14 Combinations of Therapy
Introduction
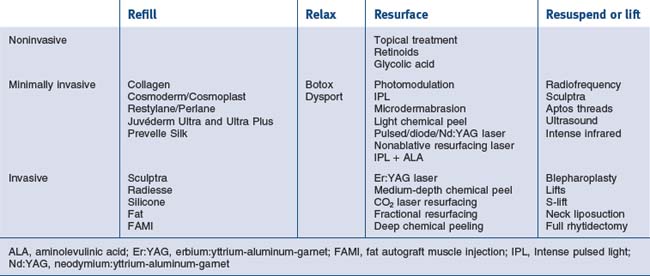
The cosmetic physician’s tools can be divided into the following categories:
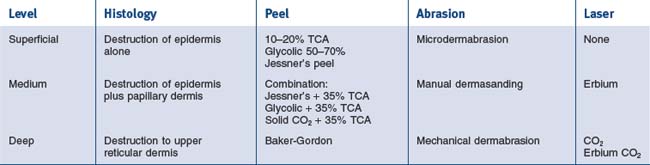
The various regenerative procedures are also classified as to the level of aggressiveness and downtime. They range from ‘lunchtime’ procedures and moderately aggressive procedures to fully aggressive procedures. Each of these also can be chosen for the appropriate patient and even the proper unit area of need. These procedures are outlined in Table 14.1. See also Box 14.1.
Box 14.1
Key features
The Analysis of Skin Types
• Fitzpatrick skin type system
The Fitzpatrick skin type system classifies degrees of pigmentation and ability to tan using grades I to VI. It prognosticates sun sensitivity, susceptibility to photodamage and ability for facultative melanogenesis (one’s intrinsic ability to tan). In addition, this system classifies skin as to its risk factors for complications during chemical peeling or other resurfacing procedures. Fitzpatrick skin types take into account both color and reaction to the sun. Skin types I and II are pale white and freckled with a high degree of potential to burn with sun exposure. Types III and IV can burn but usually are an olive to brown coloration. Types V and VI are dark brown to black skin that rarely ever burn and usually do not need sunscreen protection (Table 14.2).
| Skin type | Color | Reaction to sun |
|---|---|---|
| I | Very white or freckled | Always burns |
| II | White | Usually burns |
| III | White to olive | Sometimes burns |
| IV | Brown | Rarely burns |
| V | Dark brown | Very rarely burns |
| VI | Black | Never burns |
• Glogau system
The Glogau system classifies severity of photodamage, taking into account the degree of epidermal and dermal degenerative effects. The categorization is from I to IV, ranging from mild, through moderate and advanced, to severe photodamaged skin. These categories are devised for therapeutic intervention. Type I in young individuals or minimal degree photodamage should be treated with light chemical peeling and medical treatment. Types II and III would entail medium-depth chemical peeling, while type IV would need those modalities listed plus cosmetic surgical intervention for gravitational changes (Box 14.2). Type III or IV can have combination procedures dependent on the degree of damage in each area.
Box 14.2
Photoaging group – Glogau’s classification
Based on Glogau RG 1994 Chemical peeling and aging skin. Journal of Geriatric Dermatology 2(1):30–35
• Index of photoaging skin
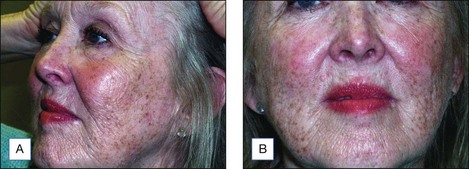
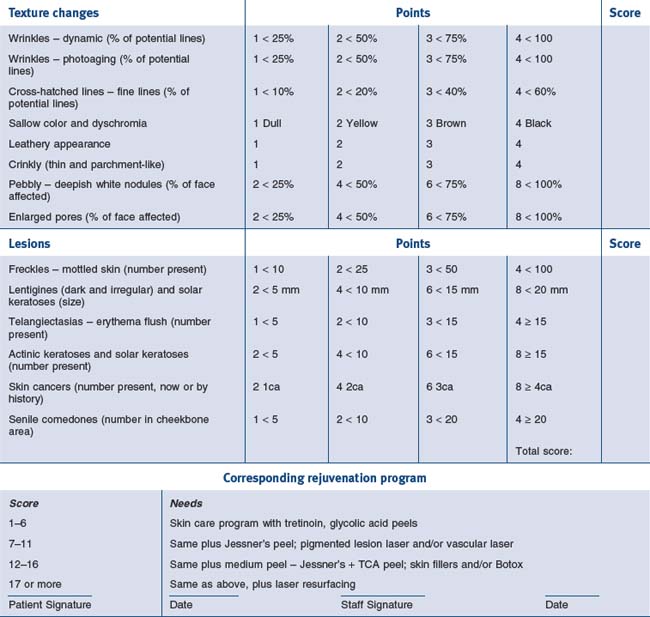
The index of photoaging skin is a system of quantitating photodamage and using numerical scores that would fit into corresponding rejuvenation programs. In analyzing photodamage, the major categories include epidermal color, skin lesions, textural changes, and dermal changes. Photoaging changes include wrinkles, cross-hatched lines, sallow color, leathery appearance, crinkly thin parchment skin, and the pebblish white nodules of milia. Each of these is classified, giving the patient a point score of between one and four. In addition, the number and extent of lesions are categorized from freckles, lentigines, telangiectasias, actinic and seborrheic keratoses, skin cancers, and senile comedones. These are also added in the classification system and the final score results are tabulated. A total score of between one and four indicates very mild damage and the patient would adequately respond to a five-step skin care program including sunscreen protection, retinoic acid, glycolic acid peels and selective lesional removal. A patient scoring between five and nine requires all of the above, plus a repetitive superficial peeling agents program such as glycolic acid, Jessner’s solution or lactic acid peels. A score of 10–14 suggests the inclusion of medium-depth chemical peeling, and if a patient scores 15 or above the practitioner will be including deep peeling or laser resurfacing in the treatment (Figs 14.1 and 14.2). Thus, the patient can understand during the consultation the degree of photodamage and the necessity for an individual peeling program (Table 14.3). The system can also quantitate individual cosmetic units indicating more aggressive resurfacing for the lids and/or lips than surrounding cheeks and forehead.
Types of Combination Chemical Peel
• Superifical chemical peeling
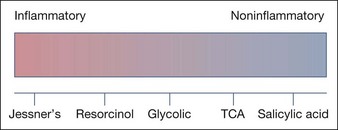
Each of these agents has its own characteristics and methodology and a physician must be thoroughly familiar with the chemicals, methods of application, and the nature of healing. The usual time for healing is from 1 to 4 days depending on the chemical and its strength. These agents range from noninflammatory (salicylic acid peels) to moderately inflammatory (Jessner’s solution) and each has a specific purpose (Fig. 14.3).
Sunscreens are necessary accompaniments to all peeling procedures and the patient should begin this prior to the peel. The proper FDA approved sunscreen should be chosen based on the patient’s skin type and procedure chosen. The choices are UVA filters, UVB filters and inorganic sunscreens (Table 14.4).
| Screens | UV protection (nm) |
|---|---|
| UVB | |
| p-Aminobenzoic acid (PABA) | 260–315 |
| Salicylates | 260–310 |
| Cinnamates | 280–310 |
| UVA | |
| Benzophenones | 270–350 |
| Meradimate | 336 |
| Avobenzone | 310–40 |
| Inorganic screens | |
| Titanium dioxide | 290–360 |
| Zinc oxide | 290–400 |
Light chemical peeling for photoaging changes utilizes the more inflammatory agents such as Jessner’s solution, glycolic acid and TCA (Fig. 14.4). These procedures can all be combined with cosmeceutical agents and even exfoliative procedures such as microdermabrasion. It is also combined with intense pulsed light, photomodulation and selective lasers. The peels will produce epidermal sloughing of various degrees and thus should not be performed on the same day as the other procedures. Separating them by alternating weeks of treatment will allow enough recovery for the combined procedures to be effective.
TCA has been the most versatile of all peeling agents and has been used in concentrations weight-per-volume from 15% to 50%. As concentration increases, ablative injury is greater as well as rejuvenative effects for photoaging skin. In most patients, TCA in concentrations above 25–30% affects the dermis as well as epidermis, having the effect of medium and deeper chemical peels (Fig. 14.5).
• Medium-depth chemical peeling
For many years, 40 to 60% TCA was the prototypical medium-depth peeling agent because of its ability to ameliorate fine wrinkles, actinic changes, and preneoplasia. TCA as a single agent for medium-depth peeling has fallen out of favor because of the high risk of complications, especially scarring and pigmentary alterations, when used in strengths approaching 50% and higher. Today, most medium-depth chemical peels are combination peels performed utilizing 35% TCA in combination with either Jessner’s solution, 70% glycolic acid, or solid carbon dioxide (CO2) as a ‘priming’ agent (Table 14.5). These combination peels have been found to be as effective as 50% TCA alone but with fewer risks. The level of penetration is more easily controlled with these combination peels, thereby preventing the ‘hot spots’ that can produce the dyschromias and scarring seen with higher concentrations of TCA.
| Agent | Comment |
|---|---|
| 40–50% Trichloroacetic acid (TCA) | Not recommended |
| Combination 35% TCA–solid CO2 (Brody) | The most potent combination |
| Combination 35% TCA–Jessner’s (Monheit) | The most popular combination |
| Combination 35% TCA–70% glycolic acid (Coleman) | An effective combination |
| 88% phenol | Rarely used |
The Jessner’s–TCA Peel
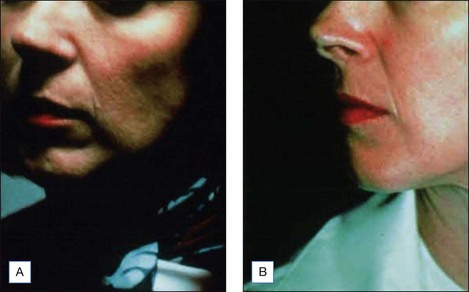
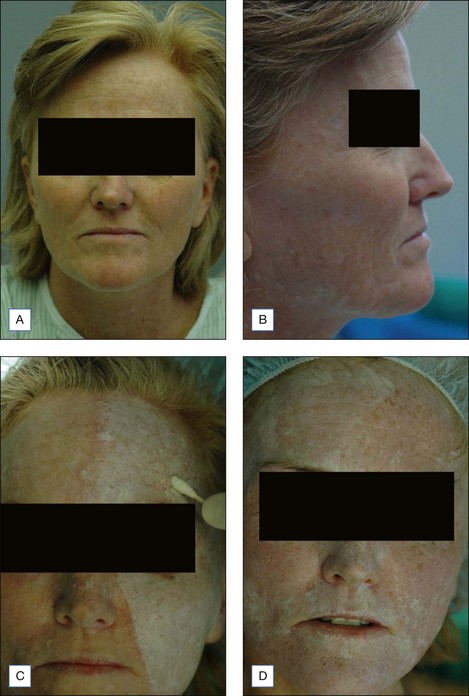
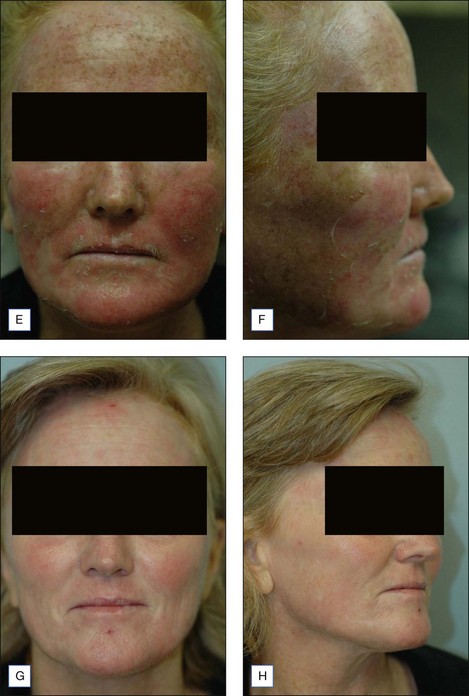
The Jessner’s–35% TCA peel is particularly useful for the improvement of mild to moderate photoaging (Fig. 14.6A). It freshens sallow, atrophic skin and softens fine rhytids, with minimal risk of textural or pigmentary complications. Collagen remodeling occurs for as long as 3 to 4 months postoperatively, during which there is continued improvement in texture and fine rhytides. Deep furrows, however, are not eliminated with this peel. When used in conjunction with a retinoid, bleaching agent, and sunscreens, a single Jessner’s–35% TCA peel lessens pigmentary dyschromias and lentigines more effectively than repetitive superficial peels (Fig. 14.7). Epidermal growths such as actinic keratoses also respond well to this peel. In fact, the Jessner’s–35% TCA peel has been found to be as effective as topical 5-fluorouracil chemotherapy in removing both grossly visible and clinically undetectable actinic keratoses but has the added advantages of lower morbidity and greater improvement in associated photoaging (Fig. 14.8).
The Jessner’s–35% TCA peel is effective in combination to blend the effects of other resurfacing procedures with the surrounding skin. Patients who undergo laser resurfacing, deep chemical peeling or dermabrasion to a localized area such as the periorbital or perioral region often develop a sharp line of demarcation between the treated and untreated skin. The treated skin may appear hypopigmented (also known as pseudohypopigmentation) in comparison to the untreated skin. These irregularities are often conspicuous and are troubling to the patient. A Jessner’s–35% TCA peel performed on the adjacent untreated skin helps to blend the area treated with deep resurfacing with its surroundings. For example, a patient with advanced photoaging in the periorbital region and moderate photoaging on the remaining face may desire CO2 laser resurfacing only around the eyes. In this patient, medium-depth chemical peeling of the areas not treated with the laser would improve the photoaging in these regions and avoid a line of demarcation (see Fig. 14.6B–F). Similarly, a patient having spot dermabrasion to a localized scar would benefit from a Jessner’s–35% TCA peel to the remainder of that cosmetic unit or to the rest of the face. It is important to note that when used in combination with other resurfacing procedures such as laser resurfacing or dermabrasion, the peel should be performed first in order to avoid accidental application of the peeling agent onto previously abraded areas of skin.
• Deep chemical peeling
Phenol Peeling
The application of pure, undiluted, 88% phenol to the skin causes rapid and complete coagulation of epidermal keratin proteins and is thought to block itself from further penetration. Classified as a medium-depth peeling agent, pure phenol is rarely used for chemical peeling because its limited depth of penetration results in a lesser degree of effectiveness. In contrast, the Baker-Gordon peel utilizes phenol in a formulation that permits deeper penetration into the dermis than full-strength phenol. First described in 1961, the Baker-Gordon peel has been used successfully for many years and the formula consists of Septisol (Vestal Laboratories, St. Louis, MO), croton oil, and tap water added to a solution of phenol, reducing its concentration to 50 or 55% (Table 14.6). The mixture of ingredients is freshly prepared and must be stirred vigorously prior to application, owing to its poor miscibility. The liquid soap, Septisol, is a surfactant that reduces skin tension, allowing a more even penetration. Croton oil is a vesicant epidermolytic agent that enhances phenol absorption. Recent investigations into the effects of this peel using varying concentrations of both phenol and croton oil have suggested that the procedure’s efficacy is more related to the amount of croton oil than the concentration of phenol. Modifications of the original Baker-Gordon formula in order to improve the risk to benefit ratio of deep peeling are discussed in depth in Chapter 8.
| 88% liquid phenol, USP (BP) | 3 mL |
| Tap water | 2 mL |
| Septisol liquid soap | 8 drops |
| Croton oil | 3 drops |
Combining Levels of Peel and Other Procedures
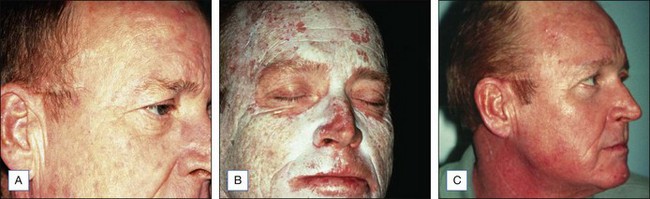
Deep chemical peeling can significantly improve or even eliminate deep furrows as well as other textural and pigmentary irregularities associated with severe photoaging (Fig. 14.9). A remarkable degree of improvement is the expected result of deep chemical peeling when performed properly on carefully selected patients. Combining superficial, medium-depth and deep peeling and/or resurfacing procedures will selectively give the cosmetic unit or area of the body the safest and most effective level of resurfacing (Table 14.7).
• Combining levels of peel
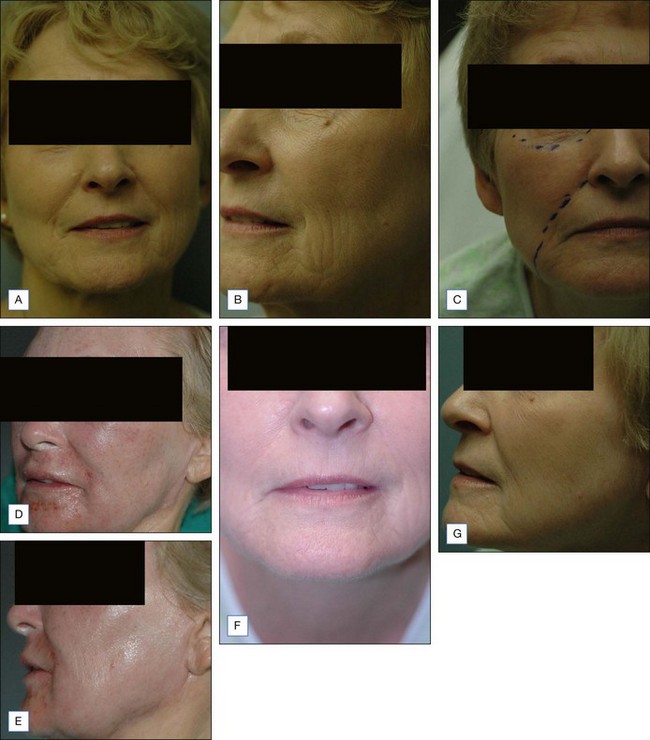
The use of these peel combinations will enhance a monotherapy procedure. An example would be the patient with moderately severe photoaging changes around the periorbital and perioral areas, such as deep wrinkles and crepey eyelid skin and rhagades around the mouth, combined with only moderate photoaging changes around the rest of the face. This would be characterized by epidermal growths, sallow color, and fine lines. This patient would best be treated by CO2 laser resurfacing of the perioral and periorbital areas and with the Jessner’s–35% TCA peel around the rest of the face. A light peel such as the Jessner’s peel alone is also performed from the neck down to the shoulders to further blend the unit areas for a natural result (Fig. 14.10).
• Combining peels with other procedures
Dermasanding/Dermal Sanding and Dermabrasion
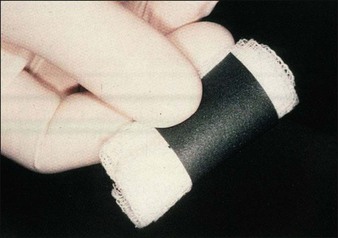
Silicone carbide sandpaper is found at a local hardware store and comes in the following grades (grit): coarse (120–180), medium (220–320) and fine (400). The author only uses medium and fine to further resurface after a chemical peel. The manual dermasanding can take the resurfacing procedure to a greater depth without the risk of further chemical or thermal damage. The sandpaper is cut into 2 cm × 6 cm strips, sterilized in surgical packs, and used individually. They are then rolled around 2″ × 2″ (5 cm2) gauze or tongue blade. The paper is wetted with saline or lidocaine to reduce drag as the skin is stretched and then manually dermasanded (Fig. 14.11). The white frosted skin is removed until fine bleeding points are seen as an endpoint.
Dermasanding is used with medium-depth chemical peeling to remove thick, keratotic lesions not amenable to peel alone. An example is the patient with diffuse, thick seborrheic keratoses with photoaging skin. Such lesions cannot be removed by peel as the only treatment. A medium depth peel is performed first; then, after the skin has frosted appropriately, the keratotic lesions are removed by dermasanding (Fig. 14.12).
Acne scars are best treated with dermabrasion. In many instances, a full-face mechanical dermabrasion is not needed and may be excessive. To simplify the procedure, a medium-depth chemical peel can be performed over the entire face and the scar units can then be resurfaced with dermasanding or dermabrasion. An example is the patient with rolling scars and ice pick scars on the medial cheek. The deepest ice pick scars are treated with punch graft exchange, requiring a dermabrasion for further refinement. The dermabrasion is performed in the mid face only and the medium peel is used over the remaining areas for blending. With this combination, the peel is always performed first and then the dermabrasion follows after frosting has occurred (Fig. 14.13).
CO2 Laser Resurfacing
Combining various resurfacing procedures together with chemical peeling makes both procedures safer, more precise, and tailored for the individual patient; see Table 14.8 for combinations that are recommended.
Table 14.8 Recommended combinations of resurfacing and chemical peeling procedures
| Chemical peeling | Laser | Dermasanding |
|---|---|---|
| Jessner’s + 35% TCA – face | Perioral | Facial borders |
| Jessner’s alone – neck and chest | Periorbital | Upper 1/3 neck Laser skip areas |
Botulinum Toxin and Fillers
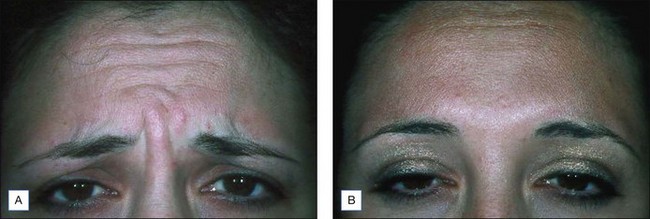
Relaxing spasmodic muscle producing dynamic wrinkles with botulinum toxin is an adjunctive procedure that supplements medium peeling or resurfacing procedures (Fig. 14.14). De-innervating muscles causing frown lines, forehead wrinkles, and crow’s feet prior to peeling and resurfacing procedures will produce a better response than peeling or laser alone. This is because the dynamic wrinkles are put to rest and, as new dermal collagen is formed over the ensuing 4 to 6 months, there is minimal muscle movement to wear down the new collagen as the wrinkles are static. The immediate results appear better than with solely laser treatment as the dynamic folds that do not respond to laser or peel alone will improve, as will the fine lines and crepiness that is response to resurfacing. Similarly, botulinum toxin can be used around the lips to put the dynamic perioral lines to rest during the healing phase of the peel.
Adding volume to atrophic skin improves wrinkles in selective areas, thus making chemical peels more effective. For example, using collagen or hyaluronic acid for lip augmentation makes peeling and/or laser resurfacing for lip rhytids more successful because the increased volume allows a more conservative resurfacing to be effective and produces a more natural result than using a peel alone (Fig. 14.15). Fillers can be used before or after resurfacing depending on the agents used. The author finds long term filling agents (fat; Sculptra (Dermik Aesthetics, Berwyn, PA) or Radiesse (Bioform-Merz Aesthetics, San Mateo, CA)) are best used 1 month to 6 weeks prior to the resurfacing procedure (Fig. 14.16). Temporary fillers such as hyaluronic acid (Restylane (Medicis, Scottsdale, AZ) or Juvéderm (Allergan, Irvine, CA)), along with collagen (Cosmoderm (Allergan, Irvine, CA)), are used after full healing and swelling has resolved to fill out residual wrinkles.
Case Studies
• Case study 1
53-year-old caucasian female with significant photoaging of the skin resulting in diffuse actinic lentigines, actinic keratoses, fine rhytides – both dynamic and static over facial surface areas. She has Fitzpatrick II skin type, Glogau II to III facial aging with a 13 index of photoaging. No prior treatment with no significant contraindications for treatment (Fig. 14.17A–B).
Alt T. Occluded Baker-Gordon chemical peel: review and update. Journal of Dermatologic Surgery and Oncology. 1989;15:980-993.
Alt TH. Technical aids for dermabrasion. Dermatologic Surgery. 2002;28:1115-1119.
Baker TJ, Gordon HL. The ablation of rhytides by chemical means: a preliminary report. Journal of the Florida Medical Association. 1961;48:451-454.
Brody HJ. Variations and comparisons in medium depth chemical peeling. Journal of Dermatologic Surgery and Oncology. 1989;15:953-963.
Brody HJ. Trichloracetic acid application in chemical peeling: operative techniques. Plastic and Reconstructive Surgery. 1995;2(2):127-128.
Brody HJ. Complications of chemical resurfacing. Fundamentals of Cosmetic Surgery. Dermatologic Clinics. 2001;19(3):427-438.
Carruthers J, Carruthers A. Combining botulinum toxin injection and laser for facial rhytides. In: Coleman WP, Lawrence N, editors. Skin resurfacing. Baltimore: Williams and Wilkins; 1998:235-243.
Chiarello SE. Tumescent dermasanding with cryospraying: a new wrinkle on the treatment of rhytids. Dermatologic Surgery. 1996;22(7):601-610.
Coleman WP, Futrell JM. The glycolic acid trichloroacetic acid peel. Journal of Dermatologic Surgery and Oncology. 1994;20:76-80.
Ditre CM, Griffin TD, Murphy GF, et al. Improvement of photodamaged skin with alphahydroxy acid (AHA): a clinical, histologic and ultrastructural study. Journal of the American Academy of Dermatology. 1996;34(2):187-195.
Donofrio LM. Structural lipoaugmentation: a parafacial technique. ournal of Dermatologic Surgery. 2000;26:1129-1134.
Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Archives of Dermatology. 1988;124:869-871.
Glogau RG. Chemical peeling and aging skin. Journal of Geriatric Dermatology. 1994;2(1):30-35.
Glogau R. Photoaging skin course. Washington, DC: Lecture at American Academy of Dermatology; 2004. February 13
Grimes PE. The safety and efficacy of salicylic acid chemical peels in darker racial-ethnic groups. Dermatologic Surgery. 1999;25:18-22.
Hanke CW, Bullock SS. Tretinoin and glycolic acid treatment regimens. Facial Plastic Surgery. 1995;11:9-14.
Harris DR, Noodleman FR. Combining manual dermasanding with low strength trichloroacetic acid to improve actinically injured skin. Journal of Dermatologic Surgery and Oncology. 1994;20:436-442.
Hetter GP. An examination of the phenol-croton oil peel: Part I: Dissecting the formula. Plastic and Reconstructive Surgery. 2000;105:227-239. discussion 49–51
Hetter GP. An examination of the phenol-croton oil peel. Part IV: face peel results with different concentrations of phenol and croton oil. Plastic and Reconstructive Surgery. 2000;105:1061-1083. discussion 84–87
Lim HW, Naylor M, Honigran H, et al. American Academy of Dermatology consensus conference on UVA protection of sunscreens: summary and recommendation. Journal of the American Academy of Dermatology. 2001;44:505-508.
Lowe NJ, et al. Pigmentation of aging skin: evaluation and treatment. In: Lowe N, editor. Textbook of facial rejuvenation. London: Martin Dunitz; 2002:75-79.
McCollough EG, Langsdon PR. Chemical peeling with phenol. In: Roenigk H, Roenigk R, editors. Dermatologic surgery: principles and practice. New York: Marcel Dekker; 1989:997-1016.
Monheit GD. The Jessner’s + TCA peel: a medium depth chemical peel. Journal of Dermatologic Surgery and Oncology. 1989;15:945-950.
Monheit GD. The Jessner’s-TCA peel. Facial Plastic Surgery Clinics of North America. 1994;2:21-27.
Monheit GD. Skin preparation: an essential step before chemical peeling or laser resurfacing. Cosmetic Dermatology. 1996;9:13-14.
Monheit GD. Chemical Peels. In: Rigel DS, editor. Photoaging. New York: Marcel Dekker; 2004:189-190.
Monheit GD, Zeitouni NC. Skin resurfacing for photoaging: laser resurfacing versus chemical peeling. Cosmetic Dermatology. 1997;10:11-22.
Pollack SV. Some new injectable dermal filler materials: hylaform, restylane and artecol. Journal of Cutaneous Medicine and Surgery. 1999;3(suppl 4):29.
Rubin MG. Manual of chemical peels: superficial and medium depth. Philadelphia: JB Lippincott; 1995.
Stegman SJ. A comparative histologic study of the effects of three peeling agents and dermabrasion on normal and sun-damaged skin. Aesthetic Plastic Surgery. 1982;6:123-125.
Timbow K Obata H, Pathak M, Fitzpatrick T. Mechanism of depigmentation by hydroquinone. Journal of Investigative Dermatology. 1974;62:436-449.
Weiss RA, Weiss MA, Beasley KL. Rejuvenation of photoaged skin: 5 year results with IPL. Dermatologic Surgery. 2002;28:1115.
Witheiler DD, Lawrence N, Cox SE, et al. Long-term efficacy and safety of Jessner’s solution and 35% trichloroacetic acid vs 5% fluorouracil in the treatment of widespread facial actinic keratoses. Dermatologic Surgery. 1997;23:191-196.