Common peripheral nerve lesions
Peripheral nerves can be affected in isolation, so-called mononeuropathies. However, only a few peripheral nerves are involved frequently. The commonly involved nerves are usually affected by entrapment at sites of vulnerability. This can be exacerbated by conditions that render the nerves more susceptible, for example diabetes and hereditary liability to pressure palsies. Isolated mononeuropathies can rarely be the onset of mononeuritis multiplex (see above).
The types of nerve injury are given in Table 1. Injuries are usually a combination of neuropraxias with some axonotmesis.
| Type of nerve injury | Structural changes | Rate of recovery |
|---|---|---|
| Neuropraxia | Myelin damage, axon intact | 2–12 weeks |
| Axonotmesis | Loss of axonal continuity, epineurium intact | Regeneration at 1 mm/day from site of lesion |
| Neurotmesis | Entire nerve trunk separated | No regeneration unless nerve repaired; then 1 mm/day |
Median nerve
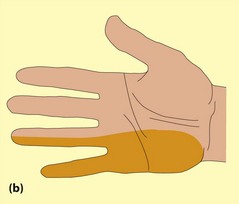
It commonly presents between 40 and 60 years of age, more often in women. The dominant hand is usually affected first. Initially patients are awoken with tingling and pain in the hand, which they characteristically shake on waking ‘like a wet fish’. Later they notice tingling or numbness during the day. They may start dropping things and note some weakness of grip. If severely affected, they may notice wasting of the abductor pollicis brevis (APB; Fig. 1a).

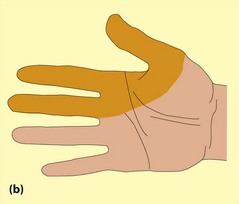
Fig. 1 Median nerve. (a) Wasting of abductor pollicis brevis; (b) sensory loss of median nerve lesions.
On examination, there may be wasting or weakness of the APB. Sensory changes of varying degrees are found within the median nerve distribution (Fig. 1b). Additional tests include Tinel’s test (percussion of the nerve to provoke paraesthesiae in the median nerve distribution) and Phalen’s test (dorsiflexing the wrist for 30–60 s). However, there are significant doubts about the sensitivity and specificity of these tests.
Ulnar nerve
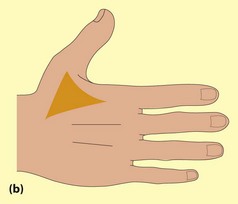
Numbness and tingling in the little and ring finger and a more diffuse arm pain are the common presentations. The patient may be aware of weakness in the hand. On examination, there may be weakness and wasting in the interossei (Fig. 2a), with weakness of the long flexors of the little and ring fingers. Sensory loss may be demonstrated in the ulnar nerve distribution (Fig. 2b).
Definitive diagnosis depends again on nerve conduction studies. The differential diagnosis of the unilateral wasted hand includes T1 lesions, in which all hand muscles are affected and the sensory loss is in the axilla. If hand wasting is bilateral, the differential diagnosis includes amyotrophic lateral sclerosis (p. 108), more generalized neuropathies (especially CMT; p. 105) and, very rarely, syringomyelia.
The management depends on severity and aetiology. Following external compression, conservative treatment and avoidance of further compression are effective. If the nerve is significantly affected and there is evidence of abnormalities at the elbow, then surgical decompression or transposition can be effective.
Radial nerve
Radial nerve lesions commonly result from compression of the radial nerve against the humerus in the upper arm and usually occur during deep sleep or unconsciousness, for example after an alcoholic binge (’Saturday night palsy’), or with fracture of the humerus. There is usually a striking weakness in the wrist and finger extensors (Fig. 3). The triceps and brachioradialis are less markedly affected. The triceps reflex is occasionally impaired. There is limited sensory disturbance with a small area of sensory loss at the base of the thumb. Even though the weakness is limited to the extensors of the fingers, the patient feels the whole hand is useless. It is important to examine finger abduction and adduction and APB with the hand placed flat (e.g. on a table) and the fingers extended.
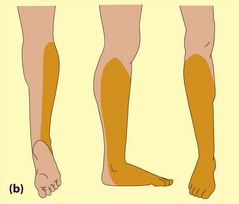
Common peroneal nerve
The common peroneal nerve is vulnerable as it runs around the fibula head. This can be injured by external pressure (coma, plaster casts, carpet laying, leg crossing), trauma and entrapment in the fibular tunnel. The presentation is of foot drop (Fig. 4a). There may be wasting of tibialis anterior, with weakness of dorsiflexion, toe extension and foot eversion with preservation of foot inversion. The sensory loss is illustrated in Figure 4b.
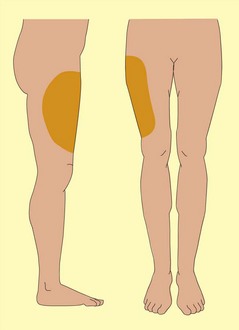
Lateral cutaneous nerve of the thigh (meralgia paraesthetica)
Lesions of this nerve are very common. Patients notice an area of burning or numbness on the outer aspect of the thigh (Fig. 5). A large number of possible causes have been cited with limited evidence, weight change being among the most common. This is usually a self-limiting condition and requires no investigation.