21 Coagulopathy
Hemostasis is a dynamic and highly complex process typically divided into two components: primary and secondary. Primary hemostasis refers to the blood vessel and platelet response, whereas secondary hemostasis refers to the protein response (clotting cascade). In reality, both primary and secondary hemostasis are tightly interconnected, feed back on each other, and operate in unison. Nevertheless, from a conceptual standpoint, it is helpful to consider each limb of hemostasis separately. In this chapter, we review the clotting mechanism. The reader is referred to Chapter 20 for a discussion of the most common coagulation disorder in the ICU: thrombocytopenia.
 General Principles
General Principles
The blood clotting cascade is highly complex, consisting of a series of linked reactions. In each reaction, a serine protease, once activated, is capable of activating its downstream substrate. For the purposes of this chapter, the scheme will be simplified according to the following themes: (1) the final step in the clotting cascade is the conversion of fibrinogen to fibrin, a process mediated by thrombin; (2) fibrin is the “glue” that holds platelet plugs together and contributes to the host defense against pathogens; (3) there are two pathways—extrinsic and intrinsic—that converge to induce thrombin generation and fibrin formation; (4) blood coagulation is always initiated by the extrinsic pathway (via tissue factor) and amplified by the intrinsic pathway; (5) the prothrombin time (PT) measures the integrity of the extrinsic (and common) pathways, and the activated partial thromboplastin time (APTT) measures the integrity of the intrinsic (and common) pathways; and (6) every procoagulant step is balanced by a natural anticoagulant (antithrombin, protein C system, tissue factor pathway inhibitor). In the final analysis, hemostasis represents a balance between anticoagulant and procoagulant forces.1–5
Disorders in hemostasis occur when the hemostatic balance shifts toward one side or the other, resulting in one of two clinical phenotypes: bleeding or thrombosis. The myriad causes, diagnostic workup, and treatment of coagulation disorders are beyond the scope of this chapter. In the sections that follow, we consider the coagulopathy that occurs in patients with sepsis. The reasons for choosing sepsis as the case study are several-fold: (1) sepsis is common in the ICU and is responsible for most coagulation disorders; (2) a consideration of the mechanisms, diagnosis, and therapy of coagulopathy in this setting may be widely applicable to other conditions also associated with activation of the innate immune response (e.g., trauma, burns, postoperative systemic inflammatory response syndrome) and (3) recent therapeutic breakthroughs emphasize the importance of targeting the host response rather than the clotting cascade per se. In sepsis, hemostasis derangement is characterized by enhanced fibrin formation and dysfunction of the physiologic anticoagulant response, with depression of fibrinolysis and impaired fibrin removal.2,4
 Incidence
Incidence
Previous studies demonstrated that the coagulation system is activated in virtually all patients with severe sepsis.2–4 In most such patients, activation may be minimal and detected only by test findings such as elevated circulating D-dimer levels,6 low protein C levels, or antithrombin deficiency.4,6 The activation also may be pronounced and characterized by the presence of thrombocytopenia or even disseminated intravascular coagulation (DIC), with evidence of both thrombosis and bleeding. It is estimated that DIC occurs in 15% to 30% of patients with severe sepsis or septic shock.2,4,7,8
 Mechanisms
Mechanisms
In sepsis, the clotting cascade is initiated by tissue factor (TF). When TF is exposed to blood, it binds to factor VII. The complex TF-FVIIa activates factor X, which in turn forms a prothrombinase complex, leading to the generation of thrombin. Finally, thrombin converts fibrinogen into fibrin. TF is exposed to blood through either endothelial disruption or expression on the surface of circulating monocytes, tissue macrophages, and even endothelial cells.4,9,10
At the same time, sepsis attenuates all three physiologic anticoagulant mechanisms: activated protein C (APC), antithrombin (AT) and tissue factor pathway inhibitor (TFPI). APC has a key role in sepsis; along with protein S and thrombomodulin, it degrades factors V and VIII by a process accelerated by endothelial protein C receptors (EPCR). In sepsis, APC, protein S, thrombomodulin, and EPCR are down-regulated, rendering the system ineffective.11,12 AT is the main inhibitor of thrombin and factor Xa, whereas TFPI inhibits the TF-FVIIa complex. Levels of both AT and TFPI are markedly reduced in patients with sepsis.4,13,14 Sepsis also inhibits fibrinolysis.2,4 Together, these changes tilt the balance toward the procoagulant side, resulting in thrombin generation, fibrin deposition, and consumption of clotting factors and platelets. DIC represents the extreme case in this pathophysiologic continuum.2–4
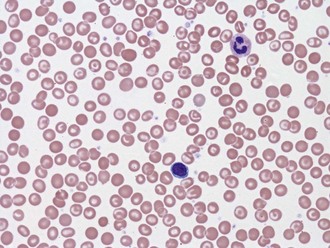
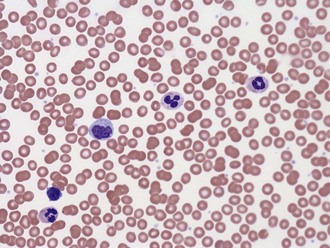
Local activation of the coagulation system in sepsis is an integral component of the innate immune response and may play a protective role in walling off infection. However, in patients with severe sepsis, systemic activation of coagulation is harmful to the patient and associated with increased mortality.15 Other common forms of coagulopathy in the ICU are associated with severe trauma, massive blood losses, and shock. Recent studies suggest that early trauma-associated coagulopathy is triggered mainly by shock, mediated by activated protein C, and exacerbated by dilution of plasma and hypothermia.16,17 Interestingly, the early trauma-associated hypercoagulable state converts to a hypercoagulable one by 24 hours after trauma, carrying a higher risk of thrombotic complications.18 Other common coagulopathies in the ICU are caused by liver dysfunction, heparin and other anticoagulant medications, and vitamin K deficiency (Figures 21-1 and 21-2).
 Clinical Manifestations and Diagnosis
Clinical Manifestations and Diagnosis
Severe sepsis is usually associated with a net procoagulant state, as evidenced by local or diffuse microvascular thrombi. These changes occasionally manifest as skin lesions, as occurs in purpura fulminans. More commonly, the coagulation cascade interacts with the inflammatory pathway to induce endothelial cell activation and secondary dysfunction of internal organs, including the liver, kidneys, lungs, and brain. Patients are at risk for bleeding when the consumption of clotting factors outstrips the production. Bleeding is more common when the coagulopathy is exacerbated by concomitant thrombocytopenia, liver disease, heparin use, and invasive procedures. In large prospective studies, the incidence of serious bleeding in patients with severe sepsis varies between 2% and 6%.19 The most sensitive laboratory markers of sepsis-associated coagulopathy include reduced circulating protein C levels and increased circulating D-dimer levels. However, protein C levels are not routinely measured, and an elevated level of D-dimers is a nonspecific finding. In general, coagulation factor levels are inversely correlated with the severity of sepsis,2 except for factor VIII, an acute-phase protein. Fibrinogen, another acute-phase protein, may be elevated in the early stages of sepsis but is reduced in up to 50% of patients with severe sepsis.20
Marked activation of coagulation and secondary consumption of clotting factors may lead to DIC. No single test is sufficiently sensitive or specific to make the diagnosis of DIC. Recently a scoring system was proposed that employs simple laboratory tests, including platelet count, elevated fibrin-related marker (e.g., soluble fibrin monomers, fibrin degradation products), prolonged PT, and fibrinogen level.20,21 Other markers of coagulation activation such as thrombin-antithrombin complexes, fibrinopeptides, and prothrombin fragment 1.2 are considered investigational in this setting.
The PT or APTT may be elevated for reasons other than sepsis-associated consumption of clotting factors (Box 21-1). As a general rule, increased clotting times are caused by inhibitors against one or more clotting factors or a congenital or acquired deficiency state. In the ICU, prolongation of the PT or APTT is almost always related to an acquired deficiency state. An isolated increase in PT indicates factor VII (extrinsic pathway) deficiency and may be seen in early liver failure or during the initial stages of warfarin (Coumadin) therapy. An isolated increase in the APTT points to a defect in the intrinsic pathway—namely, factors XII, XI, IX, or VIII. An increase in both PT and APTT reflects an abnormality in the common pathway (factors X or V, prothrombin, or fibrinogen) or a combined deficiency in the extrinsic and intrinsic pathways. The latter occurs with heparin therapy, long-term warfarin treatment, vitamin K deficiency, advanced liver disease, DIC, or dilutional coagulopathy.3,4
 Prognosis
Prognosis
Certain markers of coagulation activation have been correlated with negative outcome in patients with sepsis. For example, low antithrombin levels in patients with sepsis are predictive of poor survival.7 Decreased protein C levels in severe sepsis have been shown to correlate with mortality, presence of shock, length of ICU stay, and ventilator dependence.2,4 In clinical studies of multiple organ dysfunction, maximum PT and APTT were shown to be longer in nonsurvivors than in survivors.15 DIC is an independent predictor for mortality in patients with sepsis.22
 Treatment
Treatment
The consumption of clotting factors and platelets, with or without DIC, may result in bleeding diathesis in patients with sepsis. For such patients, transfusion therapy with platelets, fresh frozen plasma, or plasma components may be indicated if the patient is actively bleeding or if there is a high risk of bleeding (e.g., due to other types of coagulopathy, trauma, need for surgery, invasive procedures).2,4,16
In view of recent advances in our understanding of the underlying pathophysiology of sepsis, emphasis has shifted from procoagulant replacement to anticoagulant therapy. A variety of thrombin inhibitors have been tested in patients with sepsis, including antithrombin (AT), tissue factor pathway inhibitor (TFPI) and activated protein C (APC). These drugs inhibit thrombin generation and fibrin formation and demonstrated promising results in animal and early-phase clinical studies.23,24 One possible explanation for these results is that the natural anticoagulants have a dual function: inhibition of coagulation and suppression of inflammation. AT, TFI and APC each have been shown to modulate the inflammatory response under in vitro and in vivo conditions.25
However, in subsequent large, randomized controlled trials, infusions with AT and TFPI (tifacogin) failed to improve 28-day all-cause mortality in patients with severe sepsis.7,26,27 In contrast, the PROWESS study, which was stopped ahead of time, demonstrated that recombinant human activated protein C had both anticoagulant and antiinflammatory properties and improved survival of patients with severe sepsis.6 Recombinant APC is approved for use in the United States and most of the world; its use is an integral part of many guidelines for the treatment of sepsis.28 Recombinant APC’s role in sepsis, however, continues to be debated following publication of negative trials.29,30 Furthermore, we do not know at present whether the different outcomes in the phase 3 trials of AT, TFPI, and APC can be explained by differences in study design or whether they reflect differences at the mechanistic level.
Aird WC. Vascular bed–specific hemostasis: Role of endothelium in sepsis pathogenesis. Crit Care Med. 2001;29(Suppl. 7):S28-S35.
Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344(10):699-709.
Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010;38(Suppl):S26-S34.
This is an excellent review of inflammation and coagulation, particularly in sepsis.
Taylor FBJr, Toh CH, Hoots WK, et al. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86(5):1327-1330.
A remarkable paper introducing the definition and diagnostic criteria for DIC.
1 Rice TW, Wheeler AP. Coagulopathy in critically ill patients. Chest. 2009;136:1622-1630.
2 Levi M. The coagulant response in sepsis. Clin Chest Med. 2008;29:627-642.
3 Levi M, Opal SM. Coagulation abnormalities in critically ill patients. Crit Care. 2006;10:222-230.
4 Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010;38(Suppl):S26-S34.
5 Aird WC. Vascular bed-specific hemostasis: Role of endothelium in sepsis pathogenesis. Crit Care Med. 2001;29:S28-S35.
6 Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344:699-709.
7 Afshari A, Wetterslev J, Brok J, Moller A. Antithrombin III in critically ill patients: systematic review with meta-analysis and trial sequential analysis. BMJ. 2007;335:1248-1251.
8 Fisher CJJr, Agosti JM, Opal SM, et al. Treatment of septic shock with the tumor necrosis factor receptor: Fc fusion protein. The Soluble TNF Receptor Sepsis Study Group. N Engl J Med. 1996;334:1697-1702.
9 Mandal SK, Pendurthi UR, Rao LV. Cellular localization and trafficking of tissue factor. Blood. 2006;107(12):4746-4753.
10 Panes O, Matus V, Saez CG, et al. Human platelets synthesize and express functional tissue factor. Blood. 2007;109(12):5242-5250.
11 Faust SN, Levin M, Harrison OB, et al. Dysfunction of endothelial protein C activation in severe meningococcal sepsis. N Engl J Med. 2001;345:408-416.
12 Levi M, van der Poll T. Recombinant human activated protein C: Current insights into its mechanism of action. Crit Care. 2007;11(Suppl 5):S3.
13 de Jonge E, Dekkers PE, Creasey AA, et al. Tissue factor pathway inhibitor (TFPI) dose-dependently inhibits coagulation activation without influencing the fibrinolytic and cytokine response during human endotoxemia. Blood. 2000;95:1124-1129.
14 Gando S, Kameue T, Morimoto Y, et al. Tissue factor production not balanced by tissue factor pathway inhibitor in sepsis promotes poor prognosis. Crit Care Med. 2002;30:1729-1734.
15 MacLeod JB, Lynn M, McKenney MG, et al. Early coagulopathy predicts mortality in trauma. J Trauma. 2003;55:39-44.
16 Nascimento B, Callum J, Rubenfeld G, Rezende Netto JB, Lin Y, Rizoli S. Fresh frozen plasma in massive bleedings: more questions than answers. Crit Care. 2010;14:202-209.
17 Hess JR, Brohi K, Dutton RP, Hauser CJ, et al. The Coagulopathy of trauma: a review of mechanisms. J Trauma. 2008;65:748-754.
18 Selby R, Geerts W, Ofosu FA, et al. Hypercoagulability after trauma: hemostatic changes and relationship to venous thromboembolism. Thromb Res. 2008;124:281-287.
19 Bernard GR, Ely EW, Wright TJ, et al. Safety and dose relationship of recombinant human activated protein C for coagulopathy in severe sepsis. Crit Care Med. 2001;29:2051-2059.
20 Wheeler AP, Rice TW. Coagulopathy in critically ill patients: part 2—soluble clotting factors and hemostatic testing. Chest. 2010;137:185-194.
21 Taylor FBJr, Toh CH, Hoots WK, et al. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86:1327-1330.
22 Dhainaut JF, Yan SB, Joyce DE, et al. Treatment effects of drotrecogin alfa (activated) in patients with severe sepsis with or without overt disseminated intravascular coagulation. J Thromb Haemost. 2004;2:1924-1933.
23 Esmon CT. Introduction: Are natural anticoagulants candidates for modulating the inflammatory response to endotoxin? Blood. 2000;95:1113-1116.
24 Minnema MC, Chang AC, Jansen PM, et al. Recombinant human antithrombin III improves survival and attenuates inflammatory responses in baboons lethally challenged with Escherichia coli. Blood. 2000;95:1117-1123.
25 Levi M, van der Poll T. The role of natural anticoagulants in the pathogenesis and management of systemic activation of coagulation and inflammation in critically ill patients. Semin Thromb Hemost. 2008;34:459-468.
26 Warren BL, Eid A, Singer P, et al. Caring for the critically ill patient: High-dose antithrombin III in severe sepsis: A randomized controlled trial. JAMA. 2001;286:1869-1878.
27 Abraham E, Reinhart K, Opal S, et al. Efficacy and safety of tifacogin (recombinant tissue factor pathway inhibitor) in severe sepsis: a randomized controlled trial. JAMA. 2003;290:238-247.
28 Levi M. Activated protein C in sepsis: A critical review. Curr Opin Hematol. 2008;15:481-486.
29 Wiedermann CJ, Kaneider NC. A meta-analysis of controlled trials of recombinant human activated protein C therapy in patients with sepsis. BMC Emerg Med. 2005;5:7.
30 Marti-Carvajal A, Salanti G, Cardona AF. Human recombinant activated protein C for severe sepsis. Cochrane Database Syst Rev 2007;CD004388.