CHAPTER 2 Classical Patient Selection for Unicondylar Knee Arthroplasty
 The patient must be able to indicate the location of the knee pain along the medial joint line in the varus knee.
The patient must be able to indicate the location of the knee pain along the medial joint line in the varus knee. The physical examination of the knee must confirm the location of the tenderness along the medial joint line with minimal to no tenderness in all other areas.
The physical examination of the knee must confirm the location of the tenderness along the medial joint line with minimal to no tenderness in all other areas.Introduction
Unicondylar knee arthroplasty (UKA) has progressed through two separate time phases since the original designs were developed in the early 1970s. The first phase was fraught with problems related to the prosthetic designs and patient selection.1–4 The results were good to excellent for the first 10 years after the surgery in the hands of the designing surgeons. In the second decade the results did tend to taper off and were not as good as the reports of total knee arthroplasty (TKA).5,6 It was difficult for the standard orthopaedic surgeon to reproduce the findings of the designers, and interest decreased in the late 1980s and early 1990s. Insall’s data showed that only 6% of knees satisfied the criteria for UKA, and he favored TKA as the procedure of choice.7
Repicci introduced the limited surgical approach (minimally invasive surgery, or MIS) for UKA in the early 1990s, and interest in the procedure increased by the year 2000.8–13 Newer designs appeared, and the Oxford mobile-bearing UKA became very popular both in Europe and in the United States.14,15 With this new wave of interest, surgeons looked to improve the clinical results and reviewed the patient selection criteria, the surgical approach, and instruments. If the incorrect patient is chosen, the result will be compromised despite excellent surgical technique and prosthetic design. This chapter outlines the factors involved in the choice process that should lead to a more satisfactory overall result.
Physical Examination
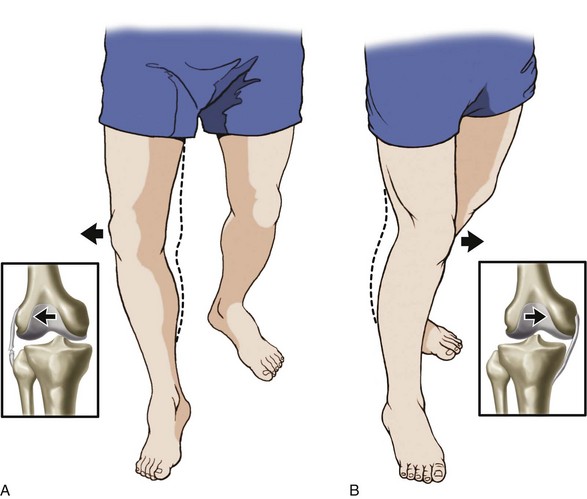
The examination should include inspection of the gait and, then, the full evaluation of both lower extremities. There should be a component of antalgia to the gait, and any thrust of the femur on the tibia through the stance phase should especially be noted. As the deformity progresses either in the varus or the valgus knee, the collateral ligament on the compressed side of the joint shortens and the ligament on the tension side lengthens. This ultimately leads to shifting of the tibia beneath the femur with impingement of the lateral tibial spine against the lateral femoral condyle in the varus knee and impingement of the medial tibial spine against the medial femoral condyle in the valgus knee (Fig. 2–1). The shift of the tibia correlates with a lateral thrust of the femur on the tibia through the stance phase of gait in the varus knee and a medial thrust in the valgus knee (Fig. 2–2). This finding is a relative contraindication to UKA and should alert the examiner to correlate the physical finding with the standing anteroposterior radiograph.
If the deformity is fixed and greater than 5°, the tibial cut will be deeper in order to accommodate the prosthetic thickness. This deeper cut can lead to increased loss of bone and metaphyseal fracture (Fig. 2–3). The valgus deformity can be as great as 10° but should correct passively to 5°.
Imaging Studies
The primary imaging tool is the standing full-length radiograph. This allows the examiner to determine the mechanical axis of the limb and the associated joint space narrowing on the medial or lateral aspect of the joint. It is valuable to measure both the anatomic axis and the mechanical axis. There should be no greater than 5° of anatomic varus and 10° of valgus (Fig. 2–4). This should correlate with the physical examination findings. Translocation of the tibia beneath the femur on the standing view indicates that the disease is progressing with involvement of the opposite compartment (see Fig. 2–1). As such, it is a relative contraindication. The anteroposterior flexed view will show more detail of the posterior femoral condyles within the notch, and the posteroanterior flexed view will give more details about the loss of joint space on either the medial or lateral side. The lateral view will show the extent of patellofemoral disease, and if there is more than mild involvement, the patient should be examined and interviewed again to be sure that there are minimal symptoms attributable to this joint. In a similar fashion, there should be limited involvement of the opposite femorotibial joint on the radiograph, and this should also correlate with the history and physical examination. There is no doubt that there will always be a certain degree of arthritic disease in the entire knee; however, the primary involvement should be the medial or lateral femorotibial joint.
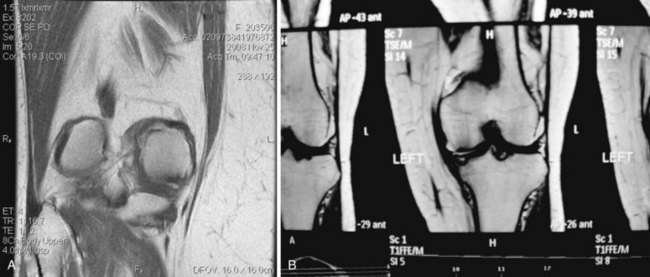
Magnetic resonance imaging (MRI) has become a very common tool for evaluation of the knee. Oftentimes, this study is requested before any radiographs are completed, and this is a mistake in the diagnostic chain. However, there are times when the MRI is valuable in combination with the appropriate radiographs. Sudden onset of distinct pain on the medial aspect of the knee often correlates with avascular necrosis, and it is important to make this diagnosis. If the event is recent, there will be hemorrhage into the medial femoral condyle or (less commonly) into the medial tibial metaphyseal area (Fig. 2–5). It is important to allow this early event to progress and mature with protected weight bearing before considering any UKA. If the hemorrhage is in the early phases, surgical intervention may lead to extensive loss of bone in the involved area and may require a TKA with complex augments to make up for the bone loss. After the avascular necrosis has matured, the remaining defect will be quite evident and it is usually surrounded by sclerotic bone that is much more amenable to UKA. On occasion, the patient may present with joint line pain medially and instability that may be secondary to pathology in the opposite lateral compartment. The author does not favor routine arthroscopy at the time of the UKA and does not favor routine MRI studies. However, MRI is a good tool to evaluate the lateral compartment and the lateral meniscus when there is a significant clinical suspicion. If the lateral meniscus is torn and the lateral compartment is also arthritic on the MRI, the surgeon should rethink the UKA and consider TKA.
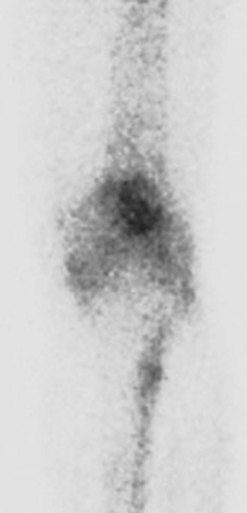
Computed tomography or arthrography of the knee are both infrequent studies but may be considered when a patient has a pacemaker and cannot undergo MRI evaluation. Technetium scans of the knee are sometimes valuable to pinpoint the area of primary arthritic involvement and also allow a visual comparison to the other areas of the knee (Fig. 2–6).
Conclusions
The results of UKA can be equally successful as TKA if the correct indications are followed.10 In a busy practice, UKA can represent 10–15% of the operative knee arthroplasty cases. It is extremely important to combine all three arms of the evaluation: history, physical examination, and imaging. If any one of these is questionable, it is best to abandon the UKA and consider TKA. However, if there are only relative contraindications in each of the three areas, the UKA can be performed with excellent results. The hesitant surgeon will often find reasons to abandon the UKA when the patient may very well be an excellent case for the surgery. The author has never abandoned the UKA during the operative procedure, and all decisions should be made well before the surgical procedure so that both the surgeon and the patient will be well prepared for the postoperative management and therapy.
1 Marmor L. Marmor modular knee in unicompartmental disease: minimum four-year follow-up. J Bone Joint Surg [Am]. 1979;61:347-353.
2 Insall J, Walker P. Unicondylar knee replacement. Clin Orthop Relat Res. 1976;120:83-85.
3 Laskin RS. Unicompartment tibiofemoral resurfacing arthroplasty. J Bone Joint Surg [Am]. 1978;60:182-185.
4 Goodfellow J, O’Connor J. The mechanics of the knee and prosthesis design. J Bone Joint Surg [Br]. 1978;60:358-369.
5 Marmor L. Unicompartmental arthroplasty of the knee with a minimum of 10-year follow-up. Clin Orthop Relat Res. 1988;228:171-177.
6 Scott RD, Cobb AG, McQueary FG, Thornhill TS. Unicompartmental knee arthroplasty: eight to twelve year follow-up with survivorship analysis. Clin Orthop Relat Res. 1991;271:96-100.
7 Stern SH, Becker MW, Insall J. Unicompartmental knee arthroplasty: an evaluation of selection criteria. Clin Orthop Relat Res. 1993;286:143-148.
8 Repicci JA, Eberle RW. Minimally invasive surgical technique for unicondylar knee arthroplasty. J South Orthop Assoc. 1999;8(1):20-27.
9 Romanowski MR, Repicci JA. Minimally invasive unicondylar arthroplasty: eight year follow-up. J Knee Surg. 2002;15:17-22.
10 Berger RA, Nedeff DD, Barden RN, et al. Unicompartmental knee arthroplasty. Clin Orthop Relat Res. 1999;367:50-60.
11 Svard UCG, Price AJ. Oxford medial unicompartmental knee arthroplasty: a survival analysis of an independent series. J Bone Joint Surg [Br]. 2001;83:191-194.
12 Price AJ, Webb J, Topf H, et al. and the Oxford Hip and Knee Group. Rapid recovery after Oxford Unicompartmental Arthroplasty through a short incision. J Arthroplasty. 2001;16:970-976.
13 Gesell MW, Tria AJ. MIS unicondylar knee arthroplasty: surgical approach and early results. Clin Orthop Rel Res. 2004;428:53-60.
14 Beard DJ, Pandit H, Gill HS, et al. The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Joint Surg [Br]. 2007;89:1597-1601.
15 Beard DJ, Pandit H, Ostlere S, et al. Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg [Br]. 2007;89:1602-1607.