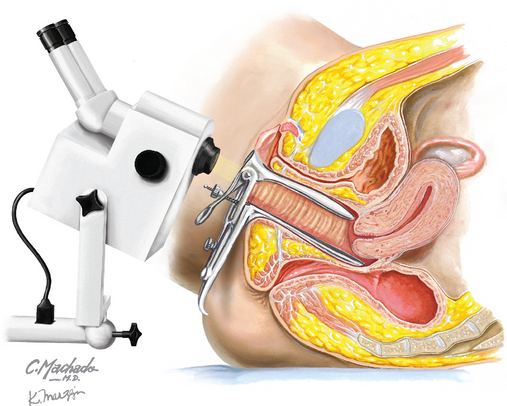
Chapter 238 Colposcopy
REQUIRED EQUIPMENT
Ang MS, Kaufman RH, Adam E, et al. Colposcopically directed biopsy and loop excision of the transformation zone. Comparison of histologic findings. J Reprod Med. 1995;40:167.
Cristoforoni PM, Gerbaldo D, Perino A, et al. Computerized colposcopy: results of a pilot study and analysis of its clinical relevance. Obstet Gynecol. 1995;85:1011.
Gage JC, Hanson VW, Abbey K, et alASCUS LSIL Triage Study (ALTS) Group. Number of cervical biopsies and sensitivity of colposcopy. Obstet Gynecol. 2006;108:264.
Lonky NM, Mann WJ, Massad LS, et al. Ability of visual tests to predict underlying cervical neoplasia. Colposcopy and speculoscopy. J Reprod Med. 1995;40:530.
American College of Obstetricians and Gynecologists. Diagnosis and treatment of cervical carcinomas. ACOG Practice Bulletin 35. Obstet Gynecol. 2002;99:855.
American College of Obstetricians and Gynecologists. Cervical cytology screening. ACOG Practice Bulletin 45. Obstet Gynecol. 2003;102:417.
American College of Obstetricians and Gynecologists. Cervical cancer screening in adolescents. ACOG Committee Opinion 300. Obstet Gynecol. 2004;104:885.
American College of Obstetricians and Gynecologists. Human papillomavirus. ACOG Practice Bulletin 61. Obstet Gynecol. 2005;105:905.
American College of Obstetricians and Gynecologists. Management of abnormal cervical cytology and histology. ACOG Practice Bulletin 66. Obstet Gynecol. 2005;106:645.
American College of Obstetricians and Gynecologists. Evaluation and management of abnormal cervical cytology and histology in the adolescent. ACOG Committee Opinion 330. Obstet Gynecol. 2006;107:963.
Burke L, Antonioli DA, Ducatman BS. Colposcopy: Text and atlas. East Norwalk, Conn: Appleton & Lange, 1991.
Craine BL, Craine ER. Digital imaging colposcopy: basic concepts and applications. Obstet Gynecol. 1993;82:869.
Davis GD. Colposcopic examination of the vagina. Obstet Gynecol Clin North Am. 1993;20:217.
Lau S, Franco EL. Management of low-grade cervical lesions in young women. CMAJ. 2005;173:771.
Rickert VI, Kozlowski KJ, Warren AM, et al. Adolescents and colposcopy: the use of different procedures to reduce anxiety. Am J Obstet Gynecol. 1994;170:504.
Safaeian M, Solomon D, Wacholder S, et al. Risk of precancer and follow-up management strategies for women with human papillomavirus-negative atypical squamous cells of undetermined significance. Obstet Gynecol. 2007;109:1325.
Shafi MI, Dunn JA, Chenoy R, et al. Digital imaging colposcopy, image analysis and quantification of the colposcopic image. Br J Obstet Gynaecol. 1994;101:234.
Wright TCJr, Cox JT, Massad LS, et al. 2001 Consensus Guidelines for the management of women with cervical cytological abnormalities. JAMA. 2002;287:2120.
Wright VC. Understanding the colposcope. Optics, light path, magnification, and field of view. Obstet Gynecol Clin North Am. 1993;20:31.