates of cardiac events in both intervention groups, with a greater reduction in the rate of recurrent events in those subjects who received both forms of counseling.
In a landmark study of 48 patients with known CAD, Ornish and colleagues (1990)11 analyzed the number of coronary artery lesions detected at angiography before and after a year-long lifestyle intervention. In addition to a low-fat vegetarian diet, smoking cessation, and a moderate exercise program, subjects participated in a stress management training program of guided imagery. At the end of the year, the 28 subjects in the intervention group demonstrated statistically significant fewer coronary lesions than the 20 subjects in the usual-care control group. The regression in coronary atherosclerosis was attributed to the comprehensive lifestyle changes, brought about without the assistance of lipid-lowering medications. Clinical reports of angina were reduced as well.
Upon recognition of the impact of emotions on the recurrence rate of cardiac events in individuals with CAD, behavioral interventions became routine therapies in cardiac care.33 Dusseldorp and colleagues (1999)128 published a metaanalysis of the results of 37 studies investigating the effects of psychoeducational programs on patients with known CAD. All studies were conducted between 1974 and 1997 and were categorized according to stress management (SM) and health education (HE) interventions. Interventions used included various combinations of education, cognitive-behavioral therapies, relaxation, imaging, and emotional support. A number of studies included SM and HE interventions in combination with standard exercise training programs typically found in traditional cardiac rehabilitation programs. Results from studies administering either SM or HE intervention suggested a 34% reduction in fatal cardiac events and a 29% reduction in recurrent MI. The authors concluded that although psychoeducational therapies should be encouraged in cardiac rehabilitation programs, future research focusing on specific SM or HE interventions is warranted. In another metaanalysis addressing the effects of psychosocial interventions in subjects with CAD, Linden and colleagues (1996)129 reviewed 23 studies of 2024 patients and 1156 control subjects. In addition to the typical education component of cardiac rehabilitation programs, almost half of the studies included in this analysis involved some form of CAM treatment as an intervention. These included relaxation, breathing relaxation, and music therapy. Just as in the aforementioned metaanalysis, the benefits of adding a psychosocial component to these cardiac rehabilitation programs significantly reduced morbidity and mortality and psychological distress.
In 2000, in a scientific statement presented by the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation, psychosocial management was identified as a “core component of cardiac rehabilitation/secondary prevention programs.”130 Suggested interventions included “individual and/or small group education and counseling regarding adjustment to coronary heart disease, stress management, and health-related lifestyle change … supportive rehabilitation environment and community resources to enhance patient’s and family’s level of social support.”130
The relationship between mental stress and myocardial ischemia in men with CAD has been well studied. Investigators have found an increased likelihood of having mental–stress-induced ischemia in individuals who experience daily life ischemia.131 Individuals with chronic anxiety and depression also exhibit more episodes of myocardial ischemia than those without documented anxiety and depression.132 In a 5-year, nonrandomized controlled study of 94 men with documented mental–stress-induced ischemia, researchers reported on the usefulness of a stress management program.133,134 In addition to educational classes, the intervention group received instruction aimed at reducing the physiological effects of stress. This included instruction in progressive muscle relaxation and individual sessions of EMG biofeedback. Outcomes of recurrent cardiac events were significantly reduced in the stress management group when compared with the control group at 1-, 2-, and 5-year follow-up. Overall reductions in hostility and clinical depression were also reported as statistically and clinically significant. The 5-year financial burden, including hospitalization and physician costs, was also significantly less in the stress management group. Similar results were reported by Zamarra and colleagues (1996)135 in a small, nonrandomized controlled study of the effects of an 8-month trial of TM. At follow-up bicycle exercise testing, participants demonstrated increases in exercise duration and maximal workload achieved and a delay in the onset of ST depression. In an early paper, Benson and colleagues (1975)136 reported on the beneficial effects of the relaxation response in reducing the number of premature ventricular contractions (PVC) in individuals with stable CAD. Subjects in this report practiced the relaxation response for 20 minutes, twice a day. Frequency of PVCs was documented by Holter monitor at baseline and again after 4 weeks.
In a thorough review Villagomeza (2006)137 explored the impact of spirituality in patients with heart disease. Twenty-six studies were discussed and included patients with acute MI, coronary artery bypass graft surgery, congestive heart failure, and heart transplant. Definitions of spirituality were listed for all articles reviewed. Most studies were descriptive or observational, and most measurement instruments were interview- and questionnaire-based; several studies used physiological and performance-based measurements. The author did not focus any conclusions on the effects of “spirituality” on heart disease but rather addressed a framework from which spirituality could be more easily studied. Irrespective of the definition of spirituality used in the 26 reviewed papers, the impact on outcomes appeared favorable.
Several studies have demonstrated no or limited improvements in cardiovascular outcomes with the intervention of specific behavioral therapies. In a large (n = 2328) RCT of early post-MI intervention, investigators reported limited benefit of psychological counseling.138 In this 2-year follow-up study, patients with acute MI returned within 28 days of the acute event to participate in 7 weeks of outpatient counseling, including PMR and skills to reduce stress. Subjects in the intervention group experienced significantly fewer episodes of angina; however, mortality, clinical complications, and clinical sequelae of CAD did not differ between groups. The authors concluded that the intervention was conducted too soon after the cardiac event, possibly accounting for the reduced treatment effect. In a study of patients participating in a phase II cardiac rehabilitation program, progressive muscle relaxation and guided imagery interventions failed to result in beneficial outcomes.139 Although there were methodological limitations in this paper, the authors similarly concluded the timing of the interventions may have contributed to the absence of benefit.
Results of the effects of selected mind/body therapies in CAD are summarized in Table 27-7. Manchanda and colleagues (2000)140 investigated the effects of yoga on numerous cardiovascular measures. Although improved outcomes were documented in the intervention group when compared with controls, the demonstrated benefits may be due to the moderate exercise component of the intervention and not necessarily the yoga component.
Table 27-7
Effect of Selected Mind/Body Therapies in CAD
| Study Authors | MBT Therapy | Sample Characteristics and Methods | Outcomes |
| Manchanda, 2000140 | Yoga | Prospective RCCT 42 men with CAD 2 groups Intervention: yoga, RF control, diet control, moderate exercise Control: RF control, AHA step 1 diet control |
Yoga group: (compared with controls) significant decrease in number of anginal episodes per week; improved exercise capacity; decreased body weight, total cholesterol, LDL cholesterol, triglycerides; fewer revascularization procedures; more lesion regression and less lesion progression (angiographic findings); improved functional class, symptomatic status, and RF profile |
| Friedlander, 1986141 | Religion (Orthodox Jewish) |
Had first MI: 454 men (51% secular) 85 women (50% secular) Healthy, no CAD: 295 men (21% secular) 391 women (16% secular) |
Higher risk for first MI if: older, smoker, less education; European born; secular, men and women; results persisted 2-3 months after acute event |
| Strawbridge, 1997142 | Religion | 5286 survey respondents Followed-up for 28 years Analyzed for association between attendance at religious services and mortality |
Frequent attenders compared with infrequent attenders: lower mortality rates; results were stronger for females; improved health practices (stop smoking, increase exercising, increase social contacts, stay married) |
| Chang, 2010143 | Tai Chi | 54 patients with CAD; 22 did 90 min tai chi 1x/week for 6 months 32 patients usual care Modified Bruce TM at baseline and 6 months |
Improved RPP and RPP reserve in tai chi group compared with usual care |
| Park, 2010144 | Tai Chi | 85 adults with CAD (50 males); 53-75 years (mean 66 years); measures at baseline and 6 months 33 received tai chi (1x/week for 60 min) and education nutrition (1 hr /month) stress management (1 hr/month) 19 received tai chi only 33 received usual care |
Tai chi is safe for population Tai chi with education significantly improved cardiovascular risk factors (BP, lipids), QOL, BMI when compared with tai chi–only group |
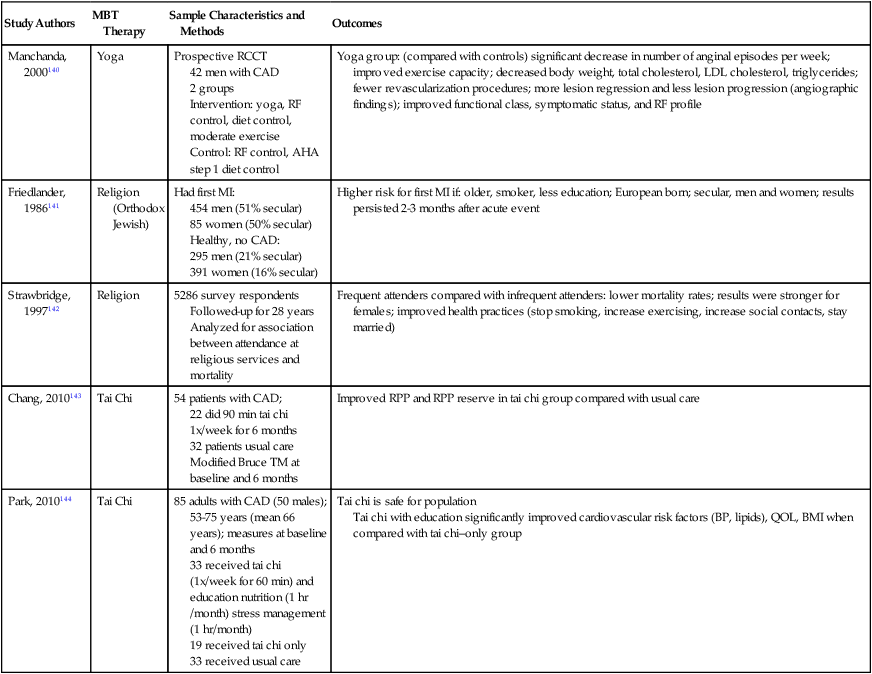
Tai chi practice has been recommended as a therapeutic intervention in balance disorders and fall prevention in older adults.25,145,146 Its potential benefits as replacement for or as an adjunct therapy in cardiac rehabilitation programs have been suggested as well.143,144,147 In an interesting commentary in 1992, Ng stated that tai chi “has many similarities with … walking exercise—the most recommended aerobic exercise for coronary artery disease.”148 Further clinical study is warranted to provide evidence of the benefit of tai chi in the population with CAD.
Two papers addressed the use of several mind/body and manual therapies to assist with anxiety reduction in patients undergoing cardiac catheterization. McCaffrey and colleagues (2005)149 reported on the use of music therapy, massage, guided imagery, and therapeutic touch. These interventions were performed within the hour before the diagnostic procedure. Outcomes demonstrated reduction in BP, HR, and worry, along with improved mood, in the intervention group when compared with the control group. In another study, using a visual analogue scale, authors demonstrated that “PalmTherapy” was effective in reducing anxiety levels before the procedure. PalmTherapy is an intervention that uses continuous pressure on various points in the hand.150
There is minimal evidence available investigating the effects of energy work on patients with CAD. Several studies compared acupuncture to sham acupuncture in individuals with angina.151 Although no significant differences were noted in the number of anginal episodes or nitroglycerin use, the use of sham acupuncture has been questioned. As noted earlier, not all practitioners agree on proper needle location; hence what one practitioner thinks is an active acupuncture site may be considered a sham site to another practitioner. An interesting review of the effects of acupuncture on cardiac dysrhythmias was recently published.152 The authors considered the ineffectiveness of antiarrhythmic drugs in managing certain dysrhythmias and aimed to examine the impact of acupuncture on reducing these abnormal cardiac rhythms. They reported on eight studies; seven were case studies or case series, and one was a randomized controlled trial. A total of 150 subjects participated in the eight studies, and the mean age was 54 years. Male and female participants were included, and dysrhythmias, although diverse, were primarily supraventricular tachycardia, sinus bradycardia, and ventricular extrasystoles. All participants received antiarrhythmic medications in addition to acupuncture. Treatments ranged between 1 day and 6 months, and between 1 and 50 sessions; each session lasted an average of 20 minutes. The primary outcome measured in all studies was the frequency of dysrhythmia presentation or conversion to normal sinus rhythm. Between 87% and 100% of participants demonstrated improvement; no dropouts or adverse effects were reported. There were significant methodological weaknesses in many of the studies, which led the authors to conclude that future large, rigorous trials are warranted.
Another role for CAM therapies that address stress reduction in patients with CAD is based on the relationship between chronic stress and reduced immune system function. Individuals with depressed immune systems are more vulnerable to inflammatory processes, the latter recently implicated in CAD.153–155
Cardiac Surgery
The Complementary Care Center (CCC) at Columbia-Presbyterian Medical Center is a “multifaceted program dedicated to evaluating and researching the effects of new modalities in health care.”156 Since 1995, practitioners at this center have been evaluating and researching the effects of various types of CAM therapies. One area of intervention involves patients having cardiac surgery. Upon initial evaluation, these patients are offered several options to help with recovery and healing. Some of these modalities include meditation, music therapy, yoga, massage, and therapeutic touch. Audiotapes can be used at various times in the perioperative period, including 5 to 10 days preoperatively, intraoperatively, immediately postoperatively, and during the recuperation phase. Therapeutic touch has been offered on the day of surgery and on postoperative days 2 and 3. Group yoga classes are offered to those patients who are medically stable as early as the third postoperative day. In addition, patients are encouraged to contact a religious leader of their choice. Continuation of these therapies is offered to the patient after hospital discharge. Patients can choose to attend sessions at the center or at a more convenient site.
The innovative approach used at the CCC resonates with the philosophy of increasing the patient’s participation in his or her health and healing. Liu and colleagues (2000)157 have reported on the use of CAM therapies in 376 consecutive patients undergoing cardiac surgery. Patients were surveyed before surgery, and 75% reported using CAM therapies. When prayer and vitamins were excluded, 44% reported using CAM therapies. Seventy-two percent of subjects were male, 76% were white, and 59% were well educated. No differences in overall CAM use were found among sex, age, race, or education level. The authors did offer an important recommendation. They noted that only 17% of patients had discussed their use of CAM therapies with their physicians, and 48% of patients did not want to discuss the topic at all. Since the frequency of CAM use found in this sample was consistent with the frequency of CAM use reported in the general population, the authors reinforced the importance of questioning patients about their use of CAM therapies.158
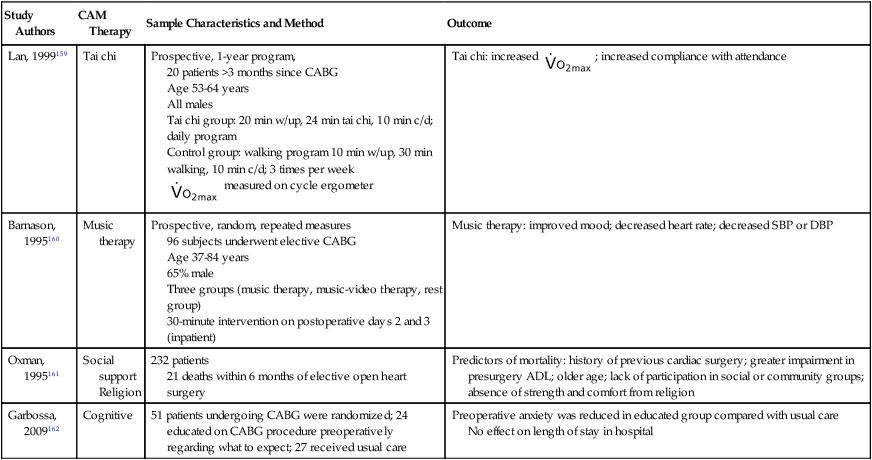
Evidence supporting the use of selected CAM therapies perioperatively is found in Table 27-8. Although methods were not always comprehensive in these studies, all demonstrated improvement in cardiovascular outcomes. In the study by Barnason and colleagues (1995)160 the authors concluded that effects of the music therapy on outcomes were consistent with a relaxation response, and in the study by Garbossa (2009),162 authors concluded that education and instruction in hospital routine significantly reduced preoperative anxiety when compared with control subjects.
Table 27-8
Effects of Selected CAM Therapies on Outcomes of Cardiovascular Surgery
| Study Authors | CAM Therapy | Sample Characteristics and Method | Outcome |
| Lan, 1999159 | Tai chi | Prospective, 1-year program, 20 patients >3 months since CABG Age 53-64 years All males Tai chi group: 20 min w/up, 24 min tai chi, 10 min c/d; daily program Control group: walking program 10 min w/up, 30 min walking, 10 min c/d; 3 times per week  measured on cycle ergometer measured on cycle ergometer |
Tai chi: increased  ; increased compliance with attendance ; increased compliance with attendance |
| Barnason, 1995160 | Music therapy | Prospective, random, repeated measures 96 subjects underwent elective CABG Age 37-84 years 65% male Three groups (music therapy, music-video therapy, rest group) 30-minute intervention on postoperative days 2 and 3 (inpatient) |
Music therapy: improved mood; decreased heart rate; decreased SBP or DBP |
| Oxman, 1995161 | Social support Religion |
232 patients 21 deaths within 6 months of elective open heart surgery |
Predictors of mortality: history of previous cardiac surgery; greater impairment in presurgery ADL; older age; lack of participation in social or community groups; absence of strength and comfort from religion |
| Garbossa, 2009162 | Cognitive | 51 patients undergoing CABG were randomized; 24 educated on CABG procedure preoperatively regarding what to expect; 27 received usual care | Preoperative anxiety was reduced in educated group compared with usual care No effect on length of stay in hospital |
In another small but clinically important study, Miller and Perry (1990)163 examined the benefit of a deep-breathing relaxation technique on pain tolerance in patients undergoing cardiac surgery. On the evening before surgery, 15 subjects were taught a slow, rhythmic, deep-breathing relaxation technique in addition to traditional preoperative instruction. The remaining 14 subjects only received the traditional preoperative instruction. All subjects were visited by the investigators on the day of surgery and on postoperative day 1 for conversation; however, only subjects in the intervention group were encouraged to perform the relaxation technique. Patients in the relaxation group had significant decreases in systolic and diastolic BP, HR, RR, and self-report of pain (on visual descriptor scale) when compared with controls. The authors concluded that “relaxation techniques may interrupt the pain-anxiety cycle” and that, although there were methodological problems with their study, this “may be an effective non-narcotic, noninvasive pain-relieving modality after” cardiac surgery. Additional study of the relaxation response has demonstrated a reduction in postoperative arrhythmias, as well as reduced tension and anger in patients undergoing cardiac surgery.32
Congestive Heart Failure
There are a limited number of published investigations on the effects of CAM therapies in patients with congestive heart failure (CHF). Results of several papers are summarized in Table 27-9. It is of interest that two of these papers used several interventions to achieve improved outcomes. This may be of value, given the multiplicity of systems affected in CHF. Unfortunately, the degree of ventricular impairment was not documented in these studies. In addition, care must be taken when interpreting results of single case studies of patients with cardiac disease. The placebo effect evoked by the investigator’s enthusiasm and expectation of success has been well studied in this population.169,170 Symptomatic and objective improvements have been documented in angina outcomes related to pharmacological interventions and after sham cardiac surgical procedures.
Table 27-9
Effects of Selected CAM Therapies in CHF
| Study Authors | CAM Therapy | Sample Method and Characteristics | Outcome |
| Moser, 1997164 | Skin-temperature biofeedback Relaxation Guided imagery |
40 patients with advanced CHF Randomized to intervention (BFR) or control (C) BFR included 1 session of skin-temperature biofeedback, guided imagery of hand warmth, and progressive muscle relaxation C group underwent measurement session but no intervention |
Baseline: comparable measurements between groups When comparing BFR with C, BFR showed: increased skin temperature in finger and foot; increased cardiac output; decreased systemic vascular resistance; decreased RR No changes in oxygen consumption or catecholamines were found in either group |
| Bernardi, 1998165 | Complete yoga breathing | 15 patients with CHF; 11 healthy volunteer controls (C) CHF patients were randomized to intervention (YB) or rest (R) YB included reduction of RR through controlled breathing (CB) and altered breathing pattern within each breath to include diaphragm, lower chest, then upper chest in inspiration and expiration, 1 hour per day for 1 month Measurements at baseline, end of 1 month and 1 month after completion Maximum symptom-limited cycle ergometer exercise test |
Baseline: SaO2 was lower during spontaneous breathing (SB) in CHF compared with C; SaO2 instability was higher during SB in CHF compared with C At 1 month: SaO2 decreased during SB in YB compared with R, and approximated C during CB R results compared with YB: decreased sensation of dyspnea; decreased SB rate 13.4 ± 1.5 to 7.6 ± 1.9 bpm; SaO2 (%) increased 92.5 ± 0.3 to 93.2 ± 0.4;  increased 13.9 to 15.9 ± 0.8; maximum cycle workload increased 92 ± 6 to 100 ± 4 watts increased 13.9 to 15.9 ± 0.8; maximum cycle workload increased 92 ± 6 to 100 ± 4 watts |
| Shinnick, 2002166 | Meditation Acupuncture Qi gong |
Case report 97-year-old terminally ill male Utilized interventions PRN |
Qi gong used to increase body temperature Acupuncture to help sleep and improve appetite Meditation increased peacefulness, lucidity, and ability to control breathing |
| Luskin 2002117 | Psychoeducational biofeedback (HeartMath, HM) |
Pilot study; 33 patients, NYHA Class 1-3; mean age 66 years 8-week intervention (HM) or control (C) HM received 10 hours training over 10 weeks and home program ≥5x/day |
When compared with C, HM decreased 22% perceived stress (C increased 7%) and decreased 34% depression (C increased 13%); HM significantly improved mental health and vitality on SF 36; HM increased 14% on 6 MWT (C decreased 2%) |
| Yeh G 2004167 | Tai Chi | 30 patients; NHYA Class 1-4; EF <40% (mean 23% ± 7%); mean age 64; 19 males Tai chi (TC) group received 1 hour tai chi 2x/week and usual care for 12 weeks, control (C) group received usual care Measurements were taken at baseline and at 12 weeks |
Compared with C, TC group improved QOL, increased distance on 6MWT, decreased serum BNP; there was a trend to increase  |
| Barrow 2007168 | Tai Chi Chuan and Chi Kung | 52 patients; NYHA 2-3; mean age 68.9; 42 males Patients were randomized to receive 55 minutes of tai chi (TC) 2x/week or standard care (C), for 16 weeks |
No difference was found in the Incremental Shuttle Walk Test between groups; significant improvement was found in TC group in symptom scores and reduction in depression scores |
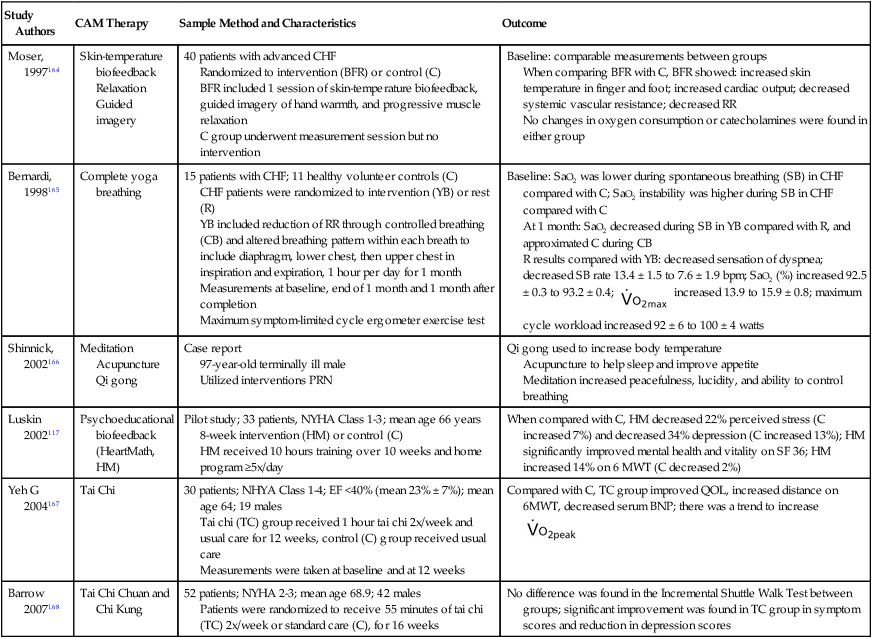
Two studies listed in Table 27-9 discuss the impact of tai chi on patients with CHF.167,168 The authors of both studies concluded that tai chi is a safe and effective adjunct in the usual management of patients with CHF. Authors suggest large randomized controlled trials are warranted for this population. Finally, a pilot study involving the impact of “HeartMath” on patients with CHF was reported.117 HeartMath includes a psychoeducational intervention that addresses “positive emotion refocusing and emotional restructuring.”109 Authors acknowledged that this intervention warrants further exploration; however, they concluded that improvements in emotional well-being carry over to improvements in functional capacity in patients with CHF.
Patients in the Coronary Care Unit
In two interesting, detailed, and well-designed studies, investigators examined the effects of intercessory prayer (praying for others) on outcomes of patients admitted to a coronary care unit.171,172 With only slight differences in design, Harris and colleagues attempted to replicate the results that Byrd demonstrated a decade earlier. Both studies were large, randomized, controlled, blinded trials (Byrd with 393 subjects, Harris with 990 subjects). Patients were admitted to the coronary care unit (CCU) with a wide variety of diagnoses in both studies. In addition to common cardiac diagnoses, patients had conditions such as pneumonia, chronic obstructive lung disease, diabetes mellitus, renal failure, sepsis, liver disease, and gastrointestinal bleeding. Patients were monitored for new problems, new diagnoses, and new therapeutic interventions that occurred after hospital admission through discharge. This information contributed to the scoring systems used by investigators to determine distinctions between recovery rates and severity of complications during hospitalization. Intercessors in the Byrd study were “born again” Christian individuals, while intercessors in the Harris study represented a variety of Christian traditions, including 35% nondenominational, 27% Episcopalian, and Protestant or Roman Catholic observers. In the original study, Byrd assigned three to seven intercessors to each patient in the intervention group. Intercessors were asked to pray daily (until hospital discharge) for the individual’s rapid recovery and prevention of complications, as well as contribute other prayers they believed would be beneficial to the patient. They were provided the patient’s first name, diagnosis, general condition, and pertinent updated information. Harris and colleagues randomly assigned a five-member team to pray for each patient. Intercessors were not given any information about the patient. They were asked to pray daily for 28 days for a “speedy recovery with no complications” and anything else the intercessor believed appropriate. Results from both studies demonstrated statistically significant better outcomes in patients who were prayed for when compared with those not prayed for. Although in both studies the length of hospital stay was not significantly different between control and intervention groups, the CCU course severity scores were significantly different between control and intervention groups. Control subjects in the Byrd study required more frequent ventilatory assistance, antibiotics, and diuretics than subjects in the intervention group. Control subjects in the study by Harris and colleagues received higher scores on a scale quantifying severity of clinical outcomes from excellent to catastrophic than did subjects in the intervention group.
The basis of this therapeutic effect of distance healing remained unexplained by the authors. The outcomes provided by these two randomized controlled clinical trials, however, warrant continued exploration into the possible benefits of intercessory prayer in medical outcomes. McCullough and colleagues (2000)173 reported data from 42 publications in a metaanalysis examining the association of religious involvement to all-cause mortality. Their results resonate with those of the Byrd and Harris studies, and they concluded, from sampling more than 126,000 participants, that religious involvement was significantly associated with lower mortality rates. Similarly, they recommend that “elucidating the nature of this robust but poorly understood association could be a fruitful topic for future research at the interface of psychology and health.”173
Music has been used as a method to induce relaxation in patients in the CCU. Bolwerk (1990)174 presented 17 patients (11 males) with music therapy within the first 48 hours of CCU admission after experiencing an acute MI. Eighteen control patients (16 males) were given usual care. Anxiety levels were monitored in both groups within 48 hours of hospital admission and again 3 days later. Both groups were similar at baseline. Those patients in the intervention group received 3 consecutive days of 22 minutes of “relaxing, calming” music. At repeat testing, significantly greater reductions in anxiety scores were found in those individuals who received music therapy compared with the control group. Although there were significant limitations in the design of the study, the authors concluded that the repetitive nature of music can reduce anxiety in patients experiencing an acute MI.
Pulmonary Conditions
Asthma
Numerous factors have been implicated as causative agents of asthma. In addition to respiratory infection and allergens, emotional stress has been identified as a trigger. Generalized panic symptoms have been found to be both a cause of asthma as well as a response to an exacerbation of asthma. Panic and anxiety states correlate with hyperventilation, a symptom closely related to a hyperactive respiratory drive. A heightened respiratory drive is not always favorable in individuals with known asthma because it can further challenge airways that are already bronchoconstricted.81 Hyperventilation itself may exacerbate asthma because the rapid movement of cooler and dryer air into the airways can trigger further bronchoconstriction.
Repressive coping styles have also been associated with asthma morbidity.81 Individuals with this behavior pattern typically ignore their symptoms, including dyspnea, and fail to seek timely health care. These individuals tend to have relatively high levels of endogenous opioids, neurochemicals that can depress unpleasant sensations. Consequently, these substances may limit an individual’s ability to recognize early signs of bronchoconstriction. Additional evidence suggests that reduced immune system responsiveness in the setting of chronic emotional stress heightens inflammatory and infective processes, both of which are implicated in asthma exacerbation.
Numerous CAM therapies have been studied in attempts to reverse a number of these factors associated with asthma morbidity. Many of these studies have methodological shortcomings; however, several are well designed and provide insights into possible mechanisms of intervention efficacy. It is reported that between 4% and 79% of adults with asthma and between 33% and 89% of children with asthma use CAM therapies as part of their disease management regimen.175 Relaxation therapy has been widely investigated; however, the results are inconsistent.176,177 In a metaanalysis of six studies on the effects of relaxation training in children with emotionally triggered asthma, McQuaid and Nassau (1999)178 concluded that “relaxation training is probably a most efficacious intervention” in this population. They noted concern regarding methods used in the articles reviewed and noted that only three of the studies reviewed in this analysis used appropriate controls, and only one examined maintenance of posttreatment effect. Although statistical significance was achieved in these investigations, the reduction of symptoms was less than 10% of baseline values, leading the authors to believe that the changes would not be clinically significant. Lehrer (1998)81 also concluded that relaxation therapy may only be effective with specific asthma patients. His results indicate significant improvement in asthma exacerbation in individuals with emotionally triggered events when relaxation interventions are used. He noted worsening of symptoms when they were acute, however, and concluded that “relaxation training may provide protection from emotionally induced asthma”81 when symptoms are chronic. Some theories regarding the failure of relaxation therapy to benefit individuals with asthma relate to its effect on the ANS. Evidence demonstrates that relaxation therapy downregulates the beta receptors of the SNS and thus reduces bronchodilation, an unfavorable outcome for individuals with asthma.
In a metaanalysis of 31 studies published between 1972 and 1993, Devine reported on the effects of psychoeducational care on adults with asthma. Psychoeducational interventions were defined as “education, behavioral skill development, cognitive therapy, and/or nonbehavioral support/counseling.”179 The author concluded that, despite methodological flaws primarily due to small numbers of subjects, education and relaxation-based behavioral interventions demonstrated improvement in clinical measures of pulmonary function. These measures included peak expiratory flow rate (PEFR), functional status, regimen compliance, use of medications, psychological well-being, and ability to use an inhaler properly. Similarly, a review of 12 well-designed studies investigating the effects of limited asthma education (information only) demonstrated a significant improvement in perceived asthma symptoms and reduced visits to the emergency department in adults with asthma.180 In a controlled study of 35 children ages 5 to 6 years, researchers investigated the effects of a 6-month psychoeducational program that included guided imagery on several clinical and immunological outcomes associated with asthma control.181 In addition to education classes and workshops for parents, daily instruction was given to the children to imagine visual images of unobstructed airways, mast cells, and immunoglobulin E (IgE) suppression. The results demonstrated significant reductions in the number of asthmatic episodes requiring medical attention and reduced bronchodilator requirements in the intervention group when compared with the control group. Spirometric values, specifically forced expiratory volume in 1 second (FEV1), improved in the intervention group despite reduction in bronchodilator use. In addition, markers associated with immune system function (specific IgE levels, leukocyte surface markers, B cells) demonstrated improved efficiency. Conversely, a review of eight clinical trials investigating the effects of a limited asthma education program on more than 1400 children with asthma failed to demonstrate any reduction in emergency department visits or hospital admissions.182 It appears that the addition of a guided imagery program to an asthma education program improves outcomes in children.
In a well-designed RCT of the effects of guided imagery on a group of adult patients with asthma, outcome measures failed to reveal statistically significant differences between intervention and control groups.183 Measures of FEV1, anxiety, depression, quality-of-life scales, and the number of visits to the emergency department were not different between groups. Those subjects who practiced mental imagery, however, demonstrated statistically significant decreases in medication usage and reported feeling more power and control in their ability to change the course of their disease. Authors stressed the pilot nature of this study and concluded that if a larger sample was studied, more significant outcomes may have been achieved because there were trends favoring the mental imagery group in all outcome measures.
Preliminary study of the effects of the Alexander technique on measures of pulmonary function warrants further investigation.184–186 To date, no controlled studies investigating the effects of this technique on individuals with asthma have been published. Although performing artists (musicians, singers, actors) with or without asthma reportedly benefit from this intervention, systematic study is lacking. Austin and Ausubel (1992)184 documented improved pulmonary function measures in 10 healthy adults after 20 private sessions of therapy with the Alexander technique. No such improvement was found in 10 healthy adults in an untreated matched control group. Significant increases were demonstrated in PEFR, maximum voluntary ventilation (MVV), maximal inspiratory pressure (MIP), and maximal expiratory mouth pressure (MEP).
Both EMG and thermal biofeedback interventions have been studied in the management of asthma. Several of these interventions have been aimed at increasing HR. It has been postulated that by increasing HR, the accompanying increase in beta SNS activity produces increased bronchodilation. The few studies investigating this intervention have not been able to validate this theory due to design flaws.81 Other trials of biofeedback have focused on general muscle relaxation and facial muscle relaxation. In a comprehensive review, McQuaid and Nassau (1999)178 concluded that studies investigating biofeedback with general muscle relaxation demonstrate similar results as those trials using relaxation without biofeedback. These results are inconclusive and conflicting in individuals with asthma. Similarly, Ritz and colleagues (2004)187 recently concluded in their review that studies addressing the use of biofeedback in the treatment of asthma were of poor quality and limited their ability to recommend this intervention. There is, however, strong evidence supporting the use of EMG biofeedback on the frontalis muscle of children with asthma.178,188 Tension in this muscle has been correlated with increased airway resistance, presumably a consequence of a trigeminal-vagal reflex. Well-designed, carefully detailed studies examining reduced tension in facial muscles have demonstrated improvements in clinical measures of pulmonary function, including PEFR and asthma severity.188
The effects of yoga on asthma have been investigated by several authors. A summary of selected studies is found in Table 27-10. Results of these studies are still insufficient to draw sound conclusions. These initial trials, however, provide reasonable evidence supporting the use of yoga as complementary in the management of asthma. Although a discussion of breathing techniques is outside the scope of this chapter, there is evidence suggesting the value of certain interventions in asthma management.193 Yoga breathing overlaps with some of these breathing exercises (e.g. slow, deep breathing mimics pranayama yoga exercise). In addition, Wronski (2008)194 offered a preliminary discussion of the benefits of Pilates breathing in children with asthma.
Table 27-10
| Study Authors | Type of Yoga | Sample Characteristics and Method | Outcomes |
| Tandon, 1978189 | Yogic breathing exercises and posture | 22 patients with severe chronic airway obstruction Matching groups of 11 subjects Yoga group (YG) and control group (CG) followed-up monthly for 9 months; CG received physiotherapy breathing |
Compared with CG, the YG showed: significant increase in maximum work by 60.55 kpm; symptomatic improvement |
| Jain, 1991190 | Yoga | 46 young individuals with asthma Age 11-18 years All had history of childhood asthma Subjects acted as their own controls |
Compared with baseline, significant increase in pulmonary function and exercise capacity At 2-year follow-up, reduced symptoms and drug requirements |
| Vedanthan, 1998191 | Slow breathing (pranayama) Postures (asanas) Meditation |
Adults with asthma Age 19-52 years 17 volunteers randomly divided into yoga (YG) and nonyoga groups (NYG) YG practiced 3 times per week for 16 weeks Both groups maintained daily symptom and medication diaries; AM and PM PEFR; weekly spirometry and questionnaires |
Compared with NYG, the YG showed: significant degree of relaxation and positive attitude; better yoga exercise tolerance; trend towards decreased use of beta adrenergic inhalers; no difference in pulmonary function measures |
| Sodhi, 2009192 | Yoga breathing | 128 patients with mostly mild asthma randomized into 2 groups, 8 weeks of yoga training (YT) or control (C); PFT performed at baseline, 4 and 8 weeks |
YT group increased % predicted PEFR, FEV1, FVC, FEF25-75, FEV1/FVC when compared with C |
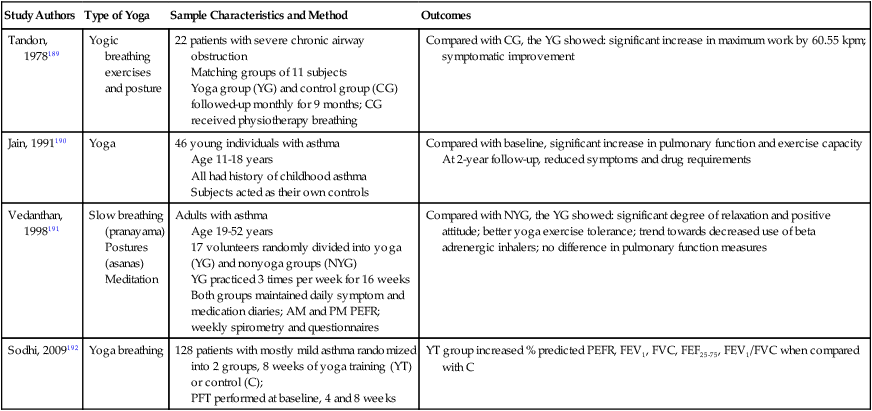
Writing about emotionally traumatic events has been shown to have physical and psychological benefits. Smyth and colleagues (1999)195 studied 58 adults with asthma (mean age 41 years). Subjects were randomized to an intervention group that was instructed to write about the most stressful event in their lives, while the control group wrote about an emotionally neutral event. Subjects were instructed to write for 20 minutes, on three consecutive days. At a 2-week follow-up, mean FEV1 in the intervention group increased significantly from 63.9% of predicted values to 76.3% of predicted values. These statistically significant improvements were maintained at 2- and 4-month follow-up testing. No changes in FEV1 were noted in the control group. Although the results of this study are complicated by the inclusion of subjects with rheumatoid arthritis, the authors offer strong preliminary evidence for the value of this writing intervention.
Most of the CAM therapies discussed thus far in the management of asthma have been mind/body techniques. Although there is a paucity of publications addressing the effects of body work on asthma, the effects of manual therapy on asthma have been reviewed.196,197 In general, the methodological differences between all studies and the shortcomings of each individual study preclude any strong recommendation supporting the use of manual therapy in the treatment of asthma. Two of the studies reported on chiropractic manipulation as compared with sham maneuvers, and a third compared massage therapy with a relaxation control group. Significant improvement in measures of lung function was found in the massage therapy study. Two studies found no differences between intervention and control groups when chest physiotherapy was compared with placebo and when footzone (reflexology) therapy was compared with a no-treatment control group.
Acupuncture, a form of energy work, has been discussed extensively in the management of asthma. Several review studies and metaanalyses have been published addressing the effects of acupuncture on various outcomes related to asthma.198–201 Inclusion criteria for an article to be reviewed in one of these publications consisted of randomized control design and measurement of objective pulmonary function outcomes, most often FEV1. Significant disagreement exists among investigators regarding details of acupuncture interventions, including proper location of needles, depth of needle penetration, and frequency and duration of treatment.202–205 There is general agreement, however, that strong evidence exists to support the process of inserting acupuncture needles into individuals with asthma. Medici and colleagues204 have demonstrated that whether or not the actual point of needle insertion is considered proper is unessential. They successfully demonstrated that regardless of the site of needle insertion, certain physiological responses occur with acupuncture that improve pulmonary function in patients with asthma. They offer several possible rationales for the improvement—a direct physiological release of substances in response to the invasiveness of inserting the needles into the body, a physiological response triggered by the interaction between practitioner and subject (including the intention of the practitioner to heal the subject), or some other unknown, as yet undefined, factor. Hence most investigators conclude that more research is necessary to understand the complexities of acupuncture as an intervention and how it can best be prescribed in the treatment of asthma. It is important to note here that although very rare, there have been a few reports of pneumothorax and cardiac tamponade occurring consequent to needle insertion in the thorax.206
Preliminary evidence exists that qi gong may be an effective adjunct to medical management of asthma.111 When pharmacological intervention is combined with qi gong, reported benefits include symptom reduction, improved immune system function, decreased sick leave and hospitalization days, decreased emergency department visits, and decreased antibiotic requirements for bronchial infections. These effects could result in a reduction in asthma-related morbidity and a substantial cost savings.
Chronic Obstructive Pulmonary Diseases
Pulmonary rehabilitation programs have been traditionally used as adjuncts to pharmacological management of chronic obstructive pulmonary disease (COPD). These programs generally consist of exercise training and a variety of educational and supportive interventions. Strong evidence has been shown to support pulmonary rehabilitation interventions in improving outcomes in patients with COPD.207–211 These outcomes include reduced perception of dyspnea, increased work tolerance, and increased physical conditioning. Results, however, are inconsistent with regard to improvements in pulmonary function measures.
Devine and Pearcy (1996)179 performed a metaanalysis of 65 studies investigating the effects of psychoeducational therapies in adults with COPD. For purposes of their analysis, they included education, exercise, and/or psychosocial support as psychoeducational therapies. Most of the articles were found in journals (66%) and dissertations (29%) and were published between 1954 and 1994. Of the studies, 34% were RCTs, 54% included a control group, and 15% had a placebo-type control. Data were included on 3642 individuals, with 72% reported as having COPD, 25% reported as having COPD or asthma, and 3% as having COPD, asthma, or other chronic pulmonary disease. Subjects ranged in age between 43 and 70 years, 81% of the studies had more men than women, and 19% had men only. Almost half of the studies were conducted in an outpatient setting, and about one-fourth were conducted in the inpatient hospital setting. The remaining studies involved various settings, including home.
Although the results of Devine and Pearcy’s analysis revealed significant benefits of various interventions, the authors noted methodological weaknesses in many of the studies, including no mention of the duration of intervention in almost half of them. Statistically significant benefits of the various interventions are listed in Table 27-11. In general, education-only interventions were of benefit in improving the subject’s knowledge of psychomotor skills. Relaxation-type interventions were effective in improving dyspnea and psychological well-being. An overwhelming benefit of pulmonary rehabilitation interventions was demonstrated in many studies. All of the pulmonary rehabilitation programs included in this analysis had education and large-muscle exercise components; 75% had breathing retraining; 57% had relaxation training; 54% had physical therapy; 43% had psychosocial support; 40% had occupational therapy; 29% had nutritional education; and 18% had vocational counseling. Although the results of this analysis begin to shed light on the benefits of individual interventions, more research is warranted. Recognition of the contribution of each of the specific CAM therapies offered within the umbrella of pulmonary rehabilitation may be difficult. This is consistent with Devine and Pearcy’s conclusion that further research efforts to break down interventions within pulmonary rehabilitation may not be clinically wise, given the complex needs of these patients.
Table 27-11
Effect of Various Psychoeducational Interventions on Outcomes in Individuals with COPD
| Outcome Variable and Measurement | Number of Studies | Statistically Significant Beneficial Interventions | Nonstatistically Beneficial Interventions |
| Psychological well-being (e.g., anxiety, mood questionnaires) | 26 | Relaxation-type therapy Pulmonary rehabilitation |
Education only |
| Endurance (e.g., time/distance able to exercise) | 16 | Pulmonary rehabilitation | Education |
Oxygen uptake ( ) ) |
8 | Vigorous exercise (e.g., 60 minutes of supervised exercise 3 times per week for 9 weeks) | Mild exercise (e.g., 10 minutes of exercise 3 times per day)* |
| Functional status (e.g., sickness impact profile) | — | Pulmonary rehabilitation Breathing exercise and large muscle exercises |
Education only |
| Dyspnea (visual analogue scales) | — | Pulmonary rehabilitation Progressive muscle relaxation |
Guided imagery |
| Pulmonary function (static volumes and FEV1) | — | Static volumes improved Pulmonary rehabilitation |
FEV1 no change Education only relaxation/imagery Pulmonary rehabilitation |
| Knowledge of psychomotor skills (e.g., accurate inhaler use) | — | Education only | |
| Adherence (self-reports, provider assessed compliance) | — | Pulmonary rehabilitation | Education only |
| Utilization of health care (e.g., ED visits, hospitalizations and LOS) | — | Pulmonary rehabilitation | Education only |
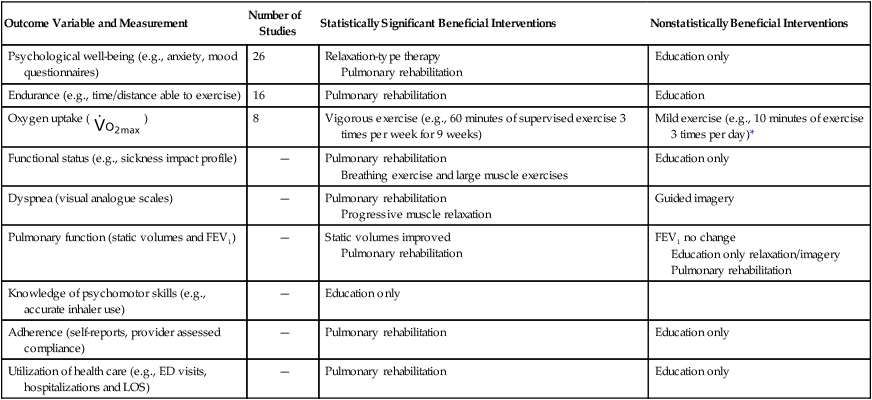
ED, Emergency department; LOS, length of stay.
Based on data from Devine EC, Pearcy J: Meta-analysis of the effects of psychoeducational care in adults with chronic obstructive pulmonary disease, Patient Education and Counseling 29:167–178, 1996.
In a recent review of psychological interventions for individuals with cystic fibrosis (CF), Glasscoe and Quittner (2009)212 found 13 randomized controlled trials studying 529 pooled participants. Interventions were primarily behavioral or educational and focused on promoting improved quality of life and knowledge for effective disease management. Patients and family members demonstrated improvement in emotional and knowledge-based outcomes; no consistent lung function measurement outcomes were noted.
Intuitively, yoga would seem a beneficial adjunct to the medical management of COPD. Components of yoga include slow breathing, or pranayama, and body positions, or asanas. At times meditation is included as well. Unfortunately, investigation of the effects of yoga on COPD is in its infancy and is still mostly anecdotal.213 The reports include improved perceptions of dyspnea and decreased anxiety.
Similarly, singing therapy would appear to benefit individuals with breathing impairments. Irons (2010a; 2010b)214,215 performed two appropriate literature reviews to study this: one to determine the effects of singing therapy on individuals with bronchiectasis, and one on individuals with CF. No studies were found for either population. Alternatively, music therapy, used primarily for relaxation, has been found effective as a complement to chest physical therapy in toddlers with CF216 and in adults with infectious lung diseases.217 In a recent review, Huth (2005)218 reported on the benefits of massage therapy in the same populations. Individuals with CF and those with chronic lung disease demonstrated reduction in anxiety and improved measures of pulmonary function after 2 to 4 weeks of a 20-minute intervention. Further research is needed because these studies were small and had numerous methodological limitations.
Lung Cancer
Two large and thorough reviews recently reported on noninvasive interventions used for patients with lung cancer.219,220 Only randomized controlled trials were included, and several of the studies analyzed were common to both reviews. Sola (2009)220 categorized studies into six groups according to intervention, including the use of treatments for breathlessness, structured nursing support programs, nutritional intervention, psychotherapeutic interventions, exercise, and reflexology. Primary outcome measures were well-being and quality of life. Measures of pulmonary function were not reported; measures of functional activity were reported in two studies. All studies reported significant improvement in well-being or in quality of life in the intervention groups when compared with controls. When breathlessness was the primary outcome measure, all studies also reported significant improvement in the intervention group when compared with controls.219 Interventions for breathlessness included individualized counseling and psychosocial support, breathing control training, relaxation and anxiety management, and activity pacing. The authors of both reviews recommended caregiver training for this population given the many components of intervention required to effectively tailor a noninvasive program for each individual. They also suggested large, well-designed, higher-quality studies in the future.

 , Maximum oxygen uptake (in L/min or mL/kg/min);
, Maximum oxygen uptake (in L/min or mL/kg/min);  , ventilatory equivalent for oxygen; Vf, ventilatory frequency in breaths per minute; VD/VT, ratio of dead space ventilation to tidal volume; METs, metabolic equivalents (1 MET = 3.5 mL of oxygen/kilogram/weight).
, ventilatory equivalent for oxygen; Vf, ventilatory frequency in breaths per minute; VD/VT, ratio of dead space ventilation to tidal volume; METs, metabolic equivalents (1 MET = 3.5 mL of oxygen/kilogram/weight). , Oxygen consumption (mL/min); RR, respiratory rate (breath rate); TV, tidal volume (breath volume), CM, cyclic meditation; SH, shavasana; TM, treadmill; HR, heart rate; %MHR, percent maximum heart rate.
, Oxygen consumption (mL/min); RR, respiratory rate (breath rate); TV, tidal volume (breath volume), CM, cyclic meditation; SH, shavasana; TM, treadmill; HR, heart rate; %MHR, percent maximum heart rate. , peak oxygen uptake; QOL, quality of life; BNP, brain naturietic peptide
, peak oxygen uptake; QOL, quality of life; BNP, brain naturietic peptide


