CHAPTER 1 Clinical Examination and Imaging of the Hip
HISTORY AND PHYSICAL EXAMINATION
History
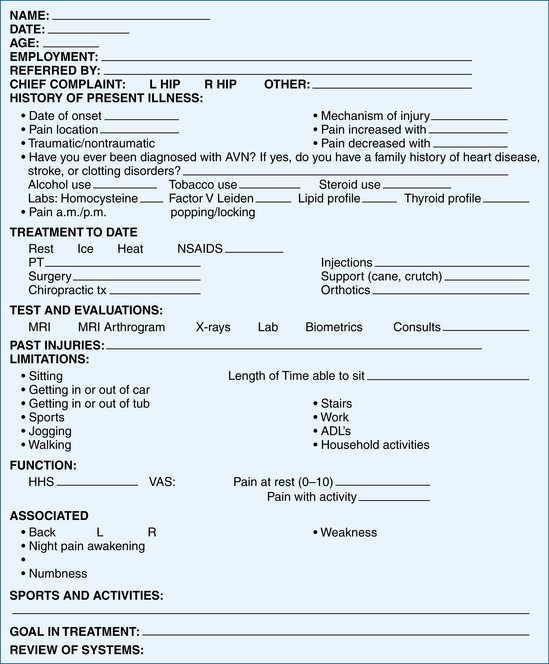
The location of the presenting pain and presence or absence of popping will aid in the determination of intra-articular versus extra-articular causes. Participation in sports and other activities are documented, which can help determine the type of injury. Rotation sports, such as golf, tennis, ballet, and martial arts, have been commonly associated with injuries to the intra-articular structures. Finally, treatment goals and expectations are reviewed with the patient. Treatment may vary, based on the patient’s expectations and postoperative goals. See Figure 1-1 for an illustration of a form for a complete review of the history.
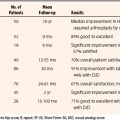
A modified Harris hip or Merle d’Aubigné (MDA) score is a general guide to establish the gross levels of function. The modified Harris hip score (HHS) is the most documented and standardized functional score to date, which is a quantitative score based on pain and function. However, the high-performing athletic population may be best evaluated by the athletic hip score.1 Other hip scores have been outlined with quantifications for more specific patient populations, such as the nonarthritic hip score (NAHS), hip disability and osteoarthritis outcome score (HOOS), musculoskeletal function assessment (MFA), short form 36 (SF-36), and the Western Ontario and McMaster University (WOMAC) osteoarthritis index.2 Currently, the MAHORN (Multicenter Arthroscopy of the Hip Outcomes Research Network) Group is in the final stages of testing the hip outcomes score (HOS), which will provide an internationally accepted score and be useful for the athletic population.3
Physical Examination
The hip assumes an essential role in most activities. The hip is not only responsible for distributing weight between the appendicular and axial skeleton, but is also the joint from which motion is initiated and executed. It is known that the forces through the hip joint can reach three to five times the body’s weight during running and jumping.4 Hip pain often stems from some type of sports-related injury.1 Of athletic injuries in children, 10% to 24% are hip-related, whereas 5% to 6% of adult sports injuries originate in the hip and pelvis.5 Athletes participating in rugby and martial arts have also been reported to have an increased incidence of degenerative hip disease.6 Currently, 60% of intra-articular disorders are initially misdiagnosed.7 An organized physical examination will help in the diagnosis of hip problems.
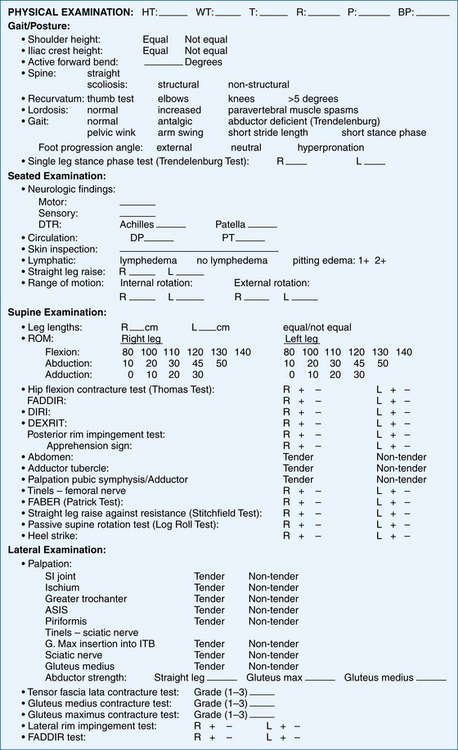
A consistent hip examination is performed quickly and efficiently to screen the hip, back, and abdominal, neurovascular, and neurologic systems and to find the comorbidities that coexist with complex hip pathology. Each examination or physical evaluation has a specific method of being performed, although interobserver consistency and practice is one of the most important aspects of the evaluation.8
The technique of physical examination is dependent on the examiner’s experience and efficiency. The most efficient order of examination begins with standing tests followed by seated, supine, and lateral tests, ending with prone tests.9,10 The physical examination will be fine-tuned and directed through the review of the history of present illness. As with other extremity examinations, access for exposure and patient comfort with loose-fitting clothes about the waist are helpful. An assistant to record the examination on a standardized written form aids in accurate documentation and thoroughness, especially when first starting a comprehensive hip evaluation.
Standing Examination
As the patient stands (Table 1-1), a general point of pain is noted with one finger, and can usually help direct the examination. The groin region directs a suspicion of intra-articular problem and lateral-based pain is primarily associated with intra- or extra-articular aspects. A characteristic sign of patients with intra-articular hip pain is the C sign.8 The patient will hold his or her hand in the shape of a C and place it above the greater trochanter, with the thumb positioned posterior to the trochanter and fingers extending into the groin. This finding can be misinterpreted as lateral soft tissue pathology, such as trochanteric bursitis or the iliotibial band; however, the patient is often describing deep interior hip pain.8 Posterior-superior pain requires a thorough evaluation in differentiating hip and back pain. The shoulder height and iliac crest heights are noted to evaluate leg length discrepancies (Fig. 1-2). Incremental wooden blocks placed under the short side heel help in orthotic considerations. General body habitus is assessed and issues of ligamentous laxity are determined by the middle finger test or hyperextension of the elbows or knees. Structural versus nonstructural scoliosis is differentiated by forward bending and the degree of lumbar flexion is recorded. Side-bending ROM is also useful.
| Examination | Assessment and Association |
|---|---|
| Abductor deficient gait | Abductor strength, proprioception mechanism |
| Antalgic | Trauma, fracture, synovial inflammation |
| Pelvic rotational wink | Intra-articular pathology, hip flexion contracture, increased femoral anteversion, anterior capsual laxity |
| Foot progression angle with excessive external rotation | Femoral retroversion, increased acetabular anteversion, torsional abnormalities, effusion, ligamentous injury |
| Foot progression angle with excessive internal rotation | Increased femoral anteversion or acetabular retroversion, torsional abnormalities |
| Short leg limp | Iliotibial band pathology, true-false leg length discrepancy |
| Single-leg stance phase test | Abductor strength, proprioception mechanism |
| Spinal alignment | Shoulder–iliac crest heights, lordosis, scoliosis, leg length |
| Laxity | Ligamentous laxity in other joints: thumb, elbows, shoulders, or knee |
See video for performing seated examination tests.
Gait abnormalities often help detect hip pathology.11,12 Joint stability, preservation of the labrum and articular cartilage, and proper functioning of the hip joint involve three biomechanical planes of the femur and acetabulum. These relationships are important for the transfer of dynamic and static load to the ligamentous and osseous structures.
Noting iliac crest rotation and terminal hip extension assesses pelvic rotation. On average, a normal gait requires 6 to 8 degrees of hip rotation and 7 degrees of pelvic rotation, for a total rotation of 15 degrees.12 The pelvic wink is demonstrated by an excessive rotation in the axial plane toward the affected hip, thus producing extension and rotation through the lumbar spine, to obtain terminal hip extension. This winking gait can be associated with intra-articular hip pathology, laxity, or hip flexion contractures, especially when combined with increased lumbar lordosis or a forward-stooping posture. Gait changes can affect spinal mechanics and function. Excessive femoral anteversion, or retroversion, can affect a wink on terminal hip extension because the patient will try to create greater anterior coverage with a rotated pelvis. Injury to the anterior capsule can also contribute to a winking gait.
During the stance phase, body weight must be supported by a single leg, with the gluteus maximus, medius, and minimus providing most of the force.12 Maximum ground reactive force occurs on heel strike at 30 degrees of hip flexion. A shortened stance phase can be indicative of neuromuscular abnormalities, trauma, or leg length discrepancies. The abductor deficient gait (Trendelenburg gait or abductor lurch) is an unbalanced stance phase attributed to abductor weakness or proprioception disruption. This pattern may present in two ways—with a shift of the pelvis away from the body (a dropping out of the hip on the affected side), or with a shift of the weight over the adducted leg (a shift of the upper body over the top of the affected hip). The antalgic gait is characterized by a shortened stance phase on the painful side, limiting the duration of weight-bearing (a self-protecting limp caused by pain). A short leg gait is noted by drop of the shoulder in the direction of the short leg.
In addition to body habitus and gait evaluation, the single-leg stance phase test (Trendelenburg test) is performed during the standing evaluation of the hip. The single-leg stance phase test is performed on both legs, with the nonaffected leg examined first, to establish a baseline (Fig. 1-3). During this test, the examiner stands behind the exposed patient (to the degree that the bony landmarks are easily observed). The patient stands with the feet shoulder width apart and then brings one leg forward by flexing the leg to 45 degrees at the hip and 45 degrees at the knee, thereby simulating the single-leg stance phase with the load on the examined hip. This position is held for 6 seconds. As the patient lifts and holds one foot off the ground, the contralateral hip abductor musculature and neural loop of proprioception are being tested. The pelvis will tilt toward or away from the unsupported side if the musculature is weak or if the neural loop of proprioception is disrupted. Normal dynamic midstance translocation is 2 cm during a normal gait pattern12; a shift in either direction of more than 2 cm constitutes a positive shift. This test is also performed in a dynamic fashion by some examiners.
Seated Examination
The seated hip examination (Table 1-2) consists of a thorough neurologic and vascular examination. The need to check the basics is obvious, even in apparently healthy individuals. The posterior tibial pulse is checked first, any swelling of the extremity is noted, and inspection of the skin is performed at this time. A straight leg raise test is then performed by passively extending the knee into full extension. The straight leg raise test is helpful for detecting radicular neurologic symptoms.
| Examination | Assessment and Association |
|---|---|
| Neurologic | Sensory nerves originating from the L2-S1 levels, deep tendon reflex of patella (L2-L4 spinal nerves and femoral nerve) and Achilles (L5-S1 sacral nerves) |
| Straight leg raise | Radicular neurologic symptoms |
| Vascular | Pulses of the dorsalis pedis and posterior tibial artery |
| Lymphatics | Skin inspection for swelling, scarring, or side to side asymmetry |
| Internal rotation | Normal between 20 and 35 degrees |
| External rotation | Normal between 30 and 45 degrees |
See video for performing seated examination tests.
The loss of internal rotation is one of the first signs of an intra-articular disorder; therefore, one of the most important assessments is internal and external rotation in the seated position. The seated position ensures that the ischium is square to the table, thus providing sufficient stability at 90 degrees of hip flexion and a reproducible platform for accurate rotational measurement. Passive internal and external rotation testing are performed gently and compared from side to side. Seated rotation range of motion is also compared and contrasted with the extended position of the hip (Fig. 1-4).
Musculotendinous, ligamentous, and osseous control of internal and external rotation are complex, so any differences in seated versus extended positions may raise the question of ligamentous versus osseous abnormality. Sufficient internal rotation is important for proper hip function—there should be at least 10 degrees of internal rotation at the midstance phase of normal gait,12 but less than 20 degrees is abnormal (see Table 1-3 for normal ROM). Pathology related to femoroacetabular impingement or to rotational constraint from increased or decreased femoral or acetabular anteversion can result in significant side-to-side differences. An increased internal rotation combined with a decreased external rotation may indicate excessive femoral anteversion and distinguished from hip capsular pathology by radiographic and biometric assessment.
Supine Examination
A battery of tests with the patient in the supine position (Table 1-4) helps distinguish internal from extra-articular sources of hip symptoms further. The supine examination begins with the assessment of leg lengths. Next, passive hip flexion range of motion is assessed (Table 1-3). Both knees are brought up to the chest and the degree of flexion is recorded (Fig. 1-5). It is important to note the pelvic position because the hip may stop early in flexion, with the end range of motion being predominantly pelvic rotation. From this position, the hip flexion contracture test (Thomas test) is performed by having the patient extend and relax one leg down toward the table (Fig. 1-6). Any lack of terminal extension, noted by the inability of the thigh to reach the table, demonstrates a hip flexion contracture. Both sides are examined for comparison. An important aspect of this test is to obtain the zero set point for the lumbar spine. Patients with hyperlaxity or connective tissue disorders could have a false-negative result. In these patients, the zero set point can be established with an abdominal contraction. The hip flexion contracture test could also be falsely negative if there is lumbar spine hyperlordosis.
| Examination | Assessment and Association |
|---|---|
| Range of motion | Flexion, abduction, adduction |
| FADDIR | Anterior femoroacetabular impingement, torn labrum |
| Hip flexion contracture test (Thomas test) | Hip flexor contracture (psoas), femoral neuropathy, intra-articular pathology, abdominal cause |
| FABER (Flexion, Abduction, External Rotation) | Distinguish between back and hip pathology, specifically sacroiliac joint pathology |
| Dynamic internal rotatory impingement test (similar to McCarthy test) | Anterior femoroacetabular impingement, torn labrum |
| Dynamic external rotatory impingement test (similar to McCarthy test) | Superior femoroacetabular impingement, torn labrum |
| Posterior rim impingement test | Posterior femoroacetabular impingement, torn labrum |
| Passive supine rotation test (log roll) | Trauma, effusion, synovitis |
| Heel strike | Trauma, femoral fracture |
| Straight leg raise against resistance (Stinchfield) | Intraarticular pathology along with psoas tendonitis or bursitis. Hip flexor strength |
| Palpation | |
See video for performing supine examination tests.
TABLE 1-3 Normal Internal and External Rotation Range of Motion
| Range of Motion Assessment | Normal (degrees) | Abnormal (degrees) |
|---|---|---|
| Seated internal rotation | 20-35 | <20 |
| Seated external rotation | 30-45 | <30 |
| Extended internal rotation | 20-35 | <20 |
| Extended external rotation | 30-45 | <30 |
| Supine hip flexion | 100-110 | <100 |
| Adduction | 20-30 | <20 |
| Abduction | 45 | <45 |
The FABER test, conventionally known as the Patrick test, is helpful in determining hip versus lumbar complaints (Fig. 1-7). Re-creation of hip pain can be associated with musculotendinous or osseous posterior lateral acetabular incongruence or ligamentous injury. In cases of a coup-contrecoup injury, in which the mechanism of injury is initiated posteriorly, pain will be secondarily referred to anteriorly.
For the DIRI test, the patient is in the supine position and instructed to hold the nonaffected leg in flexion beyond 90 degrees, thus establishing a zero pelvic set point and eliminating lumbar lordosis. The examined hip is then brought into 90 degrees of flexion or beyond and is passively taken through a wide arc of adduction and internal rotation (Fig. 1-8). A positive result is noted with re-creation of the complaint pain. DIRI can also be performed in the operating room for direct visualization of femoral neck and acetabular congruence (video).

FIGURE 1-8 Dynamic internal rotatory impingement (DIRI) test. A, DIRI begins with the hip at 90 degrees flexion or beyond. B, It is then passively taken through a wide arc of adduction and internal rotation (arrows) while decreasing flexion to about 80 degrees.
For the DEXRIT test, the patient is in the supine position and instructed to hold the nonaffected leg in flexion beyond 90 degrees, thus eliminating lumbar lordosis. The hip is then brought into 90 degrees flexion or beyond and dynamically taken through a wide arc of abduction and external rotation (Fig. 1-9). A positive result is noted with re-creation of pain. DEXRIT can be performed intraoperatively for direct visualization of femoral neck and acetabular congruence (video).
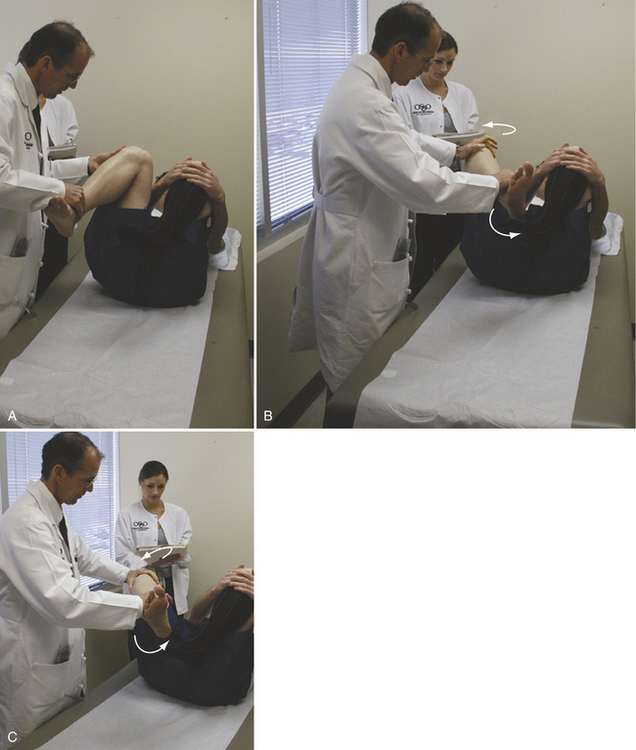
FIGURE 1-9 The dynamic external rotatory impingement test (DEXRIT). A, DEXRIT begins with the hip at 90 degrees flexion or beyond. B, C, It is then dynamically taken through a wide arc of abduction and external rotation (arrows).
Passive abduction and adduction range of motion are assessed in the supine position (see Table 1-3). Palpation of the abdomen is performed and any tenderness is documented (Fig. 1-10). Abdominal tenderness is differentiated from fascial hernia and/or adductor tendinitis. Resisted torso flexion with palpation of the abdomen will differentiate the fascial hernia from other complaints. Palpation of the adductor tubercle with active testing will detect adductor tendonitis. Common physical examination findings associated with athletic pubalgia include inguinal canal tenderness, pubic crest-tubercle tenderness, adductor origin tenderness, pain with resisted sit-ups or hip flexion, and a tender, dilated superficial ring.
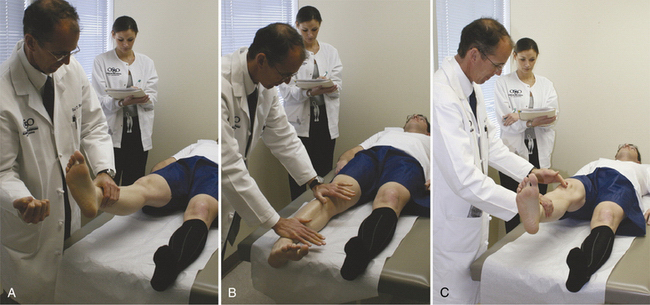
Other useful tests may include Tinel’s test of the femoral nerve. This test is found to be positive with hip flexion contractures of more than 25 degrees as a result of the proximity of the psoas tendon and femoral nerve. A heel strike is performed by striking the heel abruptly. A positive response is indicative of trauma or a stress fracture (Fig. 1-11A). The passive supine rotation test (log roll) involves passive internal and external rotation of the femur, with the leg lying in an extended or slightly flexed position (see Fig. 1-11B). The passive supine rotation test is performed bilaterally and any side to side differences in this maneuver can alert the examiner to the presence of laxity, effusion, or internal derangement. The straight leg raise against resistance test (Stinchfield test) is an assessment of hip flexor and psoas strength and is a sign of an intra-articular problem as the psoas places pressure on the labrum. The patient performs an active straight leg raise, with the knee in extension up to 45 degrees; the examiner’s hand is then placed distal to the knee while applying a downward force (see Fig. 1-11C). A positive test is noted with re-creation of the complaint, pain, or weakness.
The importance of multiple examinations is recognized for the detection of intra-articular pathology. Even in the presence of normal internal and external rotation, there is a need for further delineation of the relationships that exist among the musculotendinous, osseous, and ligamentous structures. Tests for impingement can have good specificity and reasonable predictive value for osseous abnormalities; however, no single test is sensitive enough to be used exclusively. Furthermore, the ligamentous contribution to range of motion varies with flexion and rotation.13
The posterior rim impingement test can also be performed in the supine position. The patient is positioned at the edge of the examining table so that the examined leg hangs freely at the hip and the patient draws up both legs in to the chest, eliminating lumbar lordosis. The affected leg is then extended off the table, allowing for full extension of the hip, abducted and externally rotated (Fig. 1-12). The posterior rim impingement test takes the hip into extension and assesses the congruence of the posterior acetabular wall and femoral neck. A variation of this test is the lateral rim impingement test (see next section).
Lateral Examination
The lateral examination (Table 1-5) begins with the patient on the contralateral side and palpating the areas of the suprasacroiliac and sacroiliac (SI) joint, muscles of abduction, and origin of the gluteus maximus as it inserts along the lateral border of the sacrum and the most posterior aspect of the ilium. The next point of palpation is the ischium for detection of avulsions or bursitis. Finally, the piriformis and sciatic nerve are palpated for any signs of tenderness, along with the abductor musculature, which includes the glutei (maximus, medius, and minimus) and tensor fascia lata. An active piriformis test is performed by the patient pushing the heel down into the table, abducting and externally rotating the leg against resistance, while the examiner monitors the piriformis (Fig. 1-13). The active piriformis test is similar to Pace’s sign, which is pain and weakness on resisted abduction and external rotation of the thigh in the seated position.14 A set of passive adduction tests (similar to Ober’s test) are performed with the leg in three positions (Fig. 1-14)—extension (tensor fascia lata contracture test), neutral (gluteus medius contracture test), and flexion (gluteus maximus contracture test). Gluteus medius tension is assessed by relaxation of the iliotibial band with knee flexion. In this position, the hip should adduct down toward the table. Any restrictions of these motions are recorded. When performing the gluteus maximus contracture test, the shoulder is rotated toward the side of the table, with the hip flexed and knee extended. If adduction cannot occur in this position, the gluteus maximus portion is contracted. The hip should freely be able to come into a full adducted position and any restriction of the gluteus maximus is recognized. The gluteus maximus is balanced with the tensor fascia lata anteriorly. If the hip does not come beyond the midline in the longitudinal axis of the torso, it is graded as a 3+ restriction above torso, 2+ restriction at the midline, and 1+ restriction below. A clear delineation of the exact area of restriction will help direct physical therapy and peritrochanteric treatment options. Strength is assessed with any type of lateral-based hip complaint. The gluteus medius strength test is performed with the knee in flexion (Fig. 1-15) to release the iliotibial band contribution.
| Examination | Assessment and Association |
|---|---|
| Flexion, adduction, internal rotation | Anterior femoroacetabular impingement, torn labrum |
| Lateral rim impingement | Lateral femoroacetabular impingement, torn labrum, instability |
| Tensor fascia lata contracture test (Ober test) | Tensor fascia lata contracture |
| Gluteus medius contracture test (Ober test) | Gluteus medius contracture, tear (decreased strength with knee flexion, suspect tear) |
| Gluteus maximus contracture test | Gluteus maximus contracture, contribution to iliotibial band |
| Palpation | |
See video.
Next is the passive FADDIR assessment, which is performed in a dynamic manner (Fig. 1-16). The examiner holds the monitoring hand in and about the superior aspect of the hip with the lower leg cradled on the forearm and the knee on the hand. The hip is then brought into flexion, adduction, and internal rotation. Any reproduction of the patient’s complaint and the degree of impingement are noted. FADDIR is commonly performed as part of the supine assessment.15 The difference is the position of the pelvis. The supine position eliminates lumbar lordosis, whereas the lateral tests the normal dynamic pelvic inclination. Pelvic inclination may affect testing and both positions are helpful in evaluation.
The lateral rim impingement Test is performed with the hip passively abducted and externally rotated (Fig. 1-17). The examiner cradles the patient’s lower leg with one arm and monitors the hip joint with the opposing hand. The examiner passively brings the affected hip through a wide arc from flexion to extension in continuous abduction while externally rotating the hip. Reproduction of the patient’s pain is scored positive. If the feeling of guarding or instability is present, the test is positive for apprehension, which is not to be confused with coup-contrecoup. The traditional Patrick test is performed in the supine position and is helpful for differentiating hip and back pain. However, when performed in the lateral position, the lateral rim impingement test is useful for the detection of posterior or lateral impingement. Any type of re-creation of a posterior or lateral rim complaint can be precipitated in this position. The lateral rim impingement, FABER, and posterior rim impingement tests all place the hip into positions of posterior and lateral impingement. The lateral rim impingement test establishes a functional lumbar lordosis, with a clear ability to comfortably monitor sites of impingement, which aids in the separation of posterior and lateral points of impingement.

FIGURE 1-17 Lateral rim impingement test. A, Front view. B, Rear view. The lateral rim impingement test is performed in the lateral position. The examiner cradles the patient’s lower leg with one arm and monitors the hip joint with the opposing hand. The affected hip is passively brought through a wide arc from flexion to extension in continuous abduction while externally rotating the hip (arrows).
Prone Examination
The prone examination (Table 1-6) involves palpation of four distinct areas—the supra-SI, SI, gluteus maximus, and spine (facets). Should the pain be identified in the supra-SI joint region in or about the facet, a lumbar hyperextension test can help identify the exact location of suspected pain. If this test is positive, the patient can then be placed into a supine position, with the knees flexed. If this helps alleviate the pain, the back should be evaluated further.
| Examination | Assessment and Association |
|---|---|
| Rectus contracture test (Ely test) | Rectus femoris contracture |
| Femoral anteversion test (Craig test) | Detect increased femoral anteversion or retroversion, ligamentous injury, hyperlaxity |
| Palpation | |
See video.
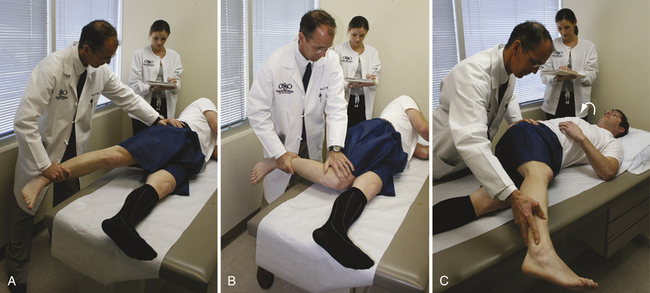
The femoral anteversion test, traditionally known as Craig’s test, will give the examiner an idea of femoral anteversion and retroversion (Fig. 1-18A).16 With the patient in the prone position, the knee is flexed to 90 degrees and the examiner manually rotates the leg while palpating the greater trochanter. The greater trochanter is positioned so that it protrudes most laterally, thereby placing the femoral head into the center portion of the acetabulum. Femoral version is assessed by noting the angle between the axis of the tibia and an imaginary vertical line. Normally, femoral anteversion is between 10 and 20 degrees.16 This test will help identify cases of retroversion. If there is a significant difference of internal rotation in the extended and seated (flexed) positions, an osseous versus a ligamentous cause should be differentiated (see Fig. 1-18B). The rectus contracture test (also known as Ely’s test) is performed with the patient in the prone position and the lower extremity flexed toward the gluteus maximus (see Fig. 1-18C). Any raise of the pelvis or restriction of hip flexion is indicative of rectus femoris contracture.

FIGURE 1-18 A, Femoral anteversion test. The knee is flexed to 90 degrees and the examiner manually rotates the leg while palpating the greater trochanter. The examiner positions the greater trochanter so that it protrudes most laterally, noting the angle between the axis of the tibia and an imaginary vertical line. B, Internal rotation in the extended position. Note any differences from the seated flexed position. C, Rectus contracture test. The lower extremity is flexed toward the gluteus maximus. Any raise of the pelvis or restriction of hip flexion motion is indicative of rectus femoris contracture.
Specific Tests
McCarthy Test.
This is a maneuver associated with a McCarthy sign, a reproducible pop or click.8 The McCarthy test is performed with the contralateral leg held in flexion. The examined hip is brought to 90 degrees flexion and then abducted, externally rotated, and extended. The hip is then brought to 90 degrees flexion, adducted, internally rotated, and extended. A positive McCarthy sign is helpful for detecting anterior femoroacetabular impingement or a torn labrum.
Seated Piriformis Stretch Test – (Figure 1-19).
The seated position offers a stable and reproducible platform with the hip at 90° of flexion. The examiner extends the knee and passively moves the flexed hip into adduction with internal rotation while palpating 1cm lateral to the ischium (middle finger) and proximally at the sciatic notch (index finger). A positive test is the recreation of the posterior pain. Freiberg has described sciatic nerve entrapment by the piriformis17 and may be entrapped in other areas which is best described as Deep Gluteal Syndrome18. Pain in the buttock may be caused from entrapment of the sciatic nerve by the piriformis muscle, hamstring, obturator internus/gemelli complex, or scar tissue. Piriformis syndrome is often due to scarring between the sciatic nerve and external rotators19. The inferior gluteal nerve, inferior gluteal artery and sciatic nerve may be scarred into the hamstring tendons due to trauma or avulsion of the hamstring20. Irritation of the structures of the obturator internus/gemelli complex are commonly overlooked in association with back pain and may cause sciatica-like pain21,22. The use of palpation of the involved anatomy along with a physical exam that includes the Straight Leg Raise Test, the Seated Piriformis Stretch Test, and Pace’s test will aid in the differential diagnosis of deep gluteal syndrome.
Abduction, Extension, External Rotation Test.
The abduction, extension, external rotation (ABDEER) test is performed in the lateral position with the affected leg passively brought into abduction, extension, and external rotation as forward pressure is applied to the posterior aspect of the hip. Re-creation of the patient’s pain is a positive test. As with the apprehension test performed on the shoulder, ABDEER is helpful for the detection of any type of anterior capsular laxity or injury. Of note, current research suggests that this position specifically releases the teres ligament.
Resisted Sit-up Test.
The athletic hernia is described as a condition of a weakened posterior wall of the inguinal canal, which results in chronic pain in the groin that may refer to other surrounding areas and is exacerbated with activity.23 Although the term hernia is associated with a bulge, it is common that no true hernia is present following laparoscopic repair. Diagnosis of the athletic hernia may be difficult because this pain may mimic the pain associated with hip pathologies. The typical athletic hernia symptoms consist of dull pain in the area of the groin that may radiate to the perineum and inner thigh or across the midline.23 Common physical examination findings include inguinal canal tenderness, pubic crest-tubercle tenderness, adductor origin tenderness, pain with resisted sit-ups or hip flexion, and a tender, dilated, superficial ring.23
Pudendal Nerve Block Test.
Four clinical features must be present for a diagnosis of pudendal nerve entrapment according to the Nantes criteria.24 These include pain in the urogenital area that is increased with sitting and that does not wake the patient at night, as well as loss of sensation of the genitalia. If these essential criteria are met, a diagnostic anesthetic pudendal nerve block should be carried out; relief of symptoms strongly supports the diagnosis.
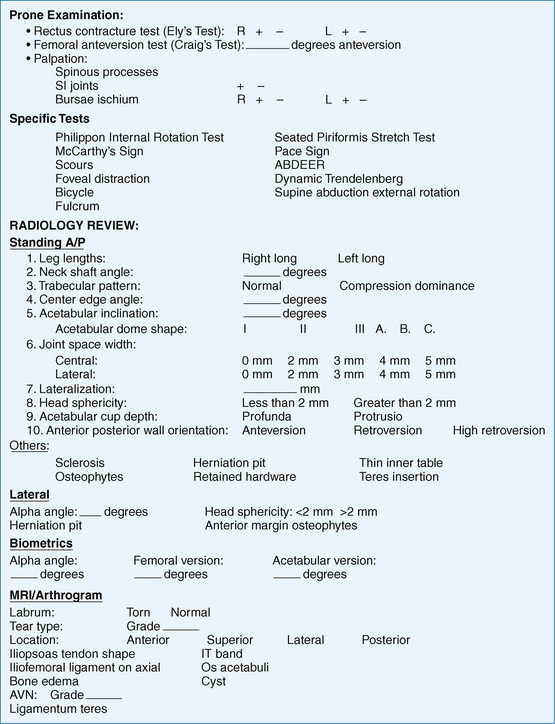
RADIOGRAPHIC ANALYSES
Evaluation by Standing Anteroposterior and Frog-Leg Lateral Views
To evaluate patients who present with hip pain fully, the following radiographic views are obtained—a standing and supine anteroposterior (AP) pelvic and frog-leg lateral view.25 Each radiographic view is critical in the diagnostic evaluation and treatment of structural abnormalities. There are a number of other radiographic views available, such as cross-table lateral,26 false profile,27,28 and 45- and 90-degree Dunn views,29 which physicians may prefer on an individual basis.30
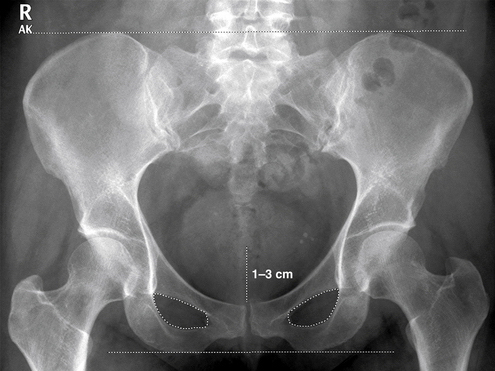
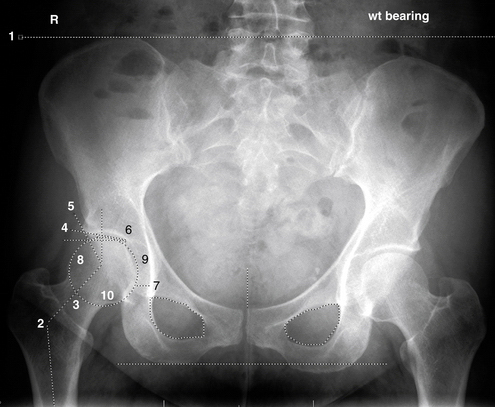
The standing AP radiograph (Fig. 1-20) is made with the patient standing with the feet in neutral rotation and shoulder width apart to resemble the natural biomechanical stance as related to gait. The feet may also be placed parallel to each other, with enough internal rotation for the feet to touch.31 The x-ray tube-to-film distance should be 120 cm, with the crosshairs centered on the midpoint between the superior border of the pubic symphysis and a line drawn connecting the anterior superior iliac spines (ASISs).30 The coccyx should be centered in line with the pubic symphysis, and the iliac wings, obturator foramina, and radiographic teardrops should be symmetrical in appearance. If pelvic inclination is appropriate, a 1- to 3-cm gap should be seen between the superior border of the pubic symphysis and the tip of the coccyx.32 This particular radiograph is used because acetabular roof obliquity, center edge angle, and minimum joint space width may vary between weight-bearing and supine positions.33 Ensuring symmetry is critical to the interpretation of radiographic findings.
The standing AP radiograph will assess the following: (1) functional leg length inequalities; (2) neck shaft angle (NSA); (3) femoral neck trabecular patterns; (4) lateral and anterior center edge angles; (5) acetabular inclination; (6) joint space width; (7) lateralization; (8) head sphericity; (9) acetabular cup depth; and (10) anterior and posterior wall orientation (Fig. 1-21).
Pathologic Definitions of Radiographic Findings
Functional Leg Lengths.
These should be considered when a patient presents with hip-related symptoms. The total length of one leg should be compared with the contralateral leg length by examining the superior border of the iliac crests. A leg length discrepancy (LLD) of more than 2.0 cm can have an adverse effect on the kinematic function of the hip.34 The difference in functional leg lengths is usually a combination of structural differences of the long bones, hemipelvis, or spine.
Neck Shaft Angle.
The NSA dictates the load transfer from the femur to the acetabulum. It is the angle formed by the longitudinal axes of the femoral neck and the proximal femoral diaphyseal axis.35 One line is drawn parallel to the midpoint of the femoral neck and one is drawn parallel to the midpoint of the femoral shaft. The angle formed represents the NSA. Normal values range from 125 to 140 degrees. If the NSA is more than 140 degrees, it is classified as coxa valgus; if less than 125 degrees, it is classified as coxa varus. The normal neck shaft angle produces the lowest stress on the femoral neck and acetabulum because of the orientation of an optimal lever arm that produces a mechanical advantage for biomechanical function.
Trabecular Pattern.
This is examined radiographically to visualize the influence of the neck shaft angle on the compressive and tensile forces within the femoral neck. In cases of coxa varus, tensile trabeculae are more prominent, whereas in cases of coxa valgus, compressive trabeculae are more prominent (Fig. 1-22).36
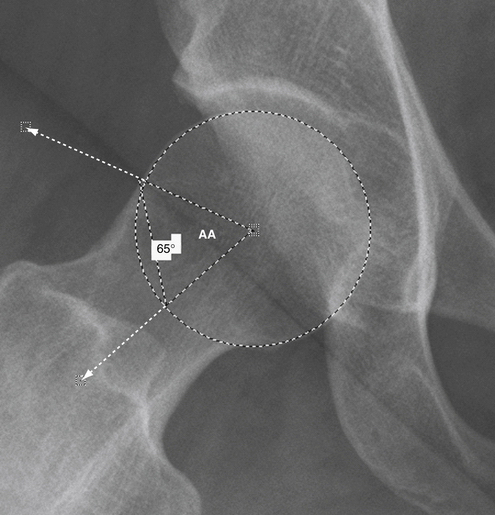
Lateral Center Edge Angles.
Lateral center edge angles (LCAs) are used to assess the degree of acetabular coverage of the femoral head. The lateral center edge angle is formed by a line drawn parallel to the longitudinal pelvic axis and a line connecting the center of the femoral head with the lateral edge of the acetabulum.37 Normal values range from 22 to 42 degrees in adults, although values less than 26 degrees may indicate inadequate coverage of the femoral head (Fig. 1-23).34,38
Anterior Center Edge Angles.
Anterior center edge angles (ACEs) are assessed from a false profile view and are determined if there is dysplasia to help locate acetabular overcoverage.26,39,40 The false profile view is performed with the patient standing with the affected hip against the cassette and pelvis rotated 65 degrees in relation to the wall stand. The foot on the same side as the affected hip is placed parallel to the cassette. The central beam is centered on the femoral head with a tube-to-film distance of 120 cm. A vertical line and a line connecting the center of the femoral head with the anterior edge of the acetabulum form the ACE. In consideration for intertrochanteric osteotomy (ITO) and periacetabular osteotomy (PAO), an abducted internal rotation radiograph allows for the examination of the centralization of the femoral head with improved acetabular coverage.
Acetabular Inclination.
This is the angle (Tonnis angle of inclination)35 formed by a horizontal line and a tangent from the lowest point of the sclerotic zone of the acetabular roof to the lateral edge of the acetabulum (Fig. 1-24). Three classifications are used for acetabular inclination30,41:
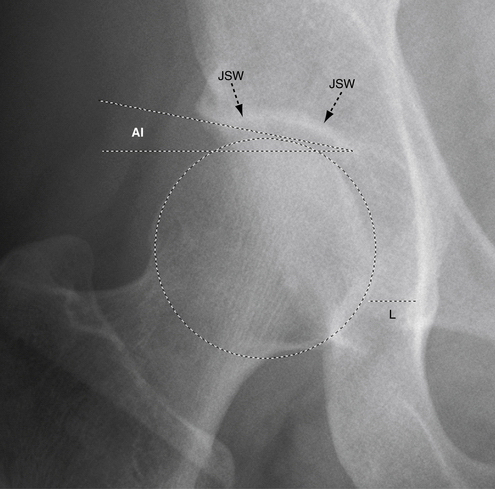
Joint Space Width.
This is measured as the shortest distance between the femoral head surface and acetabulum, centrally and laterally, at the weight-bearing sclerotic zone (see Fig. 1-24). Joint space width is examined using the standing AP radiograph because the effects of position influence the joint space observed.42 Any evidence of joint space narrowing can be classified using the Tonnis grade for osteoarthritis.35 The Tonnis grade41 for osteoarthritis can be correlated using all radiographic views, but the final grade is determined on the basis of the single view with the highest overall degree of osteoarthritic change.30
Hip Center Position.
If the medial aspect of the femoral head is more than 10 mm from the ilioischial line, the hip is classified as lateralized and nonlateralized if the medial aspect of the femoral head is within a 10-mm margin from the ilioischial line. Comparisons from side to side may help determine any amount of lateralization (see Fig. 1-24).
Head Sphericity.
This should be assessed on standing AP and frog-leg lateral radiographs because a patient may have an apparently spherical head on the AP view, but not on the lateral view. The femoral head is classified as spherical if the epiphysis does not extend beyond the margin of a reference circle by more than 2 mm and is classified as aspherical if it extends beyond this 2-mm margin (see Fig. 1-24).43,44
Acetabular Cup Depth.
The relationship of the floor of the fossa acetabuli and femoral head are evaluated relative to the ilioischial line. If the floor of the fossa acetabuli touches or is medial to the ilioischial line, or the posterior wall extends lateral to the center axis of rotation, the hip is classified as coxa profunda. If the medial aspect of the femoral head is medial to the ilioischial line, the head is classified as protrusio.45 Also, the inner acetabular wall thickness, medial wall shape, and inferior cup orientation should be recognized.
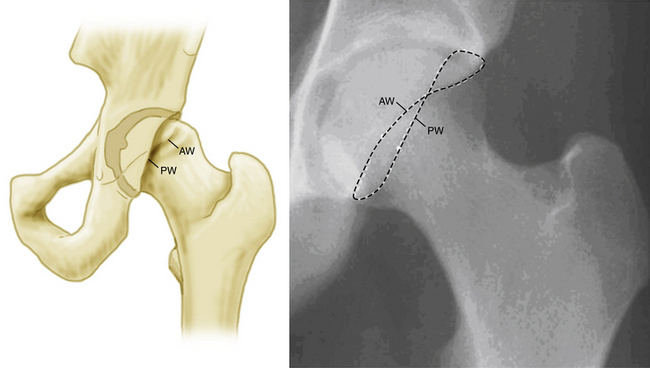
Acetabular Version.
Acetabula can be classified as anteverted or retroverted based on the presence or absence of a crossover sign (Fig. 1-25).46 The acetabulum is classified as anteverted if the line of the anterior aspect of the rim does not cross the line of the posterior aspect of the rim before reaching the lateral aspect of the sourcil. If the anterior aspect of the rim does cross the line of the posterior aspect of the rim before reaching the lateral edge of the sourcil, the acetabulum is classified as retroverted. It is important to note that true acetabular retroversion is associated with a deficient posterior wall,46 whereas a hip with a crossover sign but no posterior wall deficiency refers to anterior overcoverage—cranial acetabular retroversion or anterior focal acetabular retroversion.30,47 Both standing and supine AP radiographs should be used to determine anterior and posterior wall inclination, again ensuring good quality because of the possibility of overinterpreting the incidence of retroversion.33
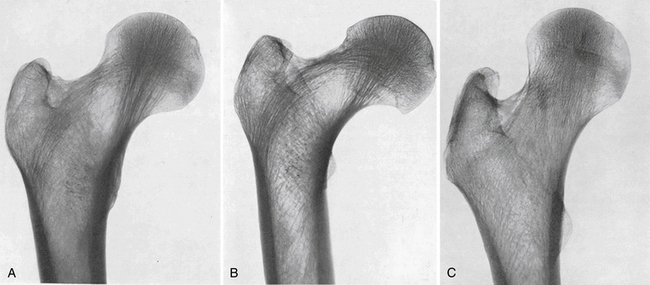
Frog-Leg Lateral Radiograph.
This allows for the assessment of another view of medial and lateral joint space width, femoral head sphericity, congruency, head-neck offset, alpha angle, and bone morphology (Fig. 1-26). The frog-leg lateral radiograph should be taken with the patient supine, the affected limb flexed at the knee approximately 30 to 40 degrees, and the hip abducted to 45 degrees. The heel should rest against the medial aspect of the contralateral knee. The cassette is placed so that the top of the film rests at the ASIS and the crosshairs directed midway between the ASIS and pubic symphysis. The x-ray tube-to-film distance should be approximately 102 cm. This particular orientation is used because it is easily reproducible in the operating room and allows for a consistent radiographic view of the head-neck junction offset during the pre- and intraoperative radiographic examination.
Head-Neck Offset.
This is assessed from the frog-leg lateral radiograph and is classified based on the gross appearance of the relationship between the radius curvatures of the anterior aspect of the femoral head with the posterior aspect of the head neck junction.43 The head-neck offset is classified as symmetrical if the anterior and posterior concavities are grossly symmetrical. If the anterior concavity has a radius of curvature greater than that at the posterior aspect of the head-neck (H-N) junction, it is classified as having a moderate decrease in H-N offset. If the anterior aspect has a convexity, as opposed to a concavity, the head-neck junction is classified as having a prominence (CAM-type FAI).43
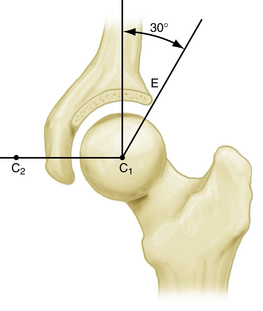
Alpha Angle.
This is calculated by drawing a line from the center of the femoral head to the point on the anterolateral aspect of the head-neck junction where the radius of the femoral head deviates from the more central femoral head radius in the acetabulum, or where a prominence starts, and a line drawn through the center of the femoral neck to the center of the femoral head (see Fig. 1-26). Values of more than 42 degrees are suggestive of head-neck offset deformity,30 but are dependent on acetabular femoral congruency.34
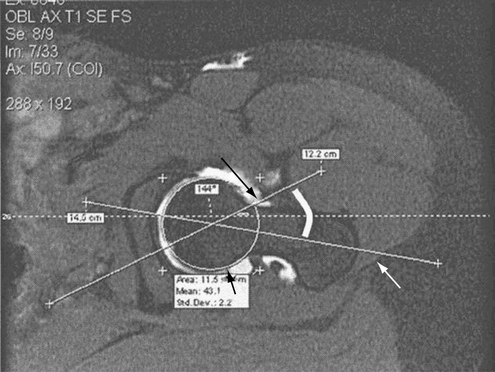
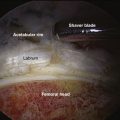
Cross-Sectional Imaging Techniques
The use of cross-sectional imaging (Fig. 1-27) is essential for the evaluation of patients for intra- and extra-articular pathology. Imaging protocols such as magnetic resonance imaging (MRI), magnetic resonance arthrography (MRA),48 multidetector computed tomography (MDCT),34 and computed tomography (CT)49 allow for the assessment of basic structural torsional alignment that give rise to or predispose patients to certain types of pathology such as FAI, acetabular tears, or articular damage.
The McKibbin instability index can be calculated from MRI scans and is based on the assumption that the effects of femoral and acetabular anteversion may be additive or may offset each other. It is calculated as the sum of the angles of femoral and acetabular anteversion, with an index of 60 denoting severe instability. Deviation is classified as ranging from grade −3, for a low instability index of less than 20, to grade +3, for a high instability index of more than 50.50 For this technique, the feet should be pointing straight ahead and held in place by a brace or tape to ensure that the geometric relationship of the acetabulum and femur are properly evaluated.
MDCT (see Fig. 1-27) is useful for assessing osseous structures and surrounding soft tissues of the hip and acetabulum and provides data that have the same resolution in the longitudinal axis (z axis) as in the x or y axis.34 This relationship is important to understand because of the potential not only to detect anatomic derangements that may allow movements that create primary pathology, but also to correct the underlying anatomic abnormalities that may predispose the patient to recurrent or persistent pathology.
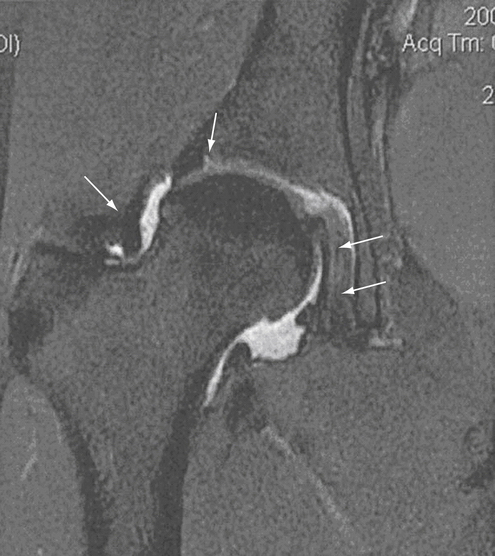
MRA (Figs. 1-28 and 1-29) provides assistance in the evaluation of intra-articular pathology of the hip. The detection of acetabular labral tears may assist in confirming a decision for arthroscopic surgery and has been reported to have a positive predictive value of 93%.51 MRA may also be helpful in the evaluation of mild osseous abnormalities, such as acetabular retroversion and reduced head-neck offset, the integrity of the acetabular labrum, and articular cartilage surface. The ability to detect these subtle abnormalities accurately may be affected by the technique and experience of the radiologist and by the quality of scanner used for imaging. Research using delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC), which measures the loss of glycosaminoglycans in the early stages of arthritis, has demonstrated that dGEMRIC can detect early stages of osteoarthritis caused by hip dysplasia and femoroacetabular impingement.52
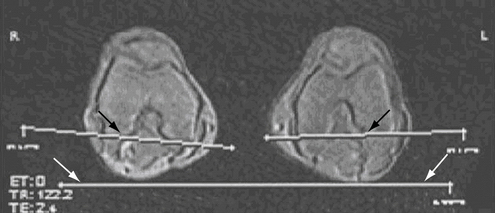
FIGURE 1-28 Axial gradient echo MR image of the knees taken from a tri-plane localizer sequence shows the coronal reference line (white arrows) and the posterior intercondylar line (white line with black shadowing indicated by the black arrows). The amount of internal or external rotation is then compared with the coronal reference line and the overall amount of femoral version is calculated. For example, if the proximal femur shows 3 degrees of external rotation and the distal femur shows 15 degrees of internal rotation, the amount of anteversion of the femur is 18 degrees (from 3 degrees external rotation proximally to 15 degrees of internal rotation distally). Foot rotation must be controlled by bracing or taping between the two images.
(From Beall DP, Martin HD, Mintz DN, et al. Anatomic and structural evaluation of the hip: a cross-sectional imaging technique combining anatomic and biomechanical evaluations. Clin Imaging. 2008;32:372-381.)
SUMMARY AND CONCLUSIONS
As our understanding of hip pathology advances, the physical examination of the hip continues to evolve. To understand the findings fully, one must be familiar with the anatomy and biomechanics of the hip joint. The use of a formalized, reproducible physical examination will help identify and distinguish osseous, musculotendinous, and ligamentous abnormalities and their comorbidities in a timely fashion (Fig. 1-30). Radiographs and cross-sectional imaging techniques, together with a standardized physical examination, will aid in the preoperative, intraoperative, and postoperative assessment of the hip. The physical examination of the hip is also used as a guide to monitor physical therapy and postoperative rehabilitation. This chapter has introduced a framework of discussion regarding clinically and biomechanically relevant physical examinations.
ACKNOWLEDGMENTS
I would like to thank Shea A. Shears, Aaron M. Smathers, Ian J. Palmer, and all the members of the MAHORN (Multicenter Arthroscopy of the Hip Outcomes Research Network) Group who were instrumental in the development of this chapter.
1. Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908-914.
2. Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833-1840.
3. Martin RL, Philippon MJ. Evidence of reliability and responsiveness for the hip outcome score. Arthroscopy. 2008;24:676-682.
4. Scopp JM, Moorman CT3rd. The assessment of athletic hip injury. Clin Sports Med. 2001;20:647-659.
5. DeAngelis NA, Busconi BD. Assessment and differential diagnosis of the painful hip. Clin Orthop Relat Res. 2003;406:11-18.
6. Kujala UM, Kaprio J, Sarna S. Osteoarthritis of weight bearing joints of lower limbs in former elite male athletes. BMJ. 1994;308:231-234.
7. Boyd KT, Peirce NS, Batt ME. Common hip injuries in sport. Sports Med. 1997;24:273-288.
8. Byrd JWT. Physical examination. In: Byrd JWT, editor. Operative Hip Arthroscopy.. New York: Springer; 2005:36-50.
9. Martin HD. Clinical examination of the hip. Oper Tech Orthop. 2005;15:177-181.
10. Braly BA, Beall DP, Martin HD. Clinical examination of the athletic hip. Clin Sports Med. 2006;25:199-210.
11. Torry MR, Schenker ML, Martin HD, et al. Neuromuscular hip biomechanics and pathology in the athlete. Clin Sports Med. 2006;25:179-197.
12. Perry J. Gait Analysis: Normal and Pathological Function, Thorofare, NJ: Slack; 1992.
13. Martin HD, Savage A, Braly BA, et al. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008;24:188-195.
14. Pace JB, Nagle D. Piriform syndrome. West J Med. 1976;124:435-439.
15. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423-429.
16. Reider B, Martel J. Pelvis, hip and thigh. In: Reider B, Martel J, editors. The Orthopedic Physical Examination. Philadelphia: WB Saunders; 1999:159-199.
17. Freiberg A. Sciatic pain and its relief by operations on muscle and fascia. Arch Surg. 1937;34:337-350.
18. McCrory P, Bell S. Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med. 1999;27:261-274.
19. Benson ER, Schutzer SF. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am. 1999;81:941-949.
20. Miller SL, Gill J, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. A cadaveric study. J Bone Joint Surg Am. 2007;89:44-48.
21. Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli-obturator internus complex. J Manipulative Physiol Ther. 2005;28:534-538.
22. Meknas K, Christensen A, Johansen O. The internal obturator muscle may cause sciatic pain. Pain. 2003;104:375-380.
23. Swan KGJr, Wolcott M. The athletic hernia: a systematic review. Clin Orthop Relat Res. 2007;455:78-87.
24. Labat JJ, Riant T, Robert R, et al. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourol Urodyn. 2008;27:306-310.
25. Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115-121.
26. Eijer H, Leunig M, Mahomed M, Ganz R. Cross-table lateral radiograph for screening of anterior femoral head-neck offset in patients with femoroacetabular impingement. Hip Int. 2001;11:37-41.
27. Lequesne M de S. False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies. Rev Rhum Malad Osteoarticul. 1961;28:643-652.
28. Lequesne MG, Laredo JD. The faux profil (oblique view) of the hip in the standing position. Contribution to the evaluation of osteoarthritis of the adult hip. Ann Rheum Dis. 1998; 57: 676-681.
29. Dunn DM. Anteversion of the neck of the femur; a method of measurement. J Bone Joint Surg Br. 1952;34:181-186.
30. Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg. 2008;90(suppl 4):47-66.
31. Troelsen A, Jacobsen S, Romer L, Soballe K. Weightbearing anteroposterior pelvic radiographs are recommended in DDH assessment. Clin Orthop Relat Res. 2008;466:813-819.
32. Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;2407:41-48.
33. Fuchs-Winkelmann S, Peterlein CD, Tibesku CO, Weinstein SL. Comparison of pelvic radiographs in weightbearing and supine positions. Clin Orthop Relat Res. 2008;466:809-812.
34. Beall DP, Martin HD, Mintz DN, et al. Anatomic and structural evaluation of the hip: a cross-sectional imaging technique combining anatomic and biomechanical evaluations. Clin Imaging. 2008;32:372-381.
35. Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999; 81: 1747-1770.
36. Pauwels F. Biomechanics of the Normal and Diseased Hip. New York: Springer-Verlag; 1976.
37. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83:28-38.
38. Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am.. 1995;77:985-989.
39. Delaunay S, Dussault RG, Kaplan PA, Alford BA. Radiographic measurements of dysplastic adult hips. Skeletal Radiol. 1997;26:75-81.
40. Crockarell JRJr, Trousdale RT, Guyton JL. The anterior centre-edge angle: A cadaver study. J Bone Joint Surg Br. 2000;82:532-534.
41. Tonnis D. General radiography of the hip joint. In: Tonnis D, editor. Congenital Dysplasia and Dislocation of the Hip. Berlin-Heidelberg: Springer; 1987:100-142.
42. Conrozier T, Lequesne MG, Tron AM, et al. The effects of position on the radiographic joint space in osteoarthritis of the hip. Osteoarthritis Cartilage. 1997;5:17-22.
43. Notzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556-560.
44. Jager M, Wild A, Westhoff B, Krauspe R. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci. 2004;9:256-263.
45. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012-1018.
46. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281-288.
47. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540-1552.
48. Petersilge CA. From the RSNA Refresher Courses. Radiological Society of North America. Chronic adult hip pain: MR arthrography of the hip. Radiographics. 2000;20(spec no.):S43-S52.
49. Millis MB, Murphy SB. Use of computed tomographic reconstruction in planning osteotomies of the hip. Clin Orthop Relat Res. 1992;274:154-159.
50. McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148-159.
51. Keeney JA, Peelle MW, Jackson J, et al. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004;429:163-169.
52. Kim YJ, Jaramillo D, Millis MB, et al. Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am. 2003;85:1987-1992.