Cleft–Orthognathic Surgery
The Isolated Cleft Palate Deformity
• Facial Growth Implications of Cleft Palate Repair in the Infant with Isolated Cleft Palate
• Timing of Orthognathic Surgery
• Residual Deformities in the Adolescent with Isolated Cleft Palate
• Orthodontic Considerations in the Patient with Isolated Cleft Palate with a Jaw Deformity
• Immediate Presurgical Assessment
• Orthognathic Surgical Approach for Isolated Cleft Palate
• Clinical Management after Initial Surgical Healing
• Orthognathic Surgery for Isolated Cleft Palate: Review of Study
Facial Growth Implications of Cleft Palate Repair in the Infant with Isolated Cleft Palate
Ross documented that at least 20% of Caucasian individuals with ICP who undergo repair during infancy will experience maxillary hypoplasia that results in malocclusion that is not responsive to either traditional or compensatory orthodontic maneuvers alone.86 Chen and colleagues reported on horizontal maxillary growth in both children and adults with Eastern Chinese ethnic backgrounds and with unoperated and operated ICP.14 There were two study groups: individuals in Group 1 had non-syndromal and unoperated ICP that was evaluated during the mixed dentition (n = 16); individuals in Group 2 had non-syndromal and unoperated ICP that was evaluated during the permanent dentition (n = 25). The control groups included patients with ICP who underwent repair during childhood as well as non-cleft individuals with Class I occlusion that was evaluated during both the mixed and permanent dentitions. Lateral cephalograms of all subjects were analyzed. The results of the mixed dentition groups showed almost normal sagittal growth in unoperated patients except for the reduced anterior-posterior maxilla length. In contrast, the operated patients showed reduced length of both the maxilla and mandible, as well as a clockwise rotation of the mandible. The analysis of the permanent dentition groups showed that in both the unoperated and operated ICP patients, there were reductions in maxilla length, mandibular protrusion, and maxillary retrusion. Interestingly, there appeared to be no correlation between maxillary growth restriction and the extent of the congenital clefting of the secondary palate (i.e., soft palate only versus hard and soft palate). The authors concluded that, for individuals born with ICP, the etiology of the maxillomandibular deficiency likely results from a combination of factors, including the intrinsic primary (cleft) defect; secondary hypoplasia as a result of the surgical repair during infancy (iatrogenic); and functional (environmental) factors (e.g., the effects of muscles of mastication, respiratory patterns, mandibular rest posture; see Chapter 4). These results were similar to those of Yoshida and colleagues, who found that individuals with ICP frequently end up with maxillary horizontal deficiency and clockwise rotation of the maxillomandibular complex that tend to become worse as the child reaches adulthood.99
A significant percentage of adolescent patients who were born with ICP will present with a jaw deformity that requires, at minimum, a maxillary Le Fort I (down-fracture) osteotomy to align the jaws.5,85 When indicated, this is combined with mandibular and chin osteotomies to achieve improved facial proportions and with intranasal procedures (i.e., septoplasty and inferior turbinate reduction) to improve nasal breathing.
Coordinated Team Approach
The facial reconstructive and dental rehabilitation of an individual with ICP is best delivered via collaborative care provided by appropriate medical and dental specialists.6,62,71 It is no longer justified for individual practitioners—whether they are surgeons, orthodontists, restorative dentists, speech pathologists, or otolaryngologists—to carry out extensive treatment without informing the patient and his or her family of available options and considering clinical input from the other specialists who are caring for the patient.
Treatment Protocol
The primary cleft surgeon completes the patient’s palate repair during infancy, and this is followed by pharyngeal procedures later during the patient’s childhood if they are required to improve velopharyngeal function. The surgeon is also likely to play an important role in directing the patient’s care throughout adolescence and into adulthood. If the cleft surgeon is not trained in skeletal procedures, then a timely and seamless transition to the maxillofacial surgeon who will continue on with the patient’s reconstruction is necessary. The orthodontist identifies early abnormal facial growth patterns and may carry out interceptive treatment.6,10,11,18,19,27,34,51,55,64,65,87,90,91 Definitive orthodontic treatment is coordinated with orthognathic surgery, when indicated.33 Extensive compensatory orthodontic treatment is likely to jeopardize periodontal health and to lead to dental relapse with recurrent malocclusion. Camouflage orthodontics should be avoided for these reasons and only be entered into with full disclosure to the family and other treating clinicians.
Before orthognathic surgery is performed, the speech pathologist performs an evaluation to assess the patient’s velopharyngeal function; this will ideally include nasoendoscopic instrumentation. Such evaluation is important, because velopharyngeal function may deteriorate after maxillary Le Fort I osteotomy with advancement (see Chapter 8). Velopharyngeal closure that was adequate before surgery may become borderline afterward, and closure that was borderline may become inadequate. In the past, investigators have speculated that, if the distraction (DO) technique is used to advance the Le Fort I osteotomy, then velopharyngeal function will not deteriorate. However, clinical studies have now documented that velopharyngeal function will deteriorate in a similar fashion after Le Fort I advancement when either DO or standard techniques are used.12,13,35,37,50,54,58,61,72,89,94 Articulatory distortions that result from the jaw discrepancy and malocclusion also are identified by the speech pathologist, and cause-and-effect relationships are determined. It is known that the successful orthodontic and surgical correction of crossbites, open bite, residual palatal fistulas, and negative overjet will generally correct the presenting articulation errors (see Chapter 8).
The otolaryngologist plays a role in the assessment of upper airway and middle ear function. Chronic nasal obstruction and sinusitis are frequent in the patient with a cleft palate. Mucous trapping may also be a problem after a pharyngeal flap procedure. If sleep apnea is suspected, an attended polysomnogram should be carried out (see Chapter 26). If intranasal procedures (i.e., septoplasty and inferior turbinate reduction) are needed to improve breathing, they should be simultaneously carried out in conjunction with orthognathic surgery (see Chapter 10).
Timing of Orthognathic Surgery
The correction of the jaw deformity associated with ICP is best carried out when the skeleton is mature and before the patient completes high school, if feasible. Maxillofacial growth is generally complete between the ages of 14 and 16 years in girls and between the ages of 16 and 18 years in boys. However, skeletal growth is variable, and it may be further clarified via the analysis of sequential cephalometric radiographs (see Chapter 17). Input from the patient and the family regarding the timing of surgery and the patient’s functional needs (e.g., breathing, speech, chewing, swallowing, body image, self-esteem) are also important considerations.
As early as 1986, clinicians clarified through preliminary studies that, if jaw surgery is undertaken in the growing patient with a cleft palate patient, revision orthognathic surgery will likely be required after skeletal maturity is reached.95–98 More recently, other investigators have tested this theory by proceeding with Le Fort I osteotomy involving DO methods during the mixed dentition. Studies to date indicate that a Le Fort I osteotomy carried out during the mixed dentition, whether with a standard or a DO technique, results in limited or no further horizontal maxillary growth.17,36,46,73,74 As the mandible continues to grow, an Angle Class III malocclusion recurs with the need for either additional Le Fort I advancement or mandibular set-back.
Residual Deformities in the Adolescent with Isolated Cleft Palate
The adolescent or adult patient with ICP who is referred for orthognathic evaluation will have an intact alveolar ridge and generally will have a full complement of teeth. However, these individuals may present with one or more of the following residual cleft-related problems (Figs. 34-1 through 34-9):

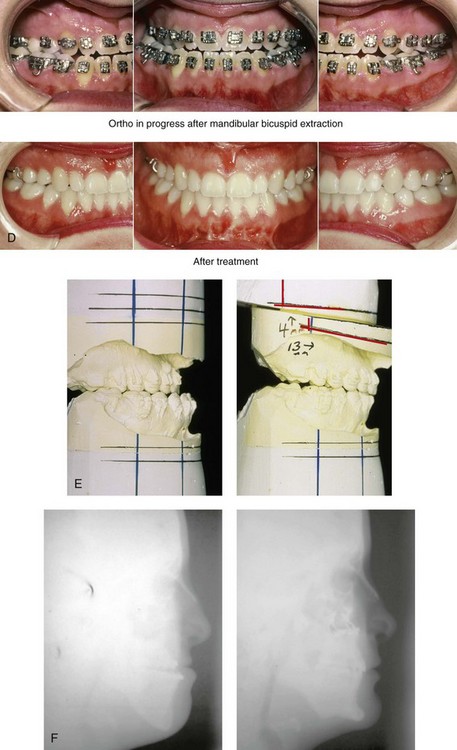
Figure 34-1 A 19-year-old woman who was born with isolated cleft palate. The maxillary deformity is characterized primarily by horizontal deficiency. The patient underwent mandibular first bicuspid extractions. She was referred to this surgeon and agreed to a comprehensive orthodontic and orthognathic surgical approach. The patient’s procedures included Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation) with interpositional grafting; osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Profile views before and after reconstruction. D, Occlusal views during orthodontics and after reconstruction. E, Articulated dental casts indicate analytic model planning. F, Lateral cephalometric radiographs before and after reconstruction. A, C, D (top center and bottom center), E (right), from Posnick JC: Skeletal stability and relapse patterns after Le Fort I osteotomy using miniplate fixation in patients with isolated cleft palate. Plast Reconstr Surg 94:51, 1994.

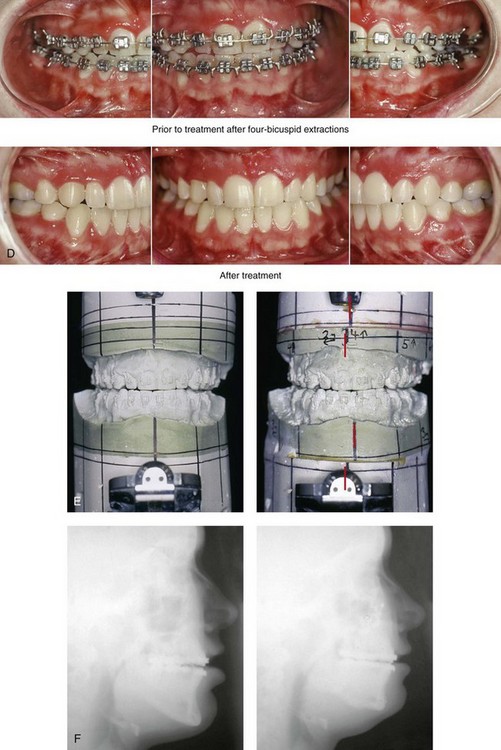
Figure 34-2 A 19-year-old woman who was born with isolated cleft palate. The deformity is characterized by vertical maxillary excess and jaw asymmetry. The patient underwent four-bicuspid extractions. She was referred to this surgeon and agreed to a comprehensive orthodontic and orthognathic approach. The patient’s procedures included Le Fort I osteotomy (minimal horizontal advancement, clockwise rotation, vertical intrusion, and asymmetry correction); bilateral sagittal split ramus osteotomies (correction of asymmetry); osseous genioplasty (vertical reduction); and septoplasty, inferior turbinate reduction, and nasal recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Profile views before and after reconstruction. D, Occlusal views with orthodontics in progress and after reconstruction. E, Articulated dental casts indicate analytic model planning. F, Lateral cephalometric radiographs before and after reconstruction.
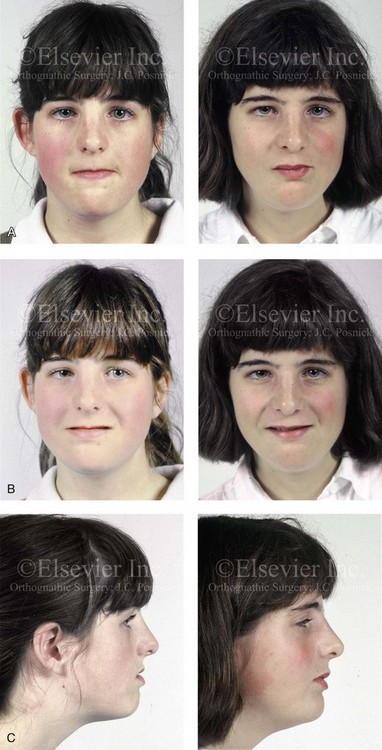
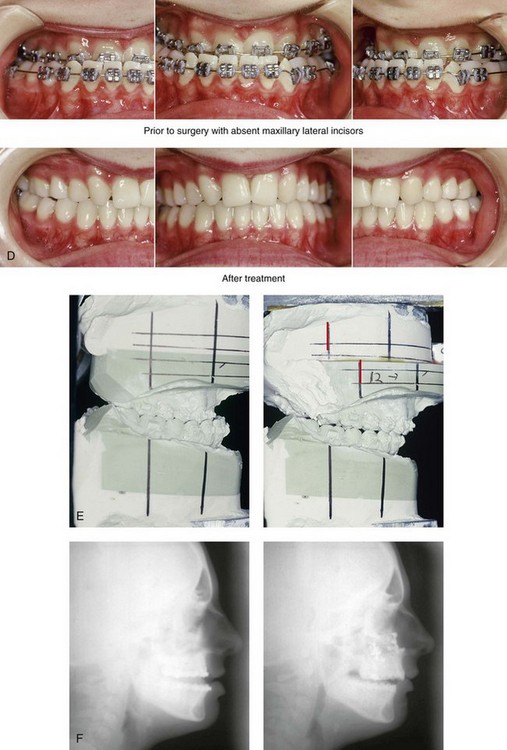
Figure 34-3 A 17-year-old girl who was born with isolated cleft palate. The deformity is characterized primarily by horizontal maxillary deficiency and a palate fistula. The patient was referred to this surgeon and agreed to a comprehensive orthodontic and orthognathic approach. The maxillary lateral incisors were congenitally absent. The patient’s procedures included a Le Fort I osteotomy (horizontal advancement and vertical lengthening) with interpositional grafting. One year after the initial procedure, she underwent an anterior-based dorsal tongue flap procedure for palatal fistula closure. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Profile views before and after reconstruction. D, Occlusal views with orthodontics in progress and after reconstruction. E, Articulated dental casts indicate analytic model planning. F, Lateral cephalometric radiographs before and after reconstruction. A, C, D, F, from Posnick JC, Tompson B: Cleft–orthognathic surgery: complications and long-term results. Plast Reconstr Surg 96:255, 1995.
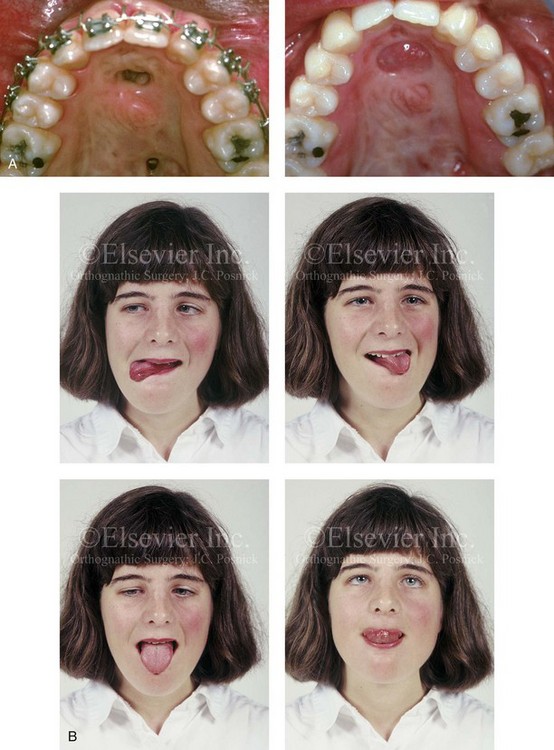
Figure 34-4 The patient from Figure 34-3 is shown after the successful placement of an anterior-based dorsal tongue flap for palatal fistula closure. A, Palatal views before and after the tongue-flap closure of a recalcitrant fistula. B, Facial views of the patient demonstrating a full range of tongue motion after the harvesting of tissue for palatal reconstruction.
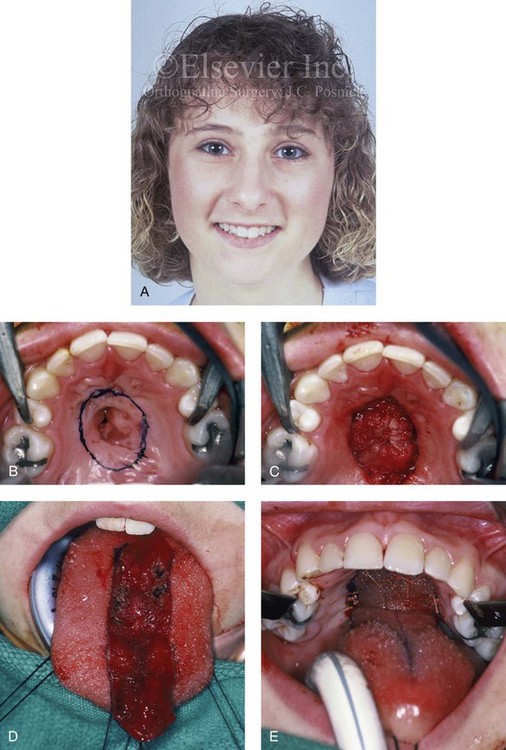
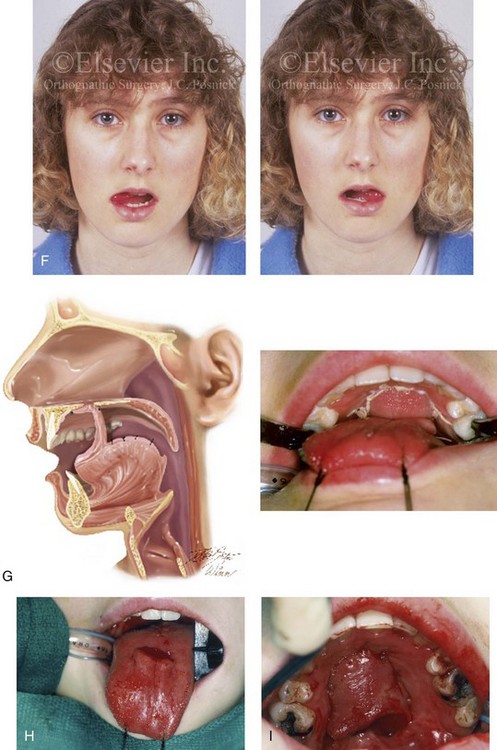
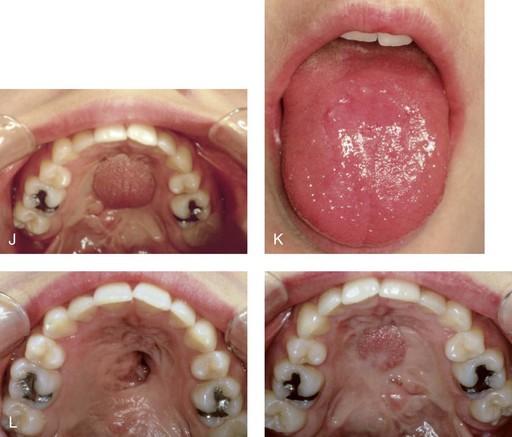

Figure 34-5 A 17-year-old girl with a recalcitrant fistula at the incisal foramen region. The fistula had been present since the time of her initial cleft palate repair, despite several attempts at closure at another institution during the patient’s childhood. She was referred to this surgeon for management. The fistula at the incisive foramen was successfully closed with an anteriorly based dorsal tongue flap. A, Facial views before fistula closure. B, Intraoperative view of the palatal fistula, with ink used to mark the extent of the bony defect. C, Local palatal flaps were developed and turned over for nasal-side closure. D, The elevated anteriorly based dorsal tongue flap is shown. It measured two thirds of the width of the tongue and was approximately 5 cm in length. E, The flap is inset to cover the oral side of the palatal defect. The tongue flap is then sutured to the adjacent palatal tissue three quarters of the way around. The posterior aspect of the flap is not sutured, because this would compromise flap circulation. The oro-tracheal tube can be seen on the side of the tongue. F, Range of motion of the tongue is demonstrated at 10 days after flap inset and before flap release. G, Illustration of a cross-sectional sagittal view of face. The tongue flap is shown inset into the palate. Intra-operative view just 10 days after the procedure is also shown. She is returned to the operating room for flap release and inset. H, Intraoperative view of the dorsum of the tongue just after sectioning of the flap and before recontouring. I, Palatal view of bulky tongue tissue on the roof of the mouth before recontouring. J, Palatal view 3 months after flap inset and before debulking. K, Dorsum of the tongue 3 months after flap inset. L, Palatal views before and 8 months after the tongue flap was placed and debulking procedure completed. M, Demonstration of the range of tongue motion 3 months after flap release.
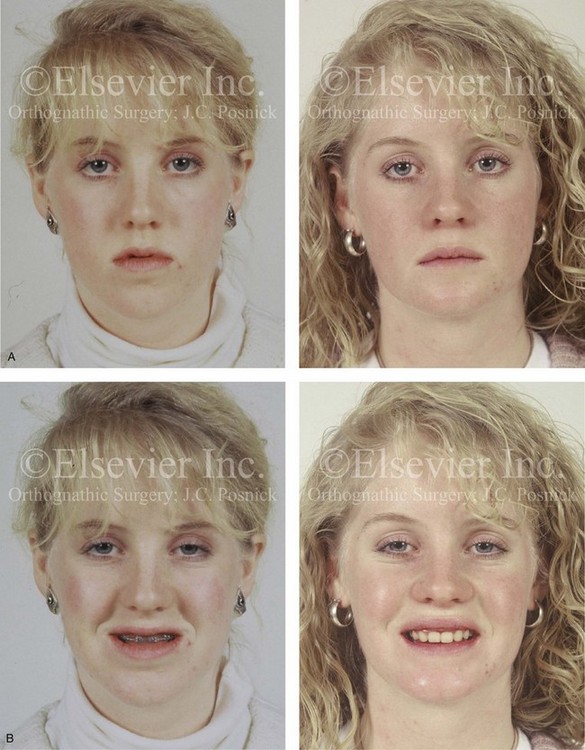

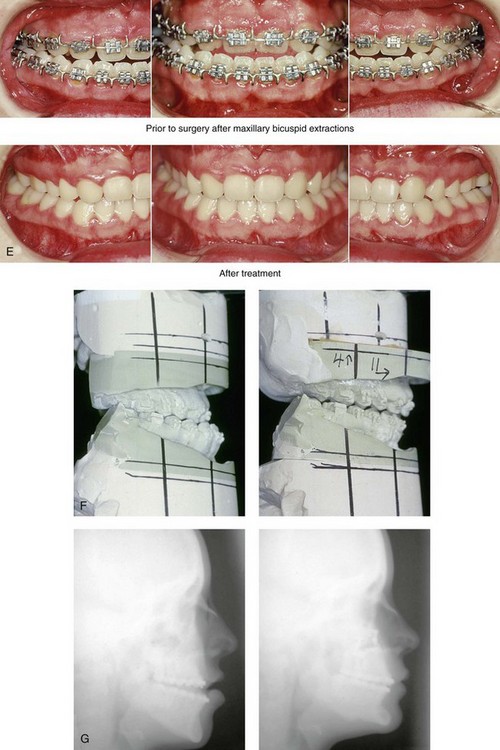
Figure 34-6 A 16-year-old girl who was born with isolated cleft palate. The deformity is characterized by horizontal and vertical deficiency of the maxilla and obstructed nasal breathing. The patient agreed to a comprehensive orthodontic and orthognathic surgical approach. Her maxillary first bicuspids were removed. The patient’s procedures included Le Fort I osteotomy (horizontal advancement and vertical lengthening) with interpositional grafting; osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views with orthodontics in progress and after reconstruction. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after reconstruction.

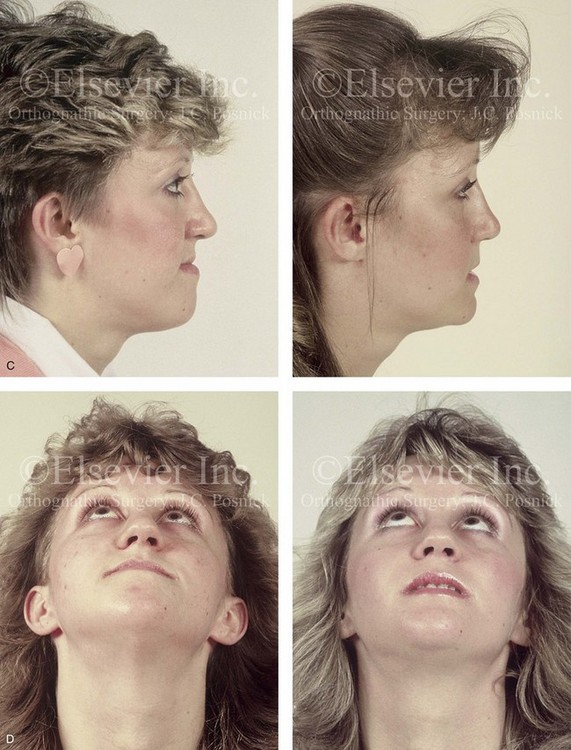
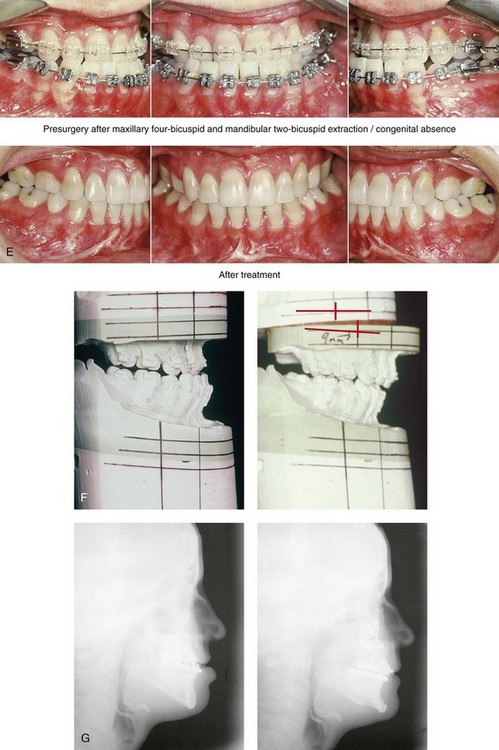
Figure 34-7 A woman in her early 20s who was born with isolated cleft palate. The deformity is characterized primarily by the horizontal and vertical deficiency of the maxilla. She was referred to this surgeon and agreed to a comprehensive orthodontic and orthognathic surgical approach. She had a congenital absence of some of her teeth, and also required extractions. All total four bicuspids in the maxilla and two bicuspids in the mandible are missing. The patient’s procedures included Le Fort I osteotomy (horizontal advancement and vertical lengthening) with interpositional grafting; osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Profile views before and after reconstruction. D, Worm’s-eye views before and after reconstruction. E, Occlusal views with orthodontics in progress and after reconstruction. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after reconstruction. A, B, C (left), E (top middle, bottom middle), F, G, from Posnick JC, Ewing MP: The role of plate and screw fixation in the treatment of cleft lip and palate jaw deformities. In Yaremchuk MJ, Gruss JS, Manson PM, eds: Rigid fixation of the craniomaxillofacial skeleton. Stoneham, Mass, 1992, Butterworth, pp 466–485.


Figure 34-8 A 16-year-old girl who was born with isolated cleft palate. The deformity is characterized primarily by the horizontal and vertical deficiency of the maxilla and chronic obstructed nasal breathing. The patient was referred to this surgeon and underwent a combined orthodontic and orthognathic surgical approach. Four bicuspids were removed. The patient’s procedures included Le Fort I osteotomy (vertical lengthening and horizontal advancement) with interpositional grafting; sagittal split ramus osteotomy of the mandible (clockwise rotation); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views with smile before and after reconstruction. B, Oblique views before and after reconstruction. C, Profile views before and after reconstruction. D, Occlusal views with orthodontics in progress and after reconstruction. E, Lateral cephalometric radiographs before and after reconstruction.


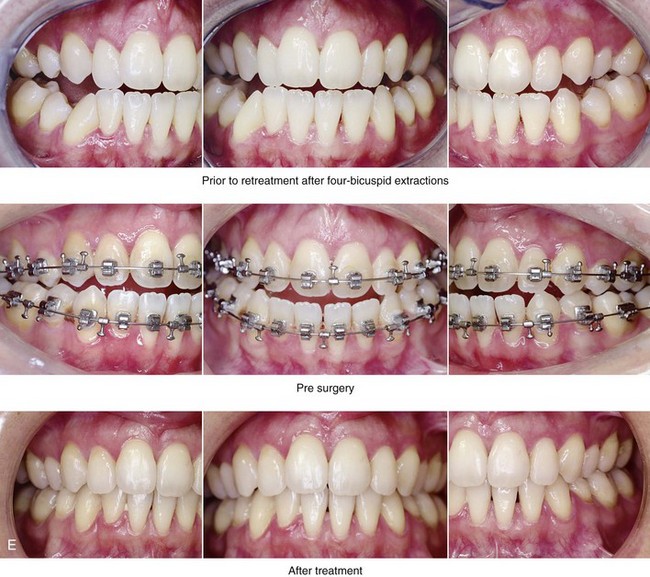

Figure 34-9 A woman in her late 20s who was born with isolated cleft palate. She developed a jaw deformity with malocclusion. Attempts to neutralize the occlusion included four bicuspid extractions with 6 years of orthodontic growth modification and orthodontic mechanics when the patient was between 11 and 17 years old. She was left with generalized labial bone loss and gingival recession, especially of the lower anterior teeth. She presented to this surgeon as an adult with a lifelong history of obstructed nasal breathing and a long face growth pattern that involved the maxilla, the mandible, and the chin; this included excess anterior facial height and horizontal retrusion. She was evaluated by clinicians in many specialties, including periodontics, prosthodontics, orthodontics, surgery, speech pathology, and otolaryngology. She underwent periodontal treatment and then orthodontic decompensation. The patient’s procedures included Le Fort I osteotomy (horizontal advancement, vertical intrusion and clockwise rotation); bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before retreatment, after orthodontic decompensation, and after reconstruction. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric views before and after reconstruction.
1. Maxillary dysplasia. When maxillary dysplasia occurs in the patient with ICP, it generally follows one of two patterns. The first and most frequently seen is horizontal maxillary retrusion, generally with a degree of vertical deficiency and often with clockwise rotation of the maxillary plane. The second pattern is vertical maxillary excess with a more limited degree of horizontal retrusion. The latter tends to occur in the presence of nasal obstruction with forced mouth breathing and an open-mouth posture, especially if a pharyngeal flap was placed during childhood (see Chapter 4).
2. Residual oronasal (palatal) fistula. There may be a residual midline palatal fistula located in the region between the incisive foramen and the soft palate. This is a residual defect that occurs after initial palate repair earlier in life.
3. Residual bony defects. The alveolus is not clefted, but residual bony defects of the hard palate are to be expected. The hard palate bony defects do not generally require grafting or reconstruction.
4. Chin dysplasia. The patient with ICP will frequently be a mouth breather with resulting open-mouth posture. The end result is often a vertically long and flat chin (i.e., a limited projection of the pogonion). If the Robin sequence was present at birth, a degree of microgenia will likely be a component of the deficiency (see Chapter 4).
5. Mandibular dysplasia. True mandibular prognathism in the patient with ICP is not common, but it may be seen more frequently among patients with certain ethnic backgrounds (e.g., Asian). A degree of mandibular retrognathism as a residual aspect of the Robin sequence is likely. This often occurs in combination with a degree of maxillary deficiency and clockwise rotation of the maxillomandibular complex. The occlusion may be satisfactory with orthodontic compensation; however, the maxillomandibular horizontal deficiency with clockwise rotation is aesthetically obvious, and it may also negatively affect the upper airway (see Ch. 26).
6. Nasal obstruction and sinus blockage. Obstructed breathing through the nose and intermittent sinusitis are frequent in the individual who is born with ICP. This may result from a combination of septal deviation and enlarged inferior turbinates. An in-place pharyngoplasty (e.g., a superiorly based flap, a sphincteroplasty) may also be a cause of partial nasopharyngeal obstruction. These findings will also predispose these patients to obstructive sleep apnea (see Chapter 26).
7. Velopharyngeal dysfunction. It has been documented that approximately 20% of individuals with a repaired cleft palate will demonstrate velopharyngeal insufficiency by the time that they are 5 years old. The adolescent with ICP who is arriving for the evaluation of a cleft jaw deformity may have a pharyngoplasty in place. The Le Fort I osteotomy with advancement is likely to improve the upper airway, but it may negatively affect velopharyngeal function (see Chapter 8).
Orthodontic Considerations in the Patient with Isolated Cleft Palate with a Jaw Deformity
A primary goal of presurgical orthodontic treatment in the teenager with an ICP jaw deformity is to eliminate all existing dental compensations. Instituting camouflage treatment is likely to jeopardize periodontal health, lead to dental relapse, and it may also cause root resorption (see Chapter 5).
Immediate Presurgical Assessment
When approaching the time of surgery, updated records are obtained, including alginate impressions of the maxillary and mandibular arches, a centric relation bite registration, a face-bow registration, and facial measurements. The patient’s medical and dental records are reviewed, including radiographs; dental models; photographs of the face and the occlusion; and special studies. Decisions are made with regard to the preferred changes (i.e., repositioning) of the jaws and the precise millimeter distances and angles required in each jaw to achieve the desired result (see Chapter 12).59,60 Analytic model planning is carried out on the articulated dental casts, and splints are constructed. The splints assist with the achievement of the precise occlusion and the preferred facial aesthetics that were determined preoperatively (see Chapter 13).
Orthognathic Surgical Approach for Isolated Cleft Palate
Evolution of Surgical Techniques
In general, the primary jaw deformity observed in the adolescent with ICP is maxillary hypoplasia or dysplasia as a result of the original cleft deformity and the subsequent surgical interventions.31,32 The usual reconstructive procedure to consider is a Le Fort I maxillary osteotomy.20,28,30,47,53,56,92 Obwegeser showed that a circumvestibular incision with the separation of the pterygoid maxillary sutures followed by down-fracture and the disimpaction of the maxilla was not only possible but clinically relevant.66–70 This allowed the maxilla to be moved in any direction, either as one unit or in segments. Obwegeser clarified that full mobilization of the down-fractured maxilla was essential to the achievement of an orthognathic correction on the operating room table and to the limiting of skeletal relapse over time. Bell and others validated the use of the Obwegeser Le Fort I technique to allow for adequate blood supply for routine satisfactory bone healing without aseptic necrosis or dental injury (see Chapter 2).3,4,7,21–24
Current Operative Technique
The surgical technique for management of the maxillary deformity involves a standard circumvestibular incision and Le Fort I osteotomy (see Chapter 15).75–81,83,84 In the patient with ICP, the soft-tissue dissection may be difficult just before down-fracture as a result of the scarring of the nasal mucosa to the palatal tissue. There will be a need to sharply separate the oral and nasal layers completely during the down-fracture procedure. Note that this is not a contraindication to maxillary surgery but rather just a technical point. Care is taken to prevent the subperiosteal dissection (i.e., separation) of the palatal mucosa from the underlying hard palate, because this would compromise circulation to the down-fractured maxilla. Although it is of interest, the presence of a pharyngeal flap generally does not alter the surgical approach. This author has not found it necessary to section an in-place flap to accomplish the planned surgical objectives.
Residual palatal oronasal fistulas in the patient with ICP will be difficult to close simultaneously with the Le Fort I procedure; the elevation and transposition of palatal flaps are generally required to do so, and this would compromise the blood supply to the down-fractured maxilla. Interestingly, if a water-tight nasal side closure can be achieved through the down-fractures before the maxilla is fixed in its new location, then the residual palatal side mucosa separation will frequently heal by secondary intention. However, if a palatal fistula remains, it can be closed 6 months to 1 year after the orthognathic procedure, either with local palatal flaps or, if necessary, by using an anteriorly based dorsal tongue flap.82
The simultaneous management of secondary deformities frequently requires bilateral sagittal split osteotomies of the mandible and an oblique osteotomy of the chin. If removal of impacted wisdom teeth is recommended for long-term dental health this is accomplished at the same time. If septoplasty or inferior turbinate reduction or both are required to improve nasal airflow, then the procedures are also carried out simultaneously (see Chapter 10).
Orthognathic Surgery for Isolated Cleft Palate: Review of Study
In a previously published study, we assessed initial and long-term skeletal stability after Le Fort I osteotomy in 14 skeletally mature patients with ICP who underwent palate repair during infancy and who then presented as adolescents with maxillary dysplasia and malocclusion.83
Patient and Methods
In a study by Posnick and colleagues, the medical records, longitudinal cephalometric radiographs, and current clinical examinations of all patients with ICP who underwent Le Fort I osteotomy over a 3-year period by a single surgeon (Posnick) were reviewed.83 The following information was noted: all previous cleft and maxillofacial surgical procedures; stabilization techniques; the presence of a pharyngoplasty; the use of a bone graft; perioperative orthodontics; age at surgery; perioperative morbidity; and, at final follow up, the amount of overjet and overbite of the incisors. All patients were skeletally mature at the time of the operation. In all patients, lateral cephalograms were taken before surgery and at 3 to 7 days, 6 to 8 weeks, and 1 year postoperatively.
Controversies and Unresolved Issues
Skeletal Stability after Le Fort I Osteotomy
The study by Posnick and Taylor assessed the skeletal stability and relapse patterns in mature adolescents and young adults with ICP who underwent palate repair during infancy and who later developed maxillary dysplasia that required orthognathic surgery for the improvement of facial balance, the airway and the occlusion.83 Interestingly, the skeletal stability in the patients with ICP after Le Fort I osteotomy was somewhat better than that documented in patients with unilateral cleft lip and palate. Posnick and Taylor’s study confirm that an in-place pharyngoplasty does not contribute to relapse or increase perioperative morbidity. Roughly half the measured horizontal and vertical relapse occurred during the first 6 weeks after the operation, and the remainder occurred during the rest of the first year. A long-term positive overjet and overbite was maintained in all patients.
The Standard Approach versus the Distraction Approach to Le Fort I Advancement
The use of a DO technique to reposition the maxilla gradually over several weeks into the preferred horizontal position and to then hold the maxilla in place with the DO appliance for several months during the consolidation phase is relatively inconvenient and costly to the patient, the family, and the health care system. It remains a distant second choice as compared with the standard approach when the surgeon is able to down-fracture the maxilla, adequately mobilize it, and then place it into the preferred position in the operating room. The standard approach originally described by Obwegeser during the 1960s and then continually refined offers a safe and effective way to manage most jaw deformities that occur in the patient with ICP.66–70 Despite two decades of use, the DO technique for maxillary advancement has not been shown to offer less morbidity or improved stability for the patient with a cleft jaw deformity.* It does not allow for the correction of the deformity during childhood, as many clinicians had initially hoped it would. No horizontal growth can be expected after a Le Fort I osteotomy is carried out, whether with a DO approach or a standard approach.17,36,46,73,74,95–98 The DO approach has not diminished the occasional occurrence of velopharyngeal insufficiency after Le Fort I osteotomy, and it has not eliminated the problem of skeletal relapse.12,13,35,37,50,54,58,61,72,89,94 Alternatively, the DO approach is useful in unusual circumstances, when the surgeon is not able to adequately mobilize and fully advance the maxilla as planned in the operating room. For patients of special concern, the surgeon may wish to discuss the DO option before the Le Fort I advancement occurs. If the surgeon is unable to sufficiently mobilize and reposition the maxilla with the use of standard techniques, then a DO appliance can be placed (see Chapter 32).
Closure of Large Residual Palatal Fistula
When a recalcitrant large oronasal fistula at the incisal foramen region remains in a patient with ICP, palatal flaps alone may not be adequate for closure. In these cases, options are limited. This author often suggests achieving nasal side closure with the use of local full-thickness palatal (turnover) flaps and then obtaining oral side closure by elevating and placing an anteriorly based dorsal tongue flap. The tongue flap will provide needed vascularized soft tissue for effective fistula closure on the oral side.82 This approach does require the sacrifice of a small portion of the tongue donor site, a second general anesthetic, and downtime for the patient during the initial convalescence period (see Figure 34-4 and 34-5).
References
1. Aksu, M, Saglam-Aydinatay, B, Akcan, CA, et al. Skeletal and dental stability after maxillary distraction with a rigid external device in adult cleft lip and palate patients. J Oral Maxillofac Surg. 2010; 68:254–259.
2. Araujo, A, Schendel, SA, Wolford, IM, et al. Total maxillary advancement with and without bone grafting. J Oral Surg. 1978; 36:849.
3. Bell, WH, Fonseca, RJ, Kennedy, JW, III., et al. Bone healing and revascularization after total maxillary osteotomy. J Oral Surg. 1975; 33:253.
4. Bell, WH. Le Fort I osteotomy for correction of maxillary deformities. J Oral Surg. 1975; 33:412.
5. Berkowitz, S. State of the art in cleft palate or facial growth and dentistry: A historical perspective. Am J Orthod. 1978; 74:564–576.
6. Bishara, SE. Cephalometric evaluation of facial growth in operated and nonoperated individuals with isolated clefts of the palate. Cleft Palate J. 1973; 3:239–245.
7. Bloomquist, DS. Intraoperative assessment of maxillary perfusion during Le Fort I osteotomy [discussion]. J Oral Maxillofac Surg. 1994; 52:831.
8. Braun, TW, Sotereanos, GC. Orthognathic and secondary cleft reconstruction of adolescent patients with cleft palate. J Oral Surg. 1980; 38:425.
9. Braun, TW, Sotereanos, GC. Orthognathic surgical reconstruction of cleft palate deformities in adolescents. J Oral Surg. 1981; 39:255.
10. Canady, JW, Thompson, SA, Colburn, A. Craniofacial growth after iatrogenic cleft palate repair in a fetal bovine model. Cleft Palate Craniofac J. 1997; 34:69.
11. Capelozza Filho, L, Normando, AD, da Silva Filho, OG. Isolated influences of lip and palate surgery on facial growth: Comparison of operated and unoperated male adults with UCL/P. Cleft Palate Craniofac J. 1996; 33:51–56.
12. Chanchareonsook, N, Samman, N, Whitehill, TL. The effect of cranio-maxillofacial osteotomies and distraction osteogenesis on speech and velopharyngeal status: A critical review. Cleft Palate Craniofac J. 2006; 43:477–487.
13. Chanchareonsook, N, Whitehill, TL, Samman, N. Speech outcome and velopharyngeal function in cleft palate: Comparison of Le Fort I maxillary osteotomy and distraction osteogenesis—early results. Cleft Palate Craniofac J. 2007; 44:23–32.
14. Chen, ZQ, Qian, YF, Wang, GM, Shen, G. Sagittal maxillary growth in patients with unoperated isolated cleft palate. Cleft Palate Craniofac J. 2009; 46:664–667.
15. Cheung, LK, Chua, HD. A meta-analysis of cleft maxillary osteotomy and distraction osteogenesis. Int J Oral Maxillofac Surg. 2006; 35:14.
16. Cho, BC, Kyung, HM. Distraction osteogenesis of the hypoplastic midface using a rigid external distraction system: The results of a one- to six-year follow-up. Plast Reconstr Surg. 2006; 118:1201.
17. Correa Normando, AD, da Silva Filho, OG, Capelozza Filho, L. Influence of surgery on maxillary growth in cleft lip and/or palate patients. J Craniomaxillofac Surg. 1992; 20:111.
18. David, DJ, Anderson, PJ, Schnitt, DE, et al. From birth to maturity: A group of patients who have completed their protocol management. Part II. Isolated cleft palate. Plast Reconstr Surg. 2006; 117:515–526.
19. DeLuke, DM, Marchand, A, Robles, EC, Fox, P. Facial growth and the need for orthognathic surgery after cleft palate repair: Literature review and report of 28 cases. J Oral Maxillofac Surg. 1997; 55:694–698.
20. Des Prez, JD, Kiehn, CL. Surgical positioning of the maxilla. Symposium on management of cleft lip and palate and associated deformities. Am Plast Reconstr Surg. 1974; 8:222.
21. Dodson, TB, Neuenschwander, MC, Bays, RA. Intraoperative assessment of maxillary perfusion during Le Fort I osteotomy. J Oral Maxillofac Surg. 1994; 52:827.
22. Dodson, TB, Neuenschwander, MC. Maxillary perfusion during Le Fort I osteotomy after ligation of the descending palatine artery. J Oral Maxillofac Surg. 1997; 55:51.
23. Drommer, R. The history of the “Le Fort I-Osteotomy. ”. J Maxillofac Surg. 1986; 14:119–122.
24. Drommer, R, Luhr, HG. The stabilization of osteotomized maxillary segments with Luhr miniplates in secondary cleft surgery. J Maxillofac Surg. 1981; 9:166–169.
25. Figueroa, AA, Polley, JW, Friede, H, et al. Long-term skeletal stability after maxillary advancement with distraction osteogenesis using a rigid external distraction device in cleft maxillary deformities. Plast Reconstr Surg. 2004; 114:1382.
26. Figueroa, AA, Polley, JW, Ko, EW. Maxillary distraction for the management of cleft maxillary hypoplasia with a rigid external distraction system. Semin Orthod. 1999; 5:46.
27. Filho, LC. Isolated influences of lip and palate surgery on facial growth: Comparison of operated and unoperated male adults. Cleft Palate Craniofac J. 1996; 33:51.
28. Fitzpatrick, B. Mid-face osteotomy in the adolescent cleft patient. Aust Dent J. 1977; 22:338.
29. Freihofer, HPM, Jr. Results of osteotomies of the facial skeleton in adolescence. J Maxillofac Surg. 1977; 5:267.
30. Georgiade, NG. Mandibular osteotomy for the correction of facial disproportion in the cleft lip and palate patient. Symposium on management of cleft lip and palate and associated deformities. Am Plast Reconstr Surg. 1974; 8:238.
31. Gillies, HD, Millard, DR, Jr. The principles and art of plastic surgery. Boston: Little, Brown; 1957.
32. Gillies, HD, Rowe, NL. L’ostéotomie du maxillaire supérieur enoisagée essentiellement dans le cas de bec-de-lièvre total. Rev Stomatol. 1954; 55:545–552.
33. Gnoinski, W. Early identification of candidates for corrective maxillary osteotomy in cleft lip and palate group. Scand J Plast Reconstr Surg Hand Surg. 1987; 21:39.
34. Good, PM, Mulliken, JB, Padwa, BL. Frequency of Le Fort I osteotomy after repaired cleft lip and palate or cleft palate. Cleft Palate Craniofac J. 2007; 44:396–401.
35. Guyette, TW, Polley, JW, Figueroa, A, Smith, BE. Changes in speech following maxillary distraction osteogenesis. Cleft Palate Craniofac J. 2001; 38:199–205.
36. Harada, K, Baba, Y, Ohyama, K, et al. Maxillary distraction osteogenesis for cleft lip and palate children using an external, adjustable, rigid distraction device: A report of 2 cases. J Oral Maxillofac Surg. 2001; 59:1492.
37. Harada, K, Ishii, Y, Ishii, M, et al. Effect of maxillary distraction osteogenesis on velopharyngeal function: A pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:538.
38. Hedemark, A, Freihofer, HP, Jr. The behavior of the maxilla in vertical movements after Le Fort I osteotomy. J Maxillofac Surg. 1978; 6:244.
39. He, D, Genecov, DG, Barcelo, R. Nonunion of the external maxillary distraction in cleft lip and palate: Analysis of possible reasons. J Oral Maxillofac Surg. 2010; 68:2402–2411.
40. Hierl, T, Hemprich, A. Callus distraction of the midface in the severely atrophied maxilla: A case report. Cleft Palate Craniofac J. 1999; 36:457.
41. Hirano, A, Suzuki, H. Factors related to relapse after Le Fort I maxillary advancement osteotomy in patients with cleft lip and palate. Cleft Palate Craniofac J. 2001; 38:1.
42. Hochban, W, Ganss, C, Austermann, KH. Long-term results after maxillary advancement in patients with clefts. Cleft Palate Craniofac J. 1993; 30:237–243.
43. Höltje, WJ, Scheuer, H. Skeletal stability and relapse patterns after Le Fort I osteotomy using miniplate fixation in patients with isolated cleft palate [discussion]. Plast Reconstr Surg. 1994; 94:59–60.
44. Horster, W. Experience with functionally stable plate osteosynthesis after forward displacement of the upper jaw. J Maxillofac Surg. 1980; 8:176.
45. Houston, WJB, James, DR, Jones, E, Kavvadia, S. Le Fort I maxillary osteotomies in cleft palate cases: Surgical changes and stability. J Craniomaxillofac Surg. 1989; 17:9–15.
46. Huang, CS, Harikrishnan, P, Liao, YF, et al. Long-term follow-up after maxillary distraction osteogenesis in growing children with cleft lip and palate. Cleft Palate Craniofac J. 2007; 44:274.
47. Hui, E, Hägg, EU, Tideman, H. Soft tissue changes following maxillary osteotomies in cleft lip and palate and non-cleft patients. J Craniomaxillofac Surg. 1994; 22:182–186.
48. Jackson, IT. Cleft and jaw deformities. Symposium on Reconstruction of Jaw Deformities. 1978; 113.
49. James, D, Brook, K. Maxillary hypoplasia in patients with cleft lip and palate deformity: The alternative surgical approach. Eur J Orthod. 1985; 7:231.
50. Janulewicz, J, Costello, BJ, Buckley, MJ, et al. The effects of Le Fort I osteotomies on velopharyngeal and speech functions in cleft patients. J Oral Maxillofac Surg. 2004; 62:308–314.
51. Jorgenson, RJ, Shapiro, SD, Odiner, KL. Studies on facial growth and arch size in cleft lip and palate. J Craniofac Genet Dev Biol. 1984; 4:33.
52. Kanno, T, Mitsugi, M, Hosoe, M, et al. Long-term skeletal stability after maxillary advancement with distraction osteogenesis in nongrowing patients. J Oral Maxillofac Surg. 2008; 66:1833–1846.
53. Kiehn, CL, DesPrez, JD, Brown, F. Maxillary osteotomy for late correction of occlusion and appearance in cleft lip and palate patients. Plast Reconstr Surg. 1968; 42:203.
54. Ko, EW, Figueroa, AA, Guyette, TW, et al. Velopharyngeal changes after maxillary advancement in cleft patients with distraction osteogenesis using a rigid external distraction device: 1-year cephalometric follow-up. J Craniofac Surg. 1999; 10:312–320.
55. Lu, D-W, Shi, B, Wang, H-J, Zheng, Q. The comparative study of craniofacial structural characteristic of individuals with different types of cleft palate. Ann Plast Surg. 2007; 59:382–387.
56. Luhr, HG. Zur stabilen osteosynthese bei unterkiefer-frakturen. Dtsch Zahnarztl Z. 1968; 23:754.
57. Luyk, NH, Ward-Booth, RP. The stability of the Le Fort I advancement osteotomies using bone plates without bone grafts. J Maxillofac Surg. 1985; 13:250.
58. Marrinan, EM, LaBrie, RA, Mulliken, JB. Velopharyngeal function in nonsyndromic cleft palate: Relevance of surgical technique, age at repair, and cleft type. Cleft Palate Craniofac J. 1998; 35:95–100.
59. McCance, AM, Moss, JP, Fright, WR, et al. Three-dimensional analysis techniques. Part 1: Three-dimensional soft-tissue analysis of 24 adult cleft palate patients following Le Fort I maxillary advancement: A preliminary report. Cleft Palate Craniofac J. 1997; 34:36.
60. McCance, AM, Orth, M, Moss, JP, et al. Three-dimensional analysis techniques. Part 4: Three-dimensional analysis of bone, and soft tissue to bone ratio of movements in 24 cleft patients following Le Fort I osteotomy: A preliminary report. Cleft Palate Craniofac J. 1997; 43:58–62.
61. McComb, R, Marrinan, E, Nuss, RC, et al. Predictors of velopharyngeal insufficiency after Le Fort I maxillary advancement in patients with cleft palate. J Oral Maxillofac Surg. 2011; 69:2226–2232.
62. McKinstry, RE. Cleft palate dental care: A historical perspective. Arlington, Va: ABI Publications; 2000.
63. Molina, F, Ortiz Monasterio, F, de la Paz Aguilar, M, Barrera, J. Maxillary distraction: Aesthetic and functional benefits in cleft lip-palate and prognathic patients during mixed dentition. Plast Reconstr Surg. 1998; 101:951.
64. Motohashi, N, Kuroda, T, Filho, LC, et al. P-A cephalometric analysis of nonoperated adult cleft lip and palate. Cleft Palate Craniofac J. 1994; 31:193.
65. Nanda, SK. Patterns of vertical growth in the face. Am J Orthod Dentofacial Orthop. 1988; 93:103–116.
66. Obwegeser, HL. Surgery as an adjunct to orthodontics in normal and cleft palate patients. Rep Congr Eur Orthod Soc. 1966; 42:343–353.
67. Obwegeser HL: Surgical correction of deformities of the jaws in adult cleft cases. Paper read at the First International Conference on Cleft Lip and Palate, Houston, Tex, April 14-17, 1969.
68. Obwegeser, HL. Surgical correction of small or retrodisplaced maxillae: The “dish-face” deformity. Plast Reconstr Surg. 1969; 43:351.
69. Obwegeser, HL. Surgical correction of maxillary deformities. In: Grabb WC, Rosenstein SW, Bzoch KR, eds. Cleft lip and palate. Boston: Little and Crown; 1971:515–556.
70. Obwegeser, HL, Lello, GE, Farmand, M, Correction of secondary cleft deformities. Surgical correction of dentofacial deformities. Bell, WH, eds. Surgical correction of dentofacial deformities; Vol III. Saunders, Philadelphia, 1985:592–638.
71. Perko, M. The history of treatment of cleft lip and palate. Prog Pediatr Surg. 1986; 20:238–251.
72. Phillips, JH, Klaiman, P, Delorey, R, MacDonald, DB. Predictors of velopharyngeal insufficiency in cleft palate orthognathic surgery. Plast Reconstr Surg. 2005; 115:681–686.
73. Polley, JW, Figueroa, AA. Management of severe maxillary deficiency in childhood and adolescence through distraction osteogenesis with an external, adjustable, rigid distraction device. J Craniofac Surg. 1997; 8:181.
74. Polley, JW, Figueroa, AA. Rigid external distraction: Its application in cleft maxillary deformities. Plast Reconstr Surg. 1998; 102:1360.
75. Posnick, JC, Orthognathic surgery in the cleft patient. Instructional courses. Russel, RC, eds. Instructional courses; 4. CV Mosby Co, St. Louis, 1991:129–157.
76. Posnick, JC. Orthognathic surgery for the cleft lip and palate patient. Semin Orthod. 1996; 2(3):205–214.
77. Posnick, JC. The treatment of secondary and residual dentofacial deformities in the cleft patient: Surgical and orthodontic therapy. Clin Plast Surg. 1997; 24(3):583–597.
78. Posnick, JC. Cleft-orthognathic surgery: The isolated cleft palate deformity. In: Posnick JC, ed. Craniofacial and maxillofacial surgery in children and young adults. Philadelphia: WB Saunders Co; 2000:951–978.
79. Posnick, JC. The staging of cleft lip and palate reconstruction: Infancy through adolescence. In: Posnick JC, ed. Craniofacial and maxillofacial surgery in children and young adults. Philadelphia: WB Saunders Co; 2000:785–826.
80. Posnick, JC, Agnihotri, N. Managing chronic nasal airway obstruction at the time of orthognathic surgery: A twofer. J Oral Maxillofac Surg. 2011; 69:695–701.
81. Posnick, JC, Ricalde, P. Cleft-orthognathic surgery. Clin Plast Surg. 2004; 31(2):315–330.
82. Posnick, JC, Ruiz, R. Repair of large anterior palatal fistulas using thin tongue flaps [discussion]. Ann Plast Surg. 2000; 45:114–117.
83. Posnick, JC, Taylor, M. Skeletal stability and relapse patterns after Le Fort I osteotomy using miniplate fixation in patients with isolated cleft palate. Plast Reconstr Surg. 1994; 94:51–58.
84. Posnick, JC, Tompson, B. Cleft-orthognathic surgery: Complications and long-term results. Plast Reconstr Surg. 1995; 96(2):255–266.
85. Rosenstein, SW. Facial growth and the need for orthognathic surgery after cleft palate repair: Literature review and report of 28 cases [discussion]. J Oral Maxillofac Surg. 1997; 55:698.
86. Ross, RB. The clinical implications of facial growth in the cleft lip and palate. Cleft Palate J. 1970; 7:37–47.
87. Shaw, WC, Asher-McDade, C, Brattstrom, V, et al. A six-center international study of treatment outcomes in patients with clefts of the lip and palate. Cleft Palate Craniofac J. 1992; 29:393.
88. Stoelinga, PJ, vd Vijver, HR, Leenen, RJ, et al. The prevention of relapse after maxillary osteotomies in cleft palate patients. J Craniomaxillofac Surg. 1987; 15:325.
89. Trindale, IE, Yamashita, RP, Suguimoto, RM, et al. Effects of orthognathic surgery on speech and breathing of subjects with cleft lip and palate: Acoustic and aerodynamic assessment. Cleft Palate Craniofac J. 2003; 40:54–64.
90. Will, LA. Growth and development in patients with untreated clefts. Cleft Palate Craniofac J. 2000; 37:523–526.
91. Williams, AC, Bearn, D, Mildinhall, S, et al. Cleft lip and palate care in the United Kingdom—the Clinical Standards Advisory Group (CSAG) study. Part 2: Dentofacial outcomes and patient satisfaction. Cleft Palate Craniofac J. 2001; 38:24–29.
92. Willmar, K. On Le Fort I osteotomy: A follow-up study of 106 operated patients with maxillofacial deformity. Scand J Plast Reconstr Surg. 1974; 12(Suppl 1):1–68.
93. Wiltfang, J, Hirschfelder, U, Neukam, FW, et al. Long-term results of distraction osteogenesis of the maxilla and midface. Br J Oral Maxillofac Surg. 2002; 40:473.
94. Witzel, MA, Munro, IR. Velopharyngeal insufficiency after maxillary advancement. Cleft Palate J. 1977; 14:176.
95. Wolford, LM. Effects of orthognathic surgery on nasal form and function in the cleft patient. Cleft Palate Craniofac J. 1992; 29:546–555.
96. Wolford, LM, Cassano, DS, Cottrell, DA, et al. Orthognathic surgery in the young cleft patient: Preliminary study on subsequent facial growth. J Oral Maxillofac Surg. 2008; 66:2524–2536.
97. Wolford, LM, Karras, SC, Mehra, P. Considerations for orthognathic surgery during growth: Part 1. Mandibular deformities. Am J Orthod Dentofacial Orthop. 2001; 119:95.
98. Wolford, LM, Karras, SC, Mehra, P. Considerations for orthognathic surgery during growth: Part 2. Maxillary deformities. Am J Orthod Dentofacial Orthop. 2001; 119:102.
99. Yoshida, H, Nakamura, A, Michi, K, et al. Cephalometric analysis of maxillofacial morphology in unoperated cleft palate patients. Cleft Palate Craniofac J. 1992; 29:419–424.


