CHAPTER 22 Cloaca
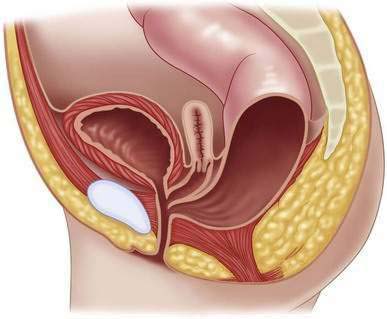
Step 1: Surgical Anatomy
Classification
Step 2: Preoperative Considerations
Management of Cloacal Malformations During the Neonatal Period
Associated Defects
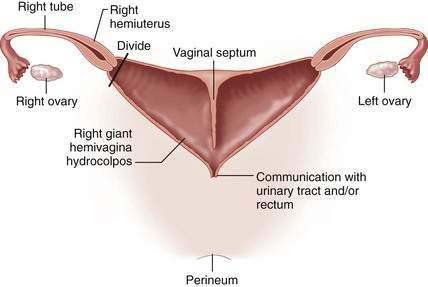
Müllerian Anomalies
Cloacagram
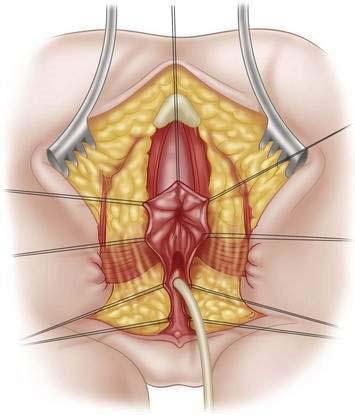
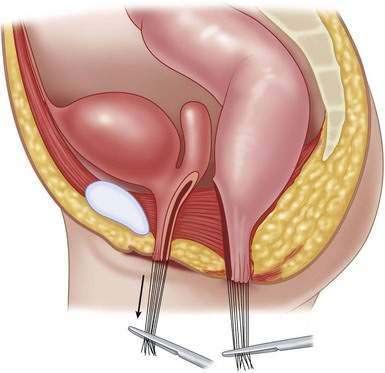
Step 3: Operative Steps
Endoscopy
| GROUP A | GROUP B | |
|---|---|---|
| Common channel | <3 cm | >3 cm |
| Type of operation | Posterior sagittal approach alone | Posterior sagittal and laparotomy |
| Length of procedure | 3 hours | 6-12 hours |
| Hospitalization | 48 hours | Several days |
| Associated urologic defects | 59% | 91% |
| Incidence in our series | 62% | 38% |
| Voluntary bowel movements | 68% | 44% |
| Urinary continence | 72% | 28% |
| Average number of operations* | 9 | 18 |
| Intraoperative decision-making | Relatively easy, reproducible operation | Complex, delicate, technically demanding** |
* Including orthopedic, urologic, cardiac, and general
** Bladder vagina separation, ureteral catheterization, ureteral re-implantation, vesicostomy, cystostomy, bladder neck reconstruction or closure, vaginal switch, vaginal replacement, (using rectum, colon, small bowel)
Colostomy
Drainage of the Hydrocolpos
Definitive Repair
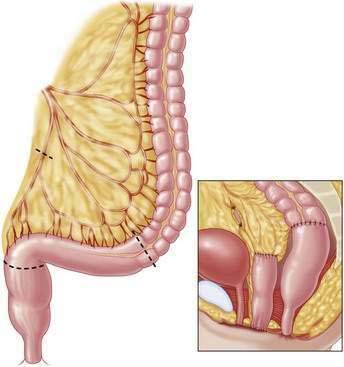
Cloacas with Common Channel Shorter Than 3 cm
Cloacas with a Common Channel Longer Than 3 cm
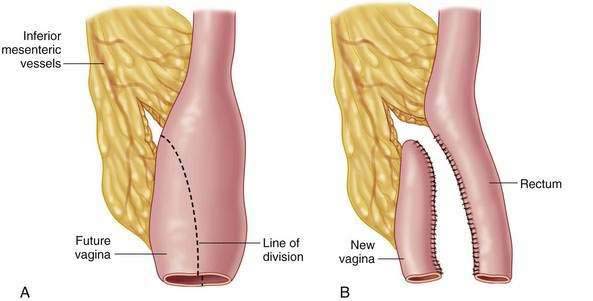
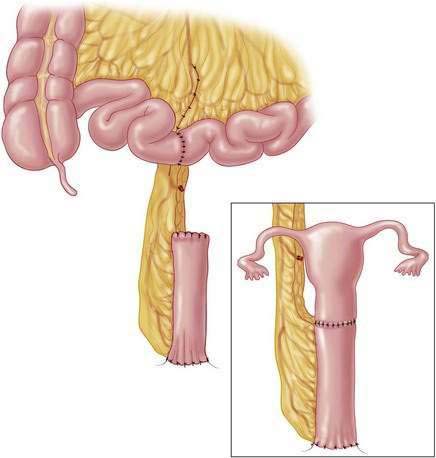
Vaginal Replacement
Rectum
Colon
Small Bowel
Vaginal Switch Maneuver
Very High Cloaca
Step 4: Postoperative Care
Postoperative Management and Colostomy Closure
Outcome
Step 5: Pearls and Pitfalls
Belizon A, Levitt MA, Shoshany G, et al. Rectal prolapse following posterior sagittal anorectoplasty for anorectal malformations. J Pediatr Surg. 2005;40:192-196.
Bianchi DW, Crombleholme TM, D’Alton ME. Cloacal exstrophy. In Fetology: Diagnosis and management of the fetal patient, 2nd ed. New York: McGraw-Hill, 2010, pp 459-466.
Levitt MA, Mak GA, Falcone RA, Peña A. Cloacal exstrophy—pull through or permanent stoma? A review of 53 patients. J Pediatr Surg. 2008;43(1):164-168.
Levitt MA, Peña A. Cloacal malformations: lessons learned from 490 cases. Semin Pediatr Surg. 2010;19:128-138.
Levitt MA, Peña A. Pitfalls in the management of newborn cloacas. Pediatr Surg Int. 2005;21(4):264-269.
Levitt MA, Stein DM, Peña A. Gynecological concerns in the treatment of teenagers with cloaca. J Pediatr Surg. 1998;33(2):188-193.
Livingston J, Elicevik M, Crombleholme T, et al. Prenatal diagnosis of persistent cloaca: a 10 year review. Am J Obstet Gynecol. 2006;195(6):S63.
Peña A. Total urogenital mobilization: an easier way to repair cloacas. J Pediatr Surg. 1997;32(2):263-268.
Peña A, Levitt MA. Neurogenic bladder and anorectal malformations. In: Esposito C, Guys JM, Gough D, Savanelli A, editors. Pediatric neurogenic bladder dysfunction. Berlin: Springer; 2006:85-88.
Rosen NG, Hong AR, Soffer SZ, et al. Recto-vaginal fistula: a common diagnostic error with significant consequences in female patients with anorectal malformations. J Pediatr Surg. 2002;7(7):961-965.