Chapter 675 Common Fractures
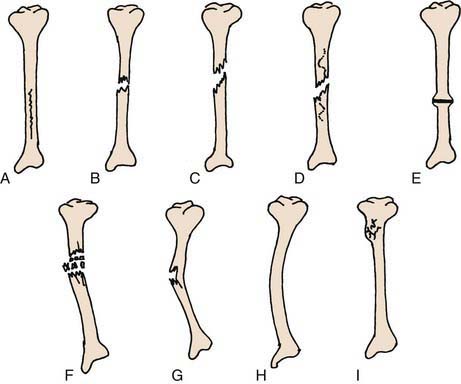
Trauma is a leading cause of death and disability in children >1 yr of age. Several factors make fractures of the immature skeleton different from those involving the mature skeleton. The anatomy, biomechanics, and physiology of the pediatric skeletal system are different from those of adults. This results in different fracture patterns (Fig. 675-1), diagnostic challenges, and management techniques specific to children to preserve growth and function.
675.1 Unique Characteristics of Pediatric Fractures
Fracture Remodeling
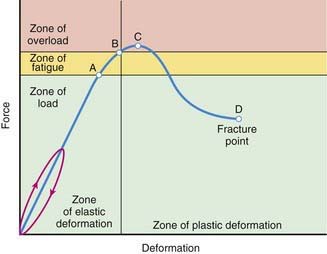
Remodeling is the 3rd and final phase in biology of fracture healing, preceded by the inflammatory and reparative phases. This occurs from a combination of appositional bone deposition on the concavity of deformity, resorption on the convexity, and asymmetric physeal growth. Thus, reduction accuracy is somewhat less important than it is in adults (Fig. 675-2). The 3 major factors that have a bearing on the potential for angular correction are skeletal age, distance to the joint, and orientation to the joint axis. The rotational deformity and angular deformity not in the axis of the joint motion are less likely to remodel. The amount of remaining growth provides the basis for remodeling; younger children have greater remodeling potential. Fractures adjacent to a physis undergo the greatest amount of remodeling, provided that the deformity is in the plane of the axis of motion for that joint. The fractures away from the elbow and closer to the knee joint have greater potential to remodel because this physis provides maximal growth to the bone. One can expect remodeling to occur over the next several months following injury throughout skeletal maturity. Skeletal maturity is reached in girls between 13 and 15 yr and in boys between 14 and 16 yr of age.
Progressive Deformity
Injuries to the physes can be complicated by progressive deformities with growth. The most common cause is complete or partial closure of the growth plate. As a consequence, angular deformity, shortening, or both, can occur. The partial arrest may be peripheral, central, or combined. The magnitude of deformity depends on the physis involved and the amount of growth remaining. CT and MRI are important for assessing partial arrests and formulating treatment (Fig. 675-3).
Beaty JH, Kasser JR, editors. Rockwood and Wilkins’ fractures in children, ed 5, Philadelphia: JB Lippincott, 2001.
Flynn JM, Kolze EA. Upper extremity injuries. In: Dormans JP, editor. Pediatric orthopaedics: core knowledge in orthopaedics. Philadelphia: Mosby; 2005:47-84.
Flynn JM, Nagda S. Upper extremity injuries. In: Dormans JP, editor. The requisites in pediatrics: pediatric orthopaedics and sports medicine. Philadelphia: Mosby; 2005:21-48.
Green NE, Swiontkowski MF, editors. Skeletal trauma in children, ed 3, vol 3. Philadelphia: WB Saunders, 2001.
Olney RC, Mazur JM, Pike LM, et al. Healthy children with frequent fractures: how much evaluation is needed? Pediatrics. 2008;121:890-897.
Overly F, Steele DW. Common pediatric fractures and dislocations. Clin Pediatr Emerg Med. 2002;3:106-117.
Poolman RW. Adjunctive non-invasive ways of healing bone fractures. BMJ. 2009;338:611-612.
Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;45:587-622.
Thompson GH, Haber LL. Upper extremity fractures in the pediatric patients. In: Fitzgerald RHJr, Kaufer H, Malkani A, editors. Orthopaedics. St Louis: Mosby; 2002:484-494.
675.2 Pediatric Fracture Patterns
Plastic Deformation
Plastic deformation is unique to children. It is most commonly seen in the ulna and occasionally the fibula. The fracture results from a force that produces microscopic failure on the tensile side of bone and does not propagate to the concave side (Fig. 675-4). The concave side of bone also shows evidence of microscopic failure in compression. The bone is angulated beyond its elastic limit, but the energy is insufficient to produce a fracture. Thus, no fracture line is visible radiographically (Fig. 675-5). The plastic deformation is permanent, and a bend in the ulna of <20 degrees in a 4 yr old child is expected to correct with growth.
Buckle or Torus Fracture
A compression failure of bone usually occurs at the junction of the metaphysis and diaphysis, especially in the distal radius (Fig. 675-6). This injury is referred to as a torus fracture because of its similarity to the raised band around the base of a classic Greek column. They are inherently stable and heal in 3-4 wk with simple immobilization.
Epiphyseal Fractures
The injuries to the epiphysis involve the growth plate. There is always a potential for deformity to occur, and hence long-term observation is necessary. The distal radial physis is the most commonly injured physis. Salter and Harris (SH) classified epiphyseal injuries into 5 groups (Table 675-1 and Fig. 675-7). This classification helps to predict the outcome of the injury and offers guidelines in formulating treatment. SH type I and II fractures usually can be managed by closed reduction techniques and do not require perfect alignment, because they tend to remodel with growth. SH type II fractures of the distal femoral epiphysis need anatomic reduction. The SH type III and IV epiphyseal fractures involve the articular surface and require anatomic alignment to prevent any step off and realign the growth cells of the physis. SH type V fractures are usually not diagnosed initially. They manifest in the future with growth disturbance. Other injuries to the epiphysis are avulsion injuries of the tibial spine and muscle attachments to the pelvis. Osteochondral fractures are also defined as physeal injuries that do not involve the growth plate.
| SALTER-HARRIS TYPE | CHARACTERISTICS |
|---|---|
| I | Separation through the physis, usually through the zones of hypertrophic and degenerating cartilage cell columns |
| II | Fracture through a portion of the physis but extending through the metaphyses |
| III | Fracture through a portion of the physis extending through the epiphysis and into the joint |
| IV | Fracture across the metaphysis, physis, and epiphysis |
| V | Crush injury to the physis |
Child Abuse
The orthopedic surgeon sees 30-50% of physically abused children. Child abuse should be expected in nonambulatory children with lower extremity long bone fractures (Chapter 37). No fracture pattern or types are pathognomonic for child abuse; any type of fracture can result from nonaccidental trauma. The fractures that suggest intentional injury include femur fractures in nonambulatory children, distal femoral metaphyseal corner fractures, posterior rib fractures, scapular spinous process fractures, and proximal humeral fractures. A skeletal survey is essential in every suspected case of child abuse, because it can demonstrate other fractures in different stages of healing. Radiographically, some systemic diseases mimic signs of child abuse, such as osteogenesis imperfecta, osteomyelitis, Caffey disease, and fatigue fractures. Many hospitals have a multidisciplinary team to evaluate and treat patients who are victims of child abuse. It is mandatory to report these cases to social welfare agencies.
Bandyopandhyay S, Yen K. Non-accidental fractures in child maltreatment syndrome. Clin Pediatr Emerg Med. 2002;3:145-152.
Davidson JS, Brown DJ, Barnes SN, et al. Simple treatment for torus fractures of the distal radius. J Bone Joint Surg Br. 2001;83:1173-1175.
Della-Giustina K, Della-Giustina DA. Emergency department evaluation and treatment of pediatric orthopedic injuries. Emerg Med Clin North Am. 1999;17:895-922.
Drendel AL, Gorelick MH, Weisman SJ, et al. A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553-560.
Green NE, Swiontkowski MF, editors. Skeletal trauma in children, ed 3, vol 3. Philadelphia: WB Saunders, 2001.
Jadhav SP, Swischuk LE. Commonly missed subtle skeletal injuries in children: a pictorial review. Emerg Radiol. 2008;15(6):391-398.
Kemp AM, Dunstan F, Harrison S, et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ. 2008;337:a1518.
Olney RC, Mazur JM, Pike LM, et al. Healthy children with frequent fractures: how much evaluation is needed? Pediatrics. 2008;121:890-897.
Overly F, Steele DW. Common pediatric fractures and dislocations. Clin Pediatr Emerg Med. 2002;3:106-117.
Plint AC, Perry JJ, Correll R, et al. A randomized, controlled trial of removable splinting versus casting for wrist buckle fractures in children. Pediatrics. 2006;117:691-697.
Poolman RW. Adjunctive non-invasive ways of healing bone fractures. BMJ. 2009;338:611-612.
Thompson GH, Haber LL. Upper extremity fractures in the pediatric patients. In: Fitzgerald RHJr, Kaufer H, Malkani A, editors. Orthopaedics. St Louis: Mosby; 2002:484-494.
675.3 Upper Extremity Fractures
Phalangeal Fractures
The different phalangeal fracture patterns in children include physeal, diaphyseal, and tuft fractures. The mechanism of injury is a direct blow to the finger or typically a finger trapped in a door (Chapter 673). Crush injuries of the distal phalanx manifest with severe comminution of the underlying bone (tuft fracture), disruption of the nail bed, and significant soft-tissue injury. These injuries are best managed with antibiotics, tetanus prophylaxis, and irrigation. A mallet finger deformity is the inability to extend the distal portion of the digit and is caused by a hyperextension injury. It represents an avulsion fracture of the physis of the distal phalanx. The treatment is splinting the digit in extension for 3-4 wk. The physeal injuries of the proximal and middle phalanx are similarly treated with splint immobilization. Diaphyseal fractures may be oblique, spiral, or transverse in fracture geometry. They are assessed for angular and rotational deformity with the finger in flexion. Any malrotation or angular deformity requires correction for optimal functioning of the hand. These deformities are corrected with closed reduction, and if unstable, they need stabilization.
Appleboam A, Reuben AD, Benger JR, et al. Elbow extension test to rule out elbow fracture: multicentre, prospective validation and observational study of diagnostic accuracy in adults and children. BMJ. 2009;338:31-34.
Bohm ER, Bubbar V, Hing KY, et al. Above- and below-the-elbow plaster casts for distal forearm fractures in children. J Bone Joint Surg Am. 2006;88:1-8.
Davidson JS, Brown DJ, Barnes SN, et al. Simple treatment for torus fractures of the distal radius. J Bone Joint Surg Br. 2001;83:1173-1175.
Della-Giustina K, Della-Giustina DA. Emergency department evaluation and treatment of pediatric orthopedic injuries. Emerg Med Clin North Am. 1999;17:895-922.
Jadhav SP, Swischuk LE. Commonly missed subtle skeletal injuries in children: a pictorial review. Emerg Radiol. 2008;15(6):391-398.
Kocher MS, Waters PM, Micheli LJ. Upper extremity injuries in the pediatric athlete. Sports Med. 2000;30:117-135.
Kropman RHJ, Bemelman M, Segers MJM, et al. Treatment of compacted greenstick forearm fractures in children using bandage or cast therapy: a prospective randomized trial. J Trauma. 2010;68:425-428.
Skaggs DL, Mirzayan R. The posterior fat pad sign in association with occult fracture of the elbow in children. J Bone Joint Surg Am. 1999;81:1429-1433.
Soto F, Fiesseler F, Morales J, et al. Presentation, evaluation, and treatment of clavicle fractures in preschool children presenting to an emergency department. Pediatr Emerg Care. 2009;25:744-747.
675.4 Fractures of Lower Extremity
Femoral Shaft Fractures
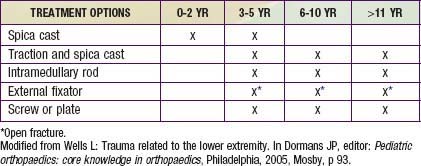
Fractures of the femur in children are common. All age groups, from early childhood to adolescence, can be affected. The mechanism of injury varies from low-energy twisting type injuries to high-velocity injuries in vehicular accidents. Femur fractures in children <2 yr should raise the concern for child abuse. A thorough physical examination is necessary to rule out other injuries and assess the neurovascular status. In the case of high-energy trauma, any signs of hemodynamic instability should prompt the examiner to look for other sources of bleeding. AP and lateral radiographs of the femur demonstrate the fracture. An AP radiograph of the pelvis is obtained to rule out any associated pelvic fracture. Treatment of shaft fractures varies with the age group, as described in Table 675-2.
Triplane and Tillaux Fractures
Triplane and Tillaux fracture patterns occur at the end of the growth period and are based on relative strength of the bone-physis junction and asymmetric closure of the tibial physis. The triplane fractures are so named because the injury has coronal, sagittal, and transverse components (Fig. 675-8). The Tillaux fracture is an avulsion fracture of the anterolateral aspect of the distal tibial epiphysis. Radiographs and further imaging with CT and 3-dimensional reconstructions are necessary to analyze the fracture geometry. The triplane fracture involves the articular surface and hence anatomic reduction is necessary. The reduction is further stabilized with internal fixation. The Tillaux fracture is treated by closed reduction. Open reduction is recommended if a residual intra-articular step off persists.
Boutis K, Willan AR, Babyn P, et al. A randomized, controlled trial of a removable brace versus casting in children with low-risk ankle fractures. Pediatrics. 2007;119:e1256-e1263.
Cummings RJ. Paediatric femoral fracture. Lancet. 2005;365:1116-1117.
Horn DB, Wells L, Tamai J. Lower extremity fractures. In: Dormans JP, editor. The requisites in pediatrics: pediatric orthopaedics and sports medicine. Philadelphia: Mosby; 2005:49-92.
Kim SJ, Shin YW, Yang KH, et al. A multi-center, randomized, clinical study to compare the effect of safety of autologous cultured osteoblast (Ossron) injection to treat fractures. BMC Musculoskel Disorders. 2009;10:20.
Loud KJ, Micheli LJ, Bristol S, et al. Family history predicts stress fracture in active female adolescents. Pediatrics. 2007;120:e364-e372.
Louie KW. Management of open fractures of the lower limb. BMJ. 2009;339:b5092.
Malanga GA, Ramirez-Del Toro JA. Common injuries of the foot and ankle in the child and adolescent athlete. Phys Med Rehab Clin N Am. 2008;19(2):347-371. ix
Wells L, Millman JE. Trauma related to the lower extremity. In: Dormans JP, editor. Pediatric orthopaedics: core knowledge in orthopaedics. Philadelphia: Mosby; 2005:85-115.
Wright JG, Wang EEL, Owen JL, et al. Treatments for paediatric femoral fractures: a randomized trial. Lancet. 2005;365:1153-1162.
675.5 Operative Treatment
Surgical Techniques
The main indications for external fixation are summarized in Table 675-3. The advantages of external fixation include rigid immobilization of the fractures, access to open wounds for continued management, and easier patient mobilization for treatment of other injuries and transportation for diagnostic and therapeutic procedures. The majority of complications with external fixation are pin tract infections, chronic osteomyelitis, and refractures after pin removal.
Table 675-3 COMMON INDICATIONS FOR EXTERNAL FIXATION IN PEDIATRIC FRACTURES
675.6 Complications of Fractures in Children
Lawrence Wells, Kriti Sehgal, and John P. Dormans
The complications specific to children are malalignment and correction by natural growth, physeal arrest, overgrowth, and refracture caused by rapid fracture healing (Table 675-4). The malalignment and late angulation is a common problem with fractures of the proximal tibial metaphysis. The physeal arrest can cause angular deformity or shortening. The angular deformities are treated by hemiepiphysiodesis or osteotomy. The shortening is treated with contralateral leg epiphysiodesis closer to skeletal maturity or lengthening of the short limb. Refractures cause more deformity and can necessitate open reduction. Other complications are reflex sympathetic dystrophy, ligamentous instability, malunion, nonunion, fat embolism, and neurovascular injuries.
Table 675-4 COMPLICATIONS OF FRACTURE
ACUTE
SUBACUTE OR CHRONIC
From Slovis TL, editor: Caffey’s pediatric diagnostic imaging, ed 11, vol 2, Philadelphia, 2008, Mosby, 2008, p 2781.