Colon Repair/Colostomy Creation
The colon is the distal continuation of the gastrointestinal (GI) tract, extending from the ileocecal valve to the distal anal canal. It measures 4.5 to 6 feet in length and functions to reabsorb sodium and water and to provide temporary storage for enteric wastes.
Operating on the colon mandates knowledge of its segmental blood supply. The right colon is supplied by the ileocolic and right colic branches of the superior mesenteric artery. The hepatic flexure to midtransverse colon is supplied by the middle colic artery. The distal transverse, splenic flexure, and descending and sigmoid colon are perfused by the left colic and sigmoidal branches of the inferior mesenteric artery. The region of the splenic flexure is known as a “watershed” area of marginal arterial supply, requiring extra caution during surgery. In addition, the ascending and descending colon have retroperitoneal attachments that must be divided during mobilization.
Areas of the colon most susceptible to injury during gynecologic procedures are the cecum, the sigmoid colon, and the rectum. Primary repair of injuries to the cecum and proximal sigmoid colon without prior bowel preparation can be performed if soilage is minimal and the mesentery is not involved. Seemingly minor injuries to the mesentery can result in delayed ischemia with transmural infarction and perforation of the affected segment. In addition, there should be no hemodynamic shock or more than 1 L of blood loss from the primary procedure. The repair is performed in a manner similar to that previously described for small bowel injuries—interrupted 3-0 silk suture closure in a transverse fashion so as not to encroach on the lumen. Copious field irrigation with normal saline should follow. A 5% to 7% incidence of postoperative localized abscess is reported. This is often amenable to percutaneous drainage.
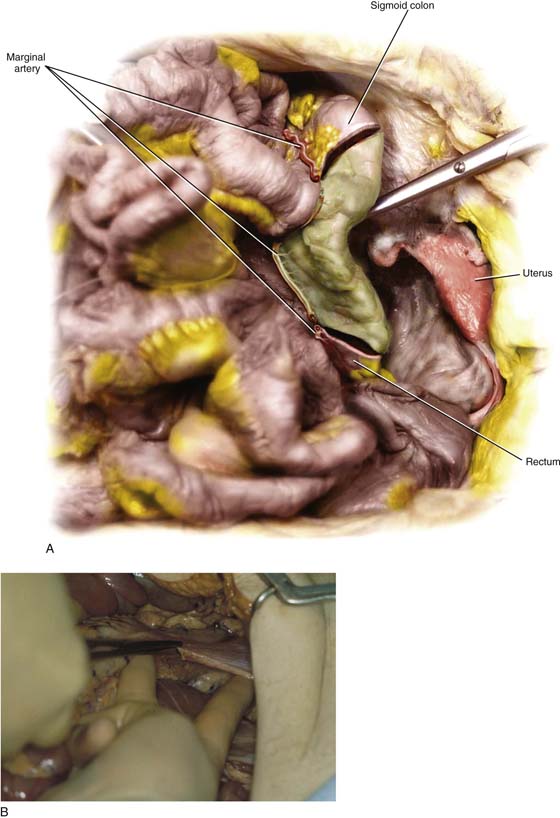
Injuries of the distal sigmoid colon and rectum without previous bowel preparation are best treated with repair of the injury as described, but with proximal division of the colon and end sigmoid colostomy construction. If the injury involves the mesentery and there is a question of bowel viability, it is always safest to divide the colon distal to the point of injury using a gastrointestinal anastomosis (GIA) stapling device (Fig. 98–1A). Then, the proximal limb is brought out through the abdominal wall as a colostomy. Some degree of judgment is required in managing these injuries, and when available, an experienced general surgeon’s assistance should be obtained.
Performance of sigmoid colostomy begins with adequate exposure. Lower abdominal transverse incisions often do not permit adequate visualization for colonic mobilization. If the real possibility of requiring a postoperative colostomy exists, a midline or midabdominal transverse incision is more desirable and permits the use of a larger retractor such as a Buchwalter or Balfour device. The small bowel is carefully packed off to the right side and moved with a wide Deaver retractor. The sigmoid colon is then grasped and retracted medially, exposing the lateral retroperitoneal attachments. The membrane (“white line”) of Toldt is incised along the length of the descending colon down to the level of the pelvic brim. Once the white line is incised, further lengthwise dissection can often be carried out bluntly with the fingers (Fig. 98–1B). Care must be taken to visualize the path of the ureter during all parts of the dissection; it is usually found medial and posterior to the colon. In addition, it is important to locate and preserve the nutrient vessels within the colonic mesentery. The left colic and sigmoidal branches of the inferior mesenteric artery are necessary for colonic function and healing.
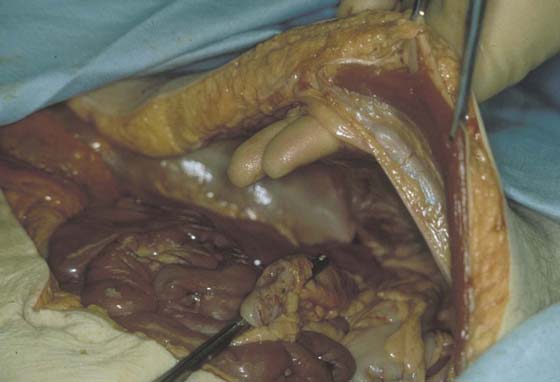
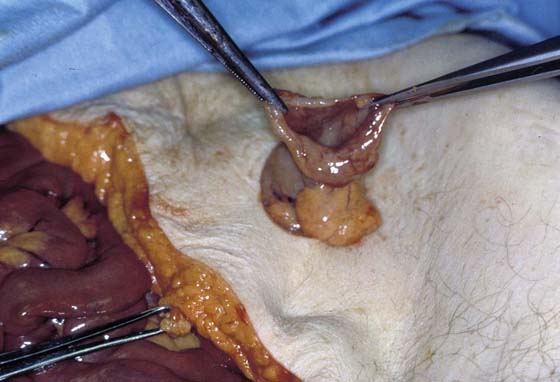
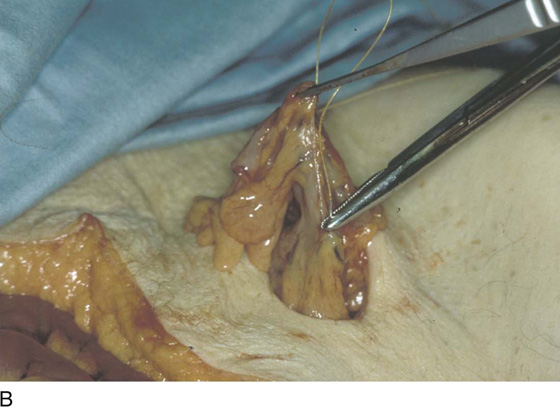
Depending upon the location of the injury, the colon should be divided distal to the left colic artery to ensure good perfusion to the stoma. The location of division is chosen, and a rent is created between the colon wall and the mesentery large enough to admit the GIA stapling device (Fig. 98–2). The stapler is then fired, resulting in division of the colon. The distal end is dropped into the pelvis. Further mobility of the proximal sigmoid is gained by scoring the peritoneum of the mesentery on both medial and lateral sides parallel to the length of the colon. Gentle blunt dissection with a sponge stick while upward retraction is applied to the colon should increase usable length. Care is taken not to avulse major mesenteric nutrient vessels. Small mesenteric bleeders may be controlled with electrocautery or suture ligation. Once sufficient length is gained so as to easily reach the anterior abdominal wall, an exit site is chosen. Traversal of the lateral rectus sheath just below or above the umbilicus is preferred because of a lower incidence of subsequent peristomal herniation. The skin is grasped with an Allis clamp (Fig. 98–3), and a circular wound is created (Fig. 98–4). The rectus fascia is incised in a cruciate fashion so as to admit two fingers snugly (Fig. 98–5). The proximal stapled end of the colon is then grasped with a Babcock clamp through the stoma site and is brought out through the fascial defect. The clamp is left on while the primary incision is closed to prevent retraction of the colon back into the peritoneal cavity. There should be enough redundancy so the colonic staple line extends several centimeters above the skin level with minimal tension. With the primary wound now closed and protected, the stoma is “matured” by sharply excising the staple line to open the colonic lumen (Fig. 98–6). Mucosal bleeding should be evident; if brisk, it is controlled with pinpoint electrocautery. A 3-0 absorbable suture is then used to circumferentially evert the colonic stoma. This is best performed in an interrupted fashion by a generous mucosal/serosal “bite” at the cut edge (Fig. 98–7A) and another smaller serosal bite 3 cm proximal with the needle (Fig. 98–7B). A small skin edge is then included, and the knot is tied (Fig. 98–7C). The finished result should be as shown with no exposed mesentery (Fig. 98–8). A lubricated finger should easily pass through the fascial portion of the stoma lumen. An ostomy appliance is then applied.
FIGURE 98–1 A. Injury to the sigmoid mesocolon can lead to devascularization of the large intestine (sigmoid colon). Here the marginal branches of one of the sigmoid branches of the inferior mesenteric vessels were disrupted, leading to complete necrosis and perforation of a segment of the sigmoid colon. B. The sigmoid colon is visible to the left of the scissors. The lateral peritoneal attachments are sharply incised while the colon is reflected medially.
FIGURE 98–2 The gastrointestinal anastomosis (GIA) 75-mm stapling device is used to divide the colon proximal to the injury. The mesenteric edge of the colon is cleared to admit the stapler.
FIGURE 98–3 The site for stoma placement is chosen. Often this can be marked preoperatively by the institution’s enterostomal therapist if a colostomy is planned. A site at the lateral aspect of the rectus sheath traversing both anterior and posterior layers is best.
FIGURE 98–4 A 3-cm circular ellipse of skin and subcutaneous fat is excised down to the level of the anterior fascia.
FIGURE 98–5 A cruciform incision is made in the anterior and posterior fascia through which two fingers may fit snugly.
FIGURE 98–6 The proximal colonic staple line is grasped with a Babcock clamp and brought through the abdominal wall. Once the surgical incision is closed, the colon is opened.
FIGURE 98–7 The stoma is matured by interrupted circumferential 3-0 absorbable sutures encompassing the cut edge (A), a 3-cm proximal serosal bite (B), and the skin edge (C).
FIGURE 98–8 Finished stoma shown with everted colonic wall and central lumen.

 David J. Lamon
David J. Lamon