Chapter 5 Clinical skills for preparation of the patient and clinical environment
 Infection control is essential to ensure that the environment is safe and clean for patients and staff at all times.
Infection control is essential to ensure that the environment is safe and clean for patients and staff at all times. Record keeping is needed to provide a continuation of care for the patients during their stay or treatment within the clinical environment where a number of professionals and individuals are involved at different times.
Record keeping is needed to provide a continuation of care for the patients during their stay or treatment within the clinical environment where a number of professionals and individuals are involved at different times.INTRODUCTION
Great importance must be put on the maintenance of a safe and clean clinical environment for the patients. Within the diagnostic imaging department it should be recognised that all patients have the potential to carry and transmit organisms. It has been shown that nosocomial infections (those occurring in a hospital setting) can be reduced considerably with the introduction of basic hygiene procedures.1 In order to prevent the transfer of infections it is important to be aware of the specific organisms that can cause infection and the mode of transfer so that the cycle of replication can be disrupted.
DISEASES AND ORGANISMS
A disease is a condition causing symptoms of an illness, which occurs when cells or molecules within the body stop functioning properly. For example, a disease can be caused through aging, the effects of chemicals, or arise from gene mutation/alteration.
BACTERIA
CROSS-INFECTION
Therefore, it is essential that the equipment, environment and healthcare professional are subject to varying levels of cleanliness dependent on the clinical requirement (Table 5.1). There arethree main levels of cleanliness that exist with regards to equipment and surfaces: clean, disinfected and sterilised.
Table 5.1 The purpose and contraindications of cleansing agents
| Cleaning agents | Purpose in department | Contraindications for use |
|---|---|---|
| Chlorhexidine gluconate solution 2.5% | For cleansing the skin prior to a procedure | Not for hard surfaces |
| Chlorhexidine gluconate 0.015%, cetrimide 0.15% (e.g. Savlon/Tisept/Sterets) |
STERILE SUPPLIES PACKAGING
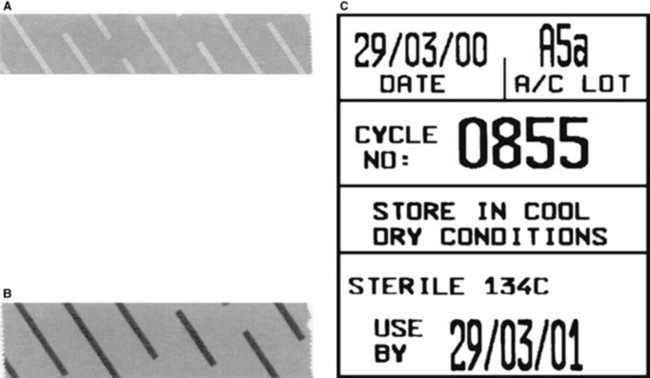
In order for the healthcare professional to know whether a set of instruments is sterile there are indicators on the outer packaging, which must be intact (Fig. 5.1).
Specialised tape will seal the package. Non heat treated CSSD tape will have diagonal white lines: heat treated and therefore sterile tape will have black diagonal lines. A label will also indicate the date and cycle number of sterilisation (Fig. 5.2).
IMAGING EQUIPMENT CLEANING
The used gowns and bed linen must be collected and sent to the laundry in the appropriate coloured linen bag. A white plastic or terylene/polyester bag is used for routine linen that is not fouled or infected. Any linen which is heavilysoiled with blood, faeces, urine or other bodily fluids should be placed in a sealed red water-soluble bag covered with an outer red plastic or terylene/polyester bag.2
Research has shown up to one third of nosocomial infections may be prevented by adequate cleaning of hospital equipment.3 Within the diagnostic imaging department the equipment most commonly in contact with the patient is an image receptor; that is, a cassette or digital device. These should be wiped clean after each patient using alcohol or bactericide impregnated wipes. There should also be a protocol in place for regular and frequent cleaning of all equipment within the X-ray room to reduce risk of infection. It is not only the patient contact surfaces which require regular cleaning but also those operated by the practitioner. The control panel and X-ray tube controls are also at risk of harbouring bacteria from the operator and contact with the patient and therefore would also benefit from frequent cleaning using alcohol or bactericide impregnated wipes.
PERSONAL HYGIENE
The following aspects of personal hygiene must be observed:
HAND WASHING
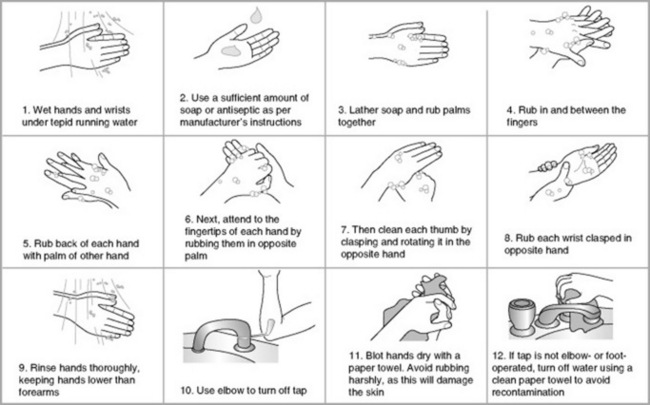
There are three levels of hand washing (Fig. 5.3):
2 Antiseptic/hygienic hand washing
The purpose of this method is also to reduce the risk of transmission of infection. This is known as a basic or 20 second hand wash. It involves washing with antiseptic followed by an alcohol rub, which will remove transient microorganisms and reduce residents.
ASEPTIC TECHNIQUE
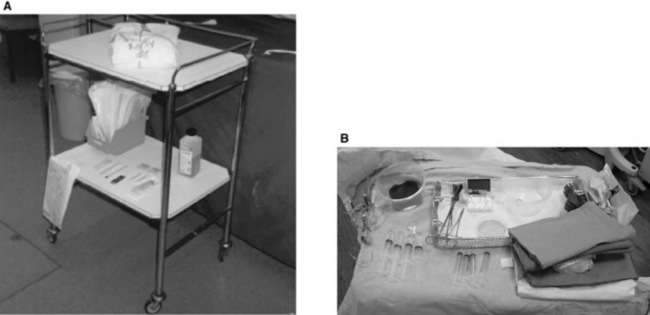
Within an imaging department an aseptic technique may be required for dressing following the insertion of a drainage tube or during a specialised procedure such as a biopsy. Initially, in order to set up the sterile trolley it is necessary to carry out a basic hand wash. The trolley shelves should then be wiped down with a hard surface disinfectant before any items are placed on it. The individual setting up the trolley should then stock the trolley with the following, ensuring that the items are in date and sterile where appropriate (Fig. 5.4):
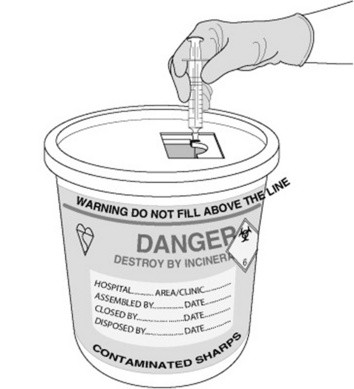
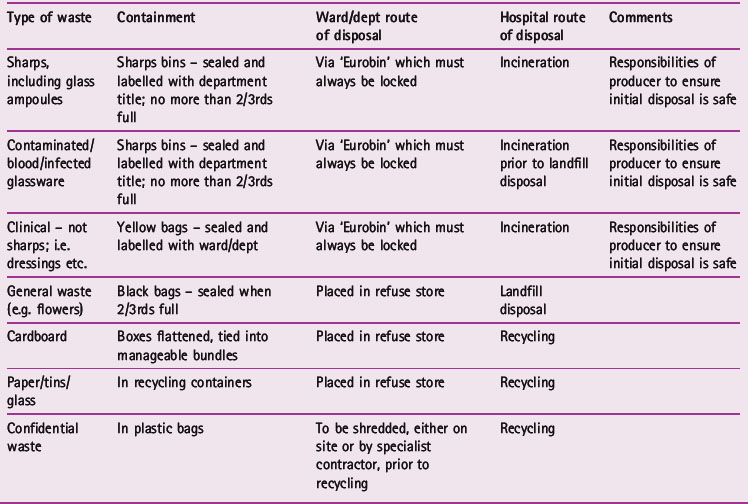
Following completion of the procedure all used objects should be either disposed of in the correct receptacle or returned to the sterile supplies department for re-sterilisation and re-issue (Table 5.2).
FLUOROSCOPIC EXAMINATION PREPARATION
PREPARATION FOR CYSTOGRAPHY
SPECIALIST PROCEDURE PREPARATION
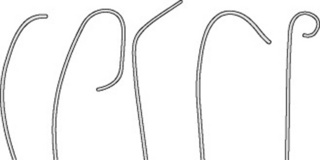
A range of specialist procedures are carried out within a diagnostic imaging department, from angiography to embolisation. The trolley setting should be adapted to the size required for the procedure. There are many different catheters that might be required during the course of the special procedure and the relevant one should be selected prior to its commencement (Fig. 5.6).
The patient will probably be an inpatient due to the requirement for sedation and possible surgical intervention, dependant on the outcome of the procedure. In this instance, the patient’s identification needs to be checked against the wristband as well as asked verbally. The special procedures require informed consent from the patient, which should be obtained by the practitioner or radiologist performing the examination. It is possible that postoperative observations of pulse; respiration, blood pressure and angiopuncture site will be required.
RECORD KEEPING
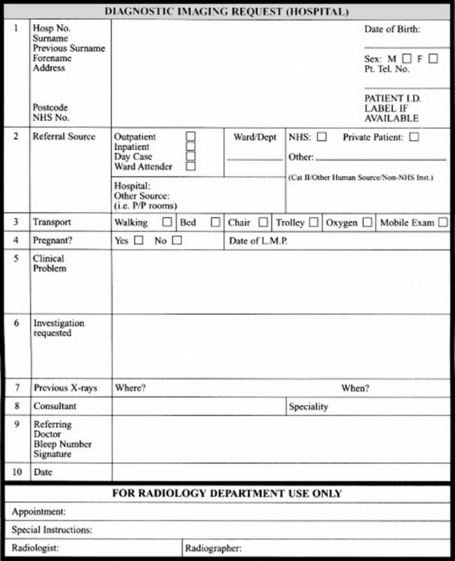
Records within a diagnostic imaging department can range from a request card to observation sheets and accident forms. Record keeping is an integral part of the healthcare professional’s practice as identified by the Health Professionals Council 2003.5
In today’s litigious society any record can be called upon during criminal procedures, Trust investigations and professional disciplinary investigations. The most common faults in record keeping are failure to document an incident or recording inaccurate accounts of events.6
REQUEST CARD
1 Pittet D. Compliance with hand disinfection and its impact on hospital-acquired infections. J Hosp Infect. 2000;48:541-546.
2 NHS Executive. Hospital laundry arrangements for used and infected linen. HSG(95)18. London: NHS Executive, 1995.
3 Schabrun S, Chipcase L. Healthcare equipment as a source of nosocomial infection: a systematic review. J Hosp Infect. 2006;63:239-245.
4 Society and College of Radiographers. Health care associated infections (HCAIs): practical guidance and advice. Society and College of Radiographers, 2006.
5 Health Professionals Council. Standards for conduct, performance and ethics. London: Health Professionals Council, 2003.
6 Dimond B. Legal aspects of documentation. Exploring common deficiencies that occur in record keeping. Br J Nurs. 2005;14(10):568-571.
Recommended reading/bibliography
Ayliffe GA, Babb JR, Quoraishi AH. A test for hygienic hand disinfection. J Clin Pathol. 1978;31:923.
Culmer P. Chesneys’ care of the patient in diagnostic radiography. Oxford: Blackwell, 1995.
Department of Health. The NHS healthcare cleaning manual. London: DoH Publications, 2004.
Lawrence JC. The bacteriology of burns. J Hosp Infect. 1985;6(Suppl B):3.