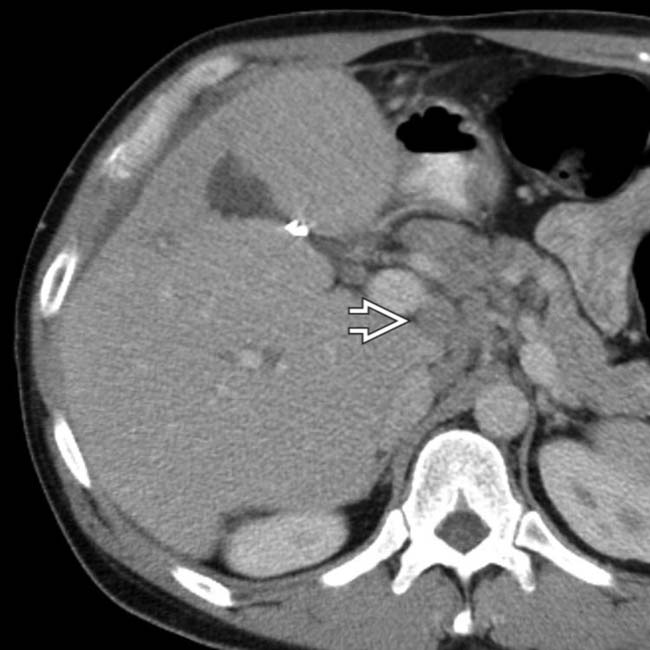
Hyperdense on NECT, isodense on CECT
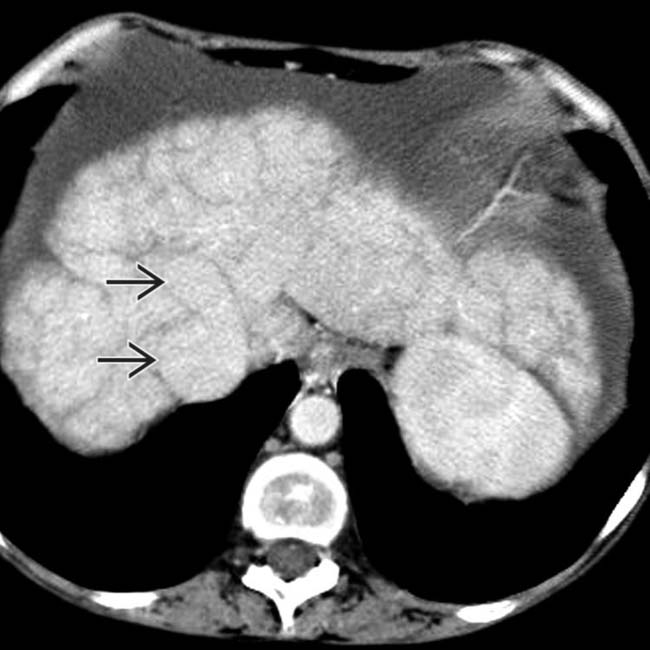
 to the edges of the caudate and right lobes, respectively. Note the bands of fibrosis
to the edges of the caudate and right lobes, respectively. Note the bands of fibrosis  and ascites.
and ascites.
 . Note the enlarged caudate lobe
. Note the enlarged caudate lobe  , which is as wide as the right lobe, although the caudate lobe is normally no more than 60% of the width of the right lobe.
, which is as wide as the right lobe, although the caudate lobe is normally no more than 60% of the width of the right lobe.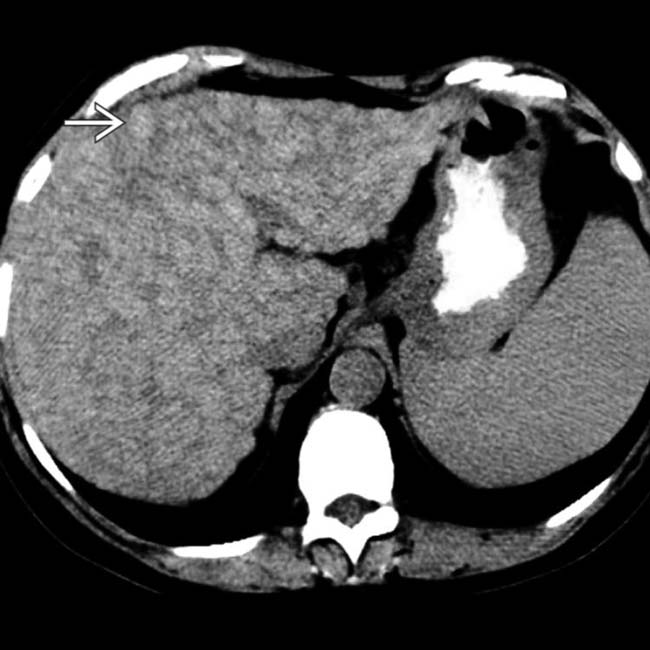
 , surrounded by lace-like fibrosis.
, surrounded by lace-like fibrosis.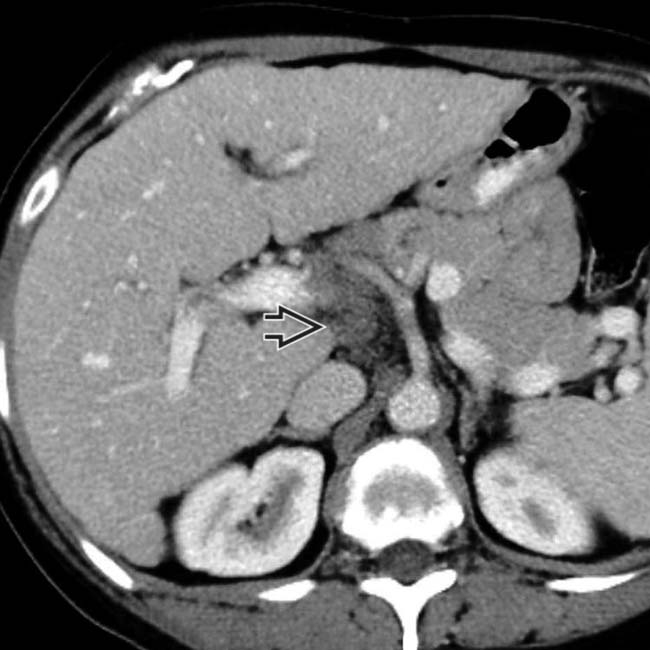
 , another typical feature of primary biliary cirrhosis, is also noted. Primary biliary cirrhosis is an autoimmune disease that typically affects women in their 5th or 6th decade.
, another typical feature of primary biliary cirrhosis, is also noted. Primary biliary cirrhosis is an autoimmune disease that typically affects women in their 5th or 6th decade.IMAGING
General Features
CT Findings
• Vascular derangements
PATHOLOGY
General Features
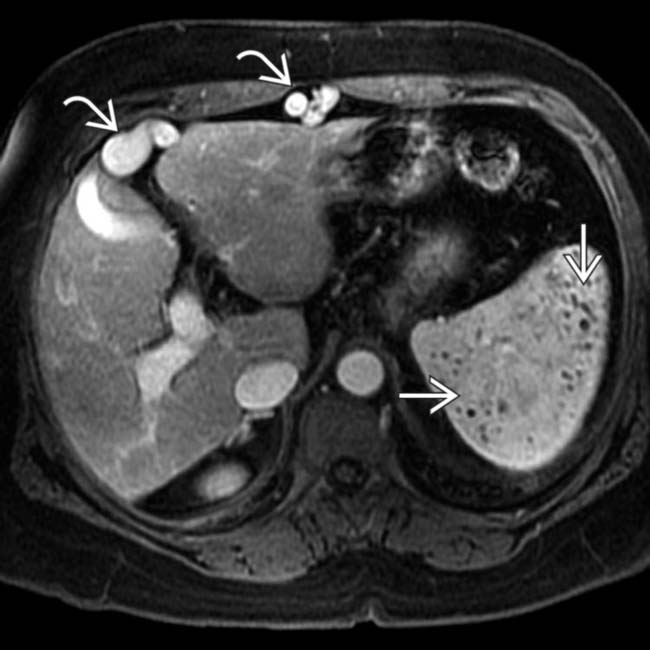
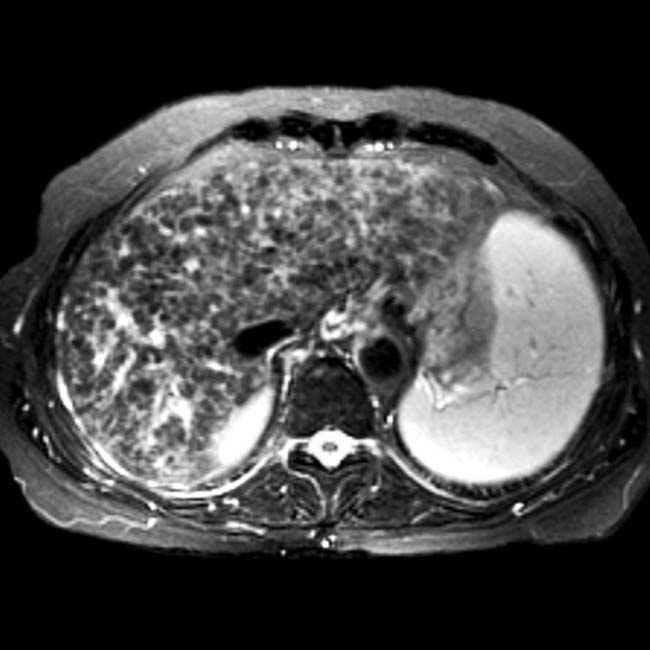
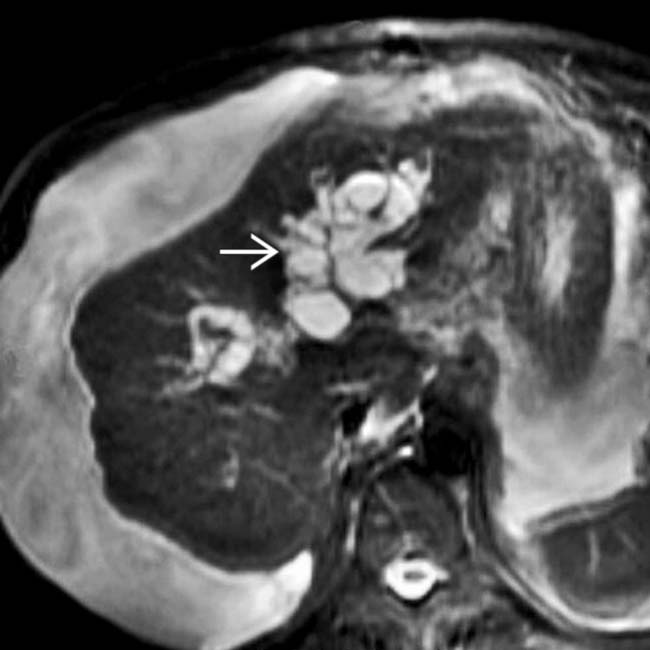
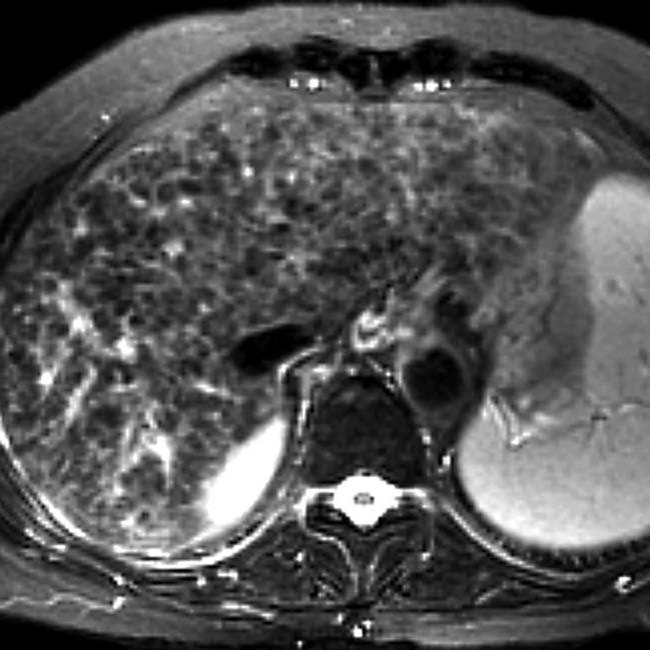
 . Within the spleen are innumerable small lesions that are especially evident as hypointense foci on this GRE T1WI contrast-enhanced image
. Within the spleen are innumerable small lesions that are especially evident as hypointense foci on this GRE T1WI contrast-enhanced image  , representing Gamna-Gandy bodies.
, representing Gamna-Gandy bodies.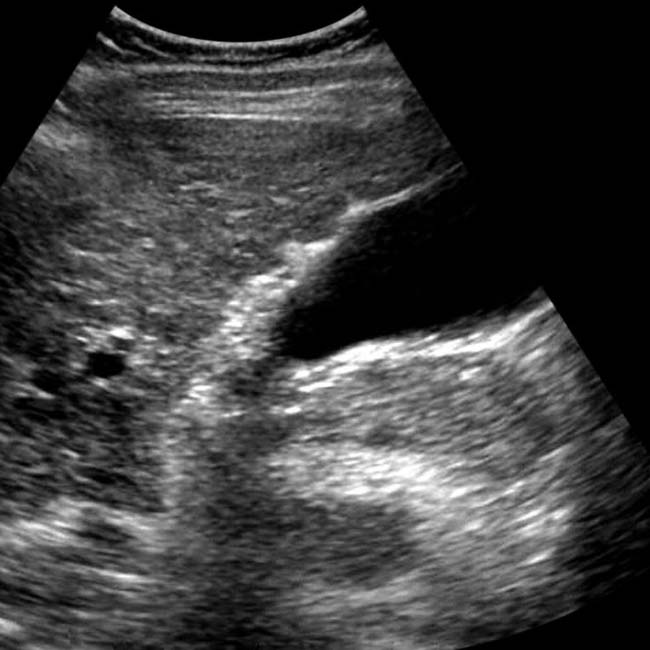

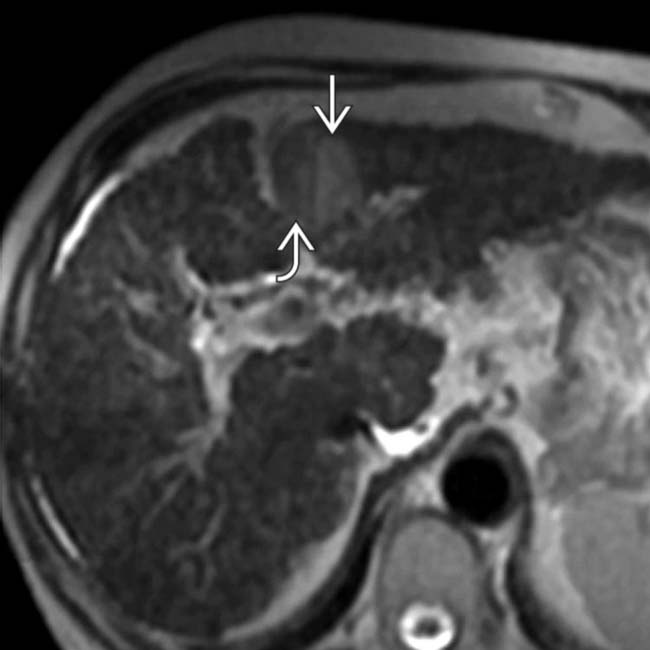
 . The intrahepatic ducts
. The intrahepatic ducts  are dilated with an abnormal arborization, suggestive of PSC.
are dilated with an abnormal arborization, suggestive of PSC.

 that was isodense to the liver on all other phases. This lesion was not evident on repeat CT or MR over the next 2 years and presumably represents a small arterioportal shunt.
that was isodense to the liver on all other phases. This lesion was not evident on repeat CT or MR over the next 2 years and presumably represents a small arterioportal shunt.
 .
.
 in cardiophrenic regions. The intrahepatic ducts are not dilated but were found to be beaded and strictured on ERCP.
in cardiophrenic regions. The intrahepatic ducts are not dilated but were found to be beaded and strictured on ERCP.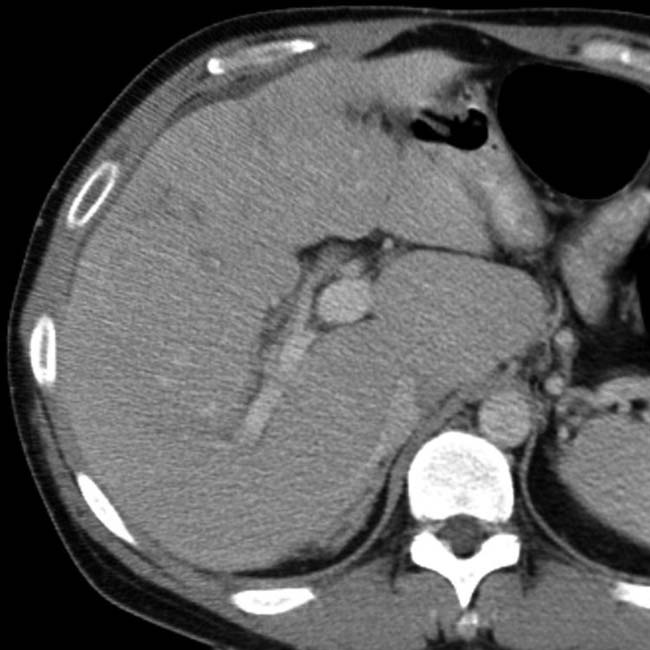
 .
.
 . Unrecognized or untreated right heart failure or constrictive pericarditis can lead to acute or irreversible hepatic damage.
. Unrecognized or untreated right heart failure or constrictive pericarditis can lead to acute or irreversible hepatic damage.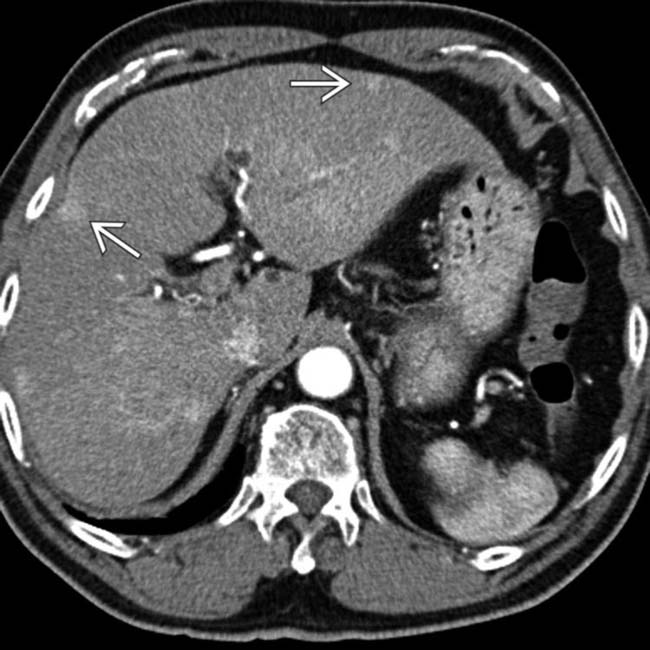
 .
.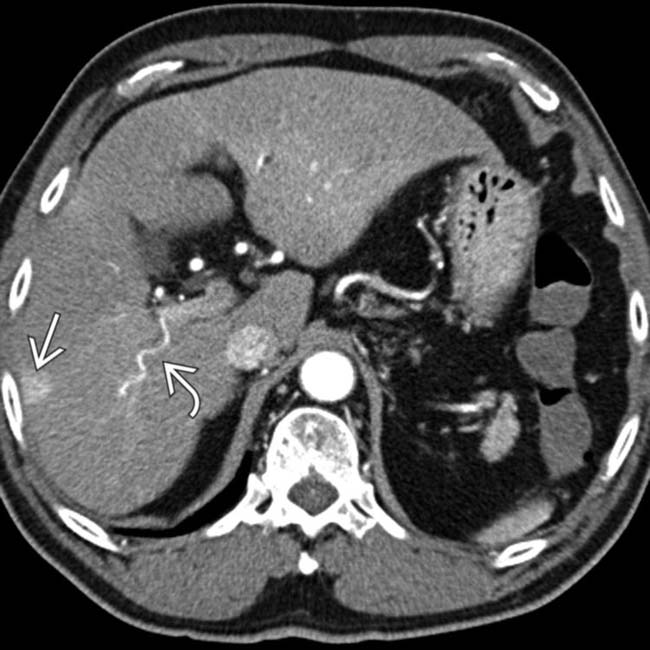
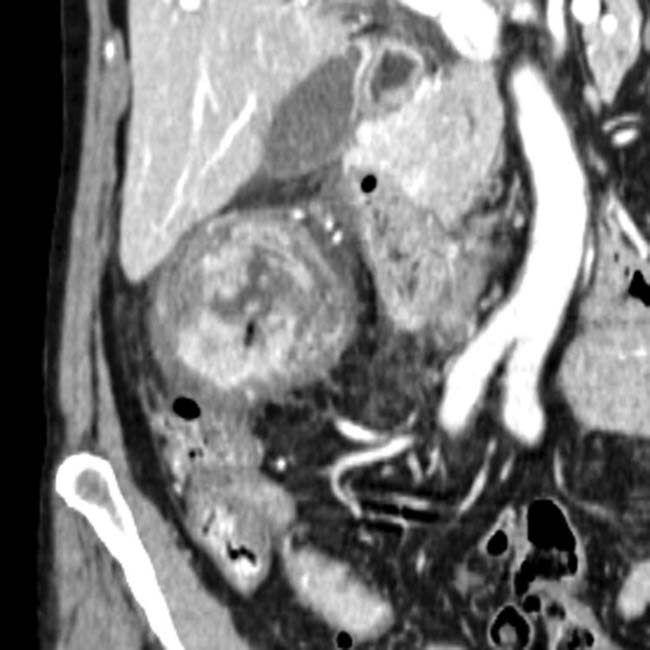
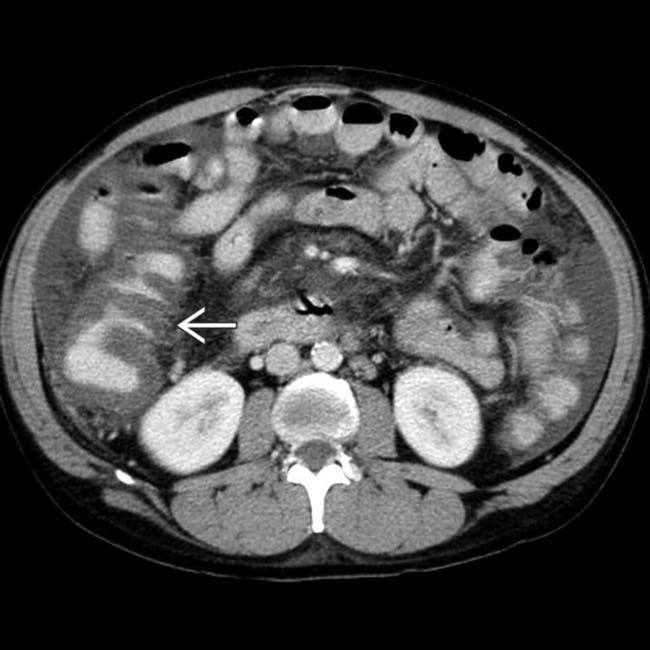
 . Also note the “corkscrew” enlarged hepatic arterial branch
. Also note the “corkscrew” enlarged hepatic arterial branch  and the widened fissures, all typical of cirrhosis.
and the widened fissures, all typical of cirrhosis.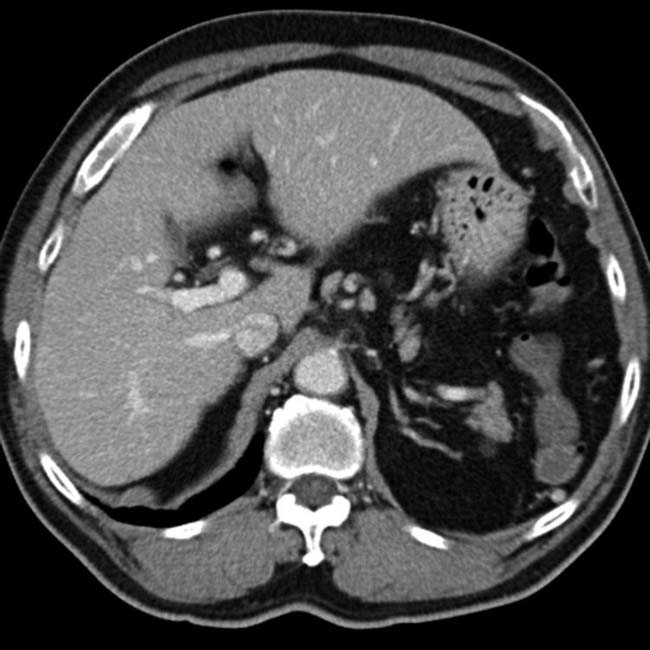
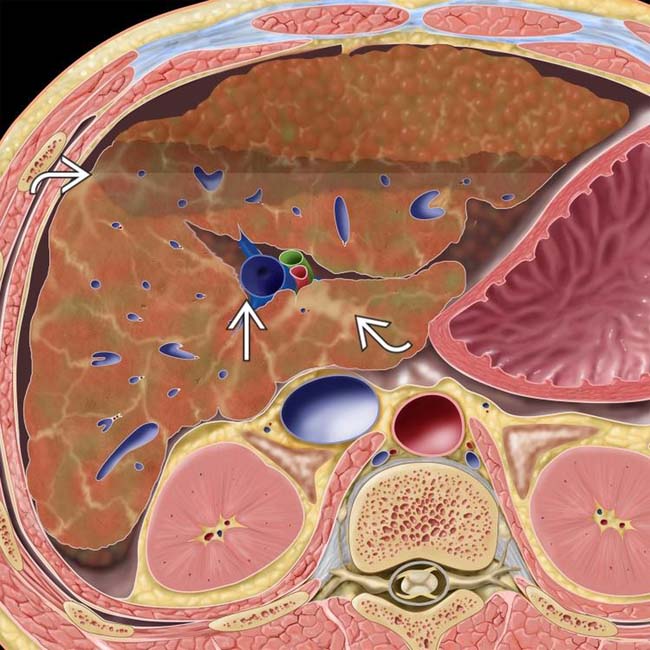
 that do not arborize (branch) as bile ducts and are spherical in shape, representing peribiliary cysts.
that do not arborize (branch) as bile ducts and are spherical in shape, representing peribiliary cysts.
 are surrounded by a collar of low density, some of which probably represent periportal edema. However, there are also discrete low-density focal lesions
are surrounded by a collar of low density, some of which probably represent periportal edema. However, there are also discrete low-density focal lesions  that represent periportal cysts.
that represent periportal cysts.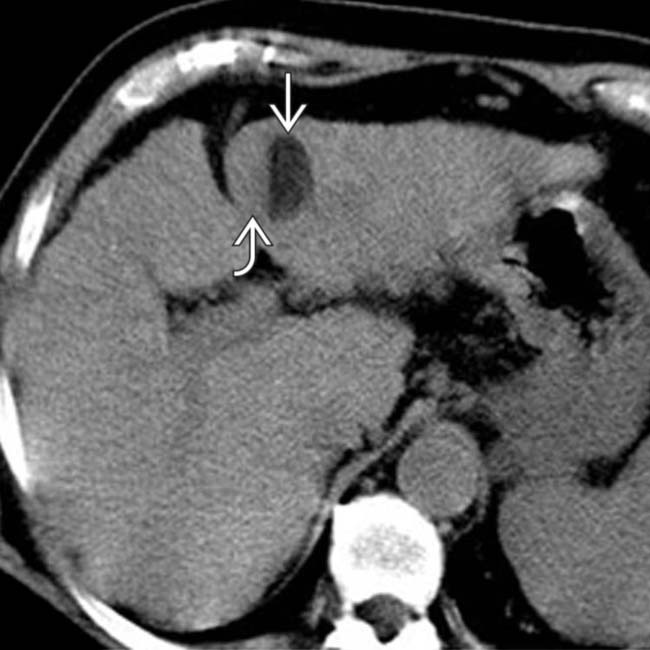
 and a soft tissue-density right half
and a soft tissue-density right half  .
.
 and only relatively hyperintensity within the right lateral component
and only relatively hyperintensity within the right lateral component  .
.
 , while the other portion of the lesion shows relatively bright signal
, while the other portion of the lesion shows relatively bright signal  on this non-fat-suppressed T2WI.
on this non-fat-suppressed T2WI.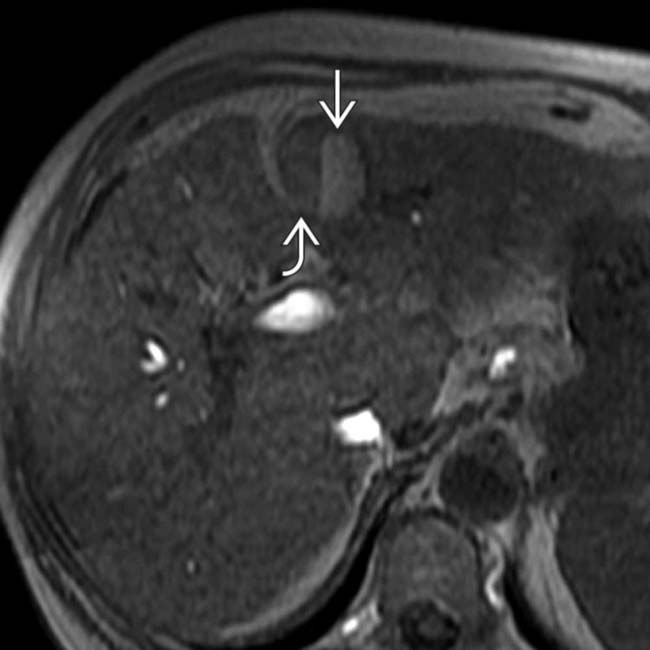
 is hyperintense and represents HCC, while the other half of the nodule is hypointense and is a dysplastic nodule
is hyperintense and represents HCC, while the other half of the nodule is hypointense and is a dysplastic nodule  .
.
 , which is strongly suggestive of HCC in a cirrhotic liver.
, which is strongly suggestive of HCC in a cirrhotic liver.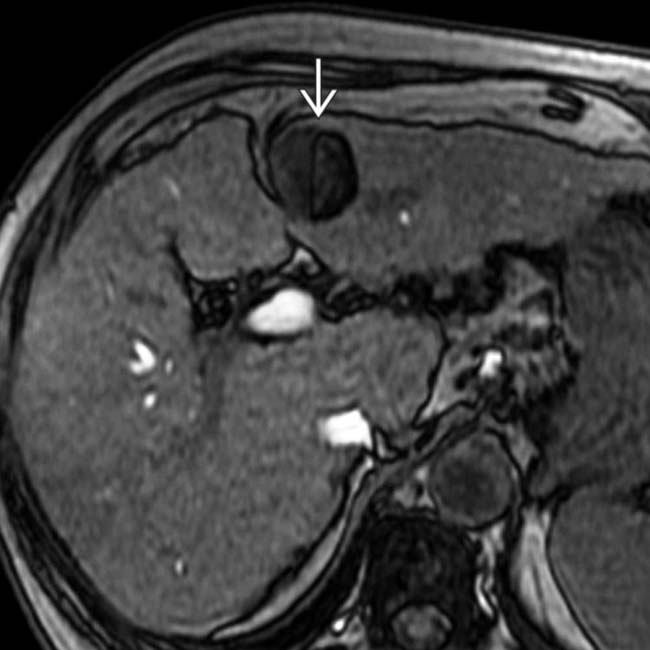
 . At resection, this was an HCC with fatty components within a larger dysplastic nodule. In addition, there are innumerable tiny cirrhotic regenerative nodules that are most evident as tiny hypointense foci on this GRE image.
. At resection, this was an HCC with fatty components within a larger dysplastic nodule. In addition, there are innumerable tiny cirrhotic regenerative nodules that are most evident as tiny hypointense foci on this GRE image.
 .
.
 is iso- to hypodense to the liver. These are typical features of HCC, particularly for a tumor detected as part of a surveillance program for patients with known cirrhosis who are at risk for developing HCC.
is iso- to hypodense to the liver. These are typical features of HCC, particularly for a tumor detected as part of a surveillance program for patients with known cirrhosis who are at risk for developing HCC.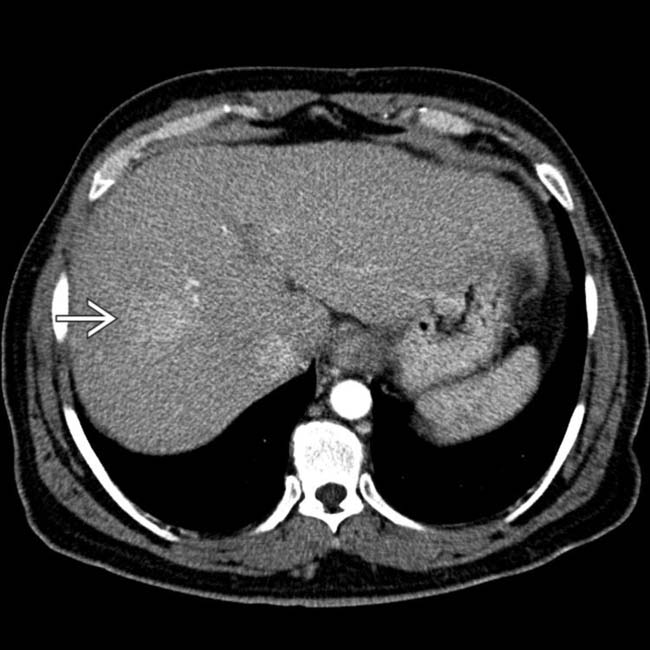
 . This proved to be HCC.
. This proved to be HCC.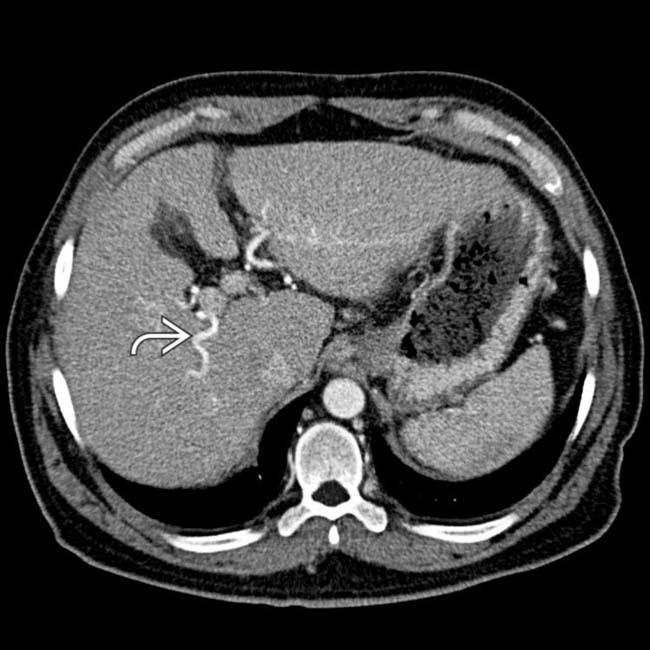
 .
.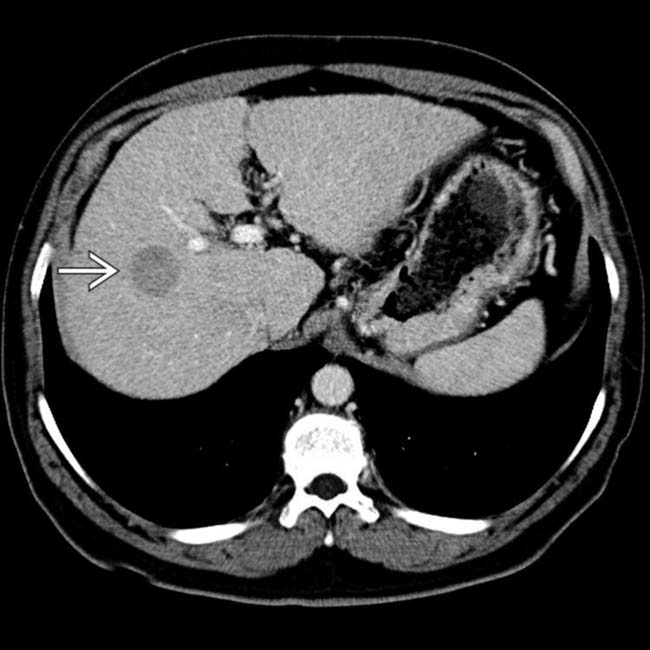
 , an HCC, much more clearly due to washout of contrast medium from the lesion.
, an HCC, much more clearly due to washout of contrast medium from the lesion.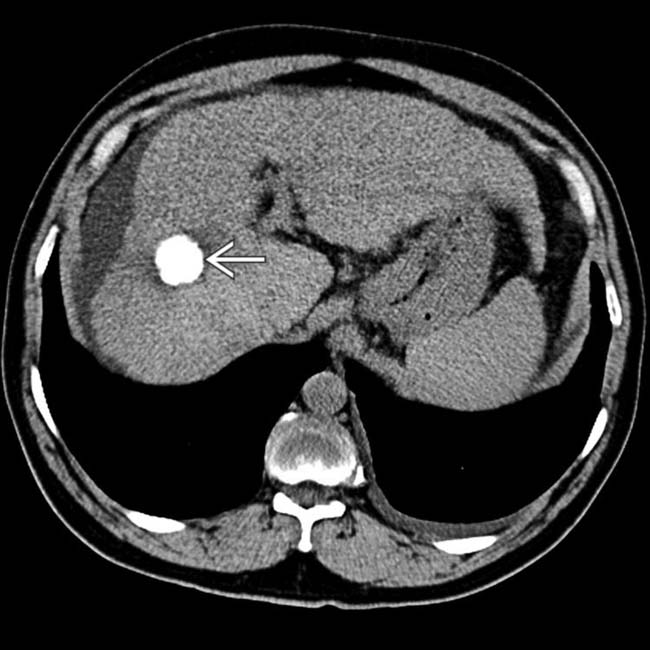
 . The tumor responded well to treatment, but liver function deteriorated, as evidenced by volume loss and development of ascites.
. The tumor responded well to treatment, but liver function deteriorated, as evidenced by volume loss and development of ascites.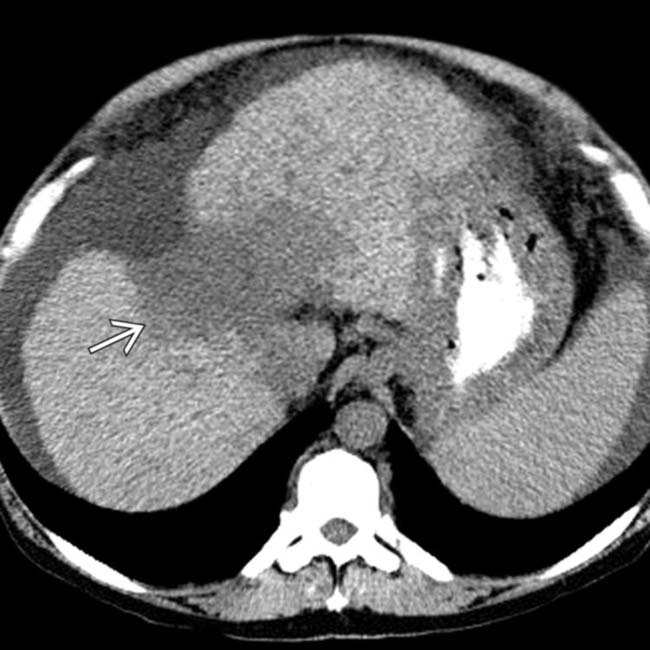
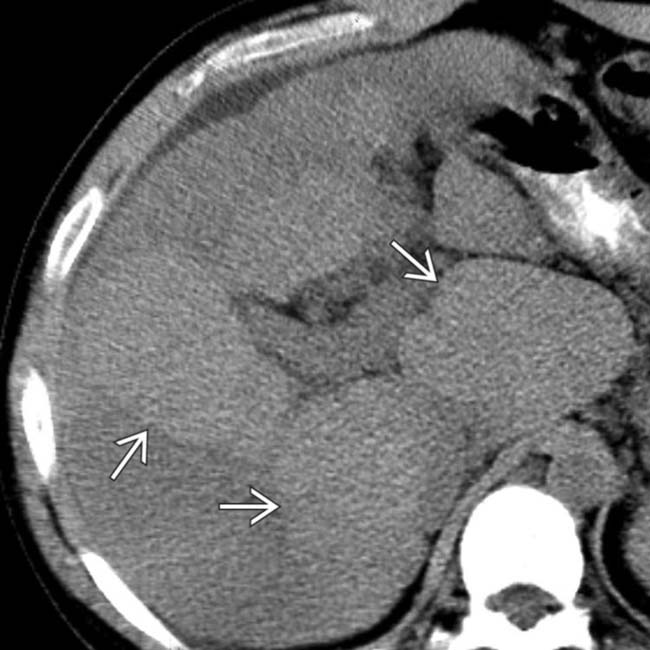
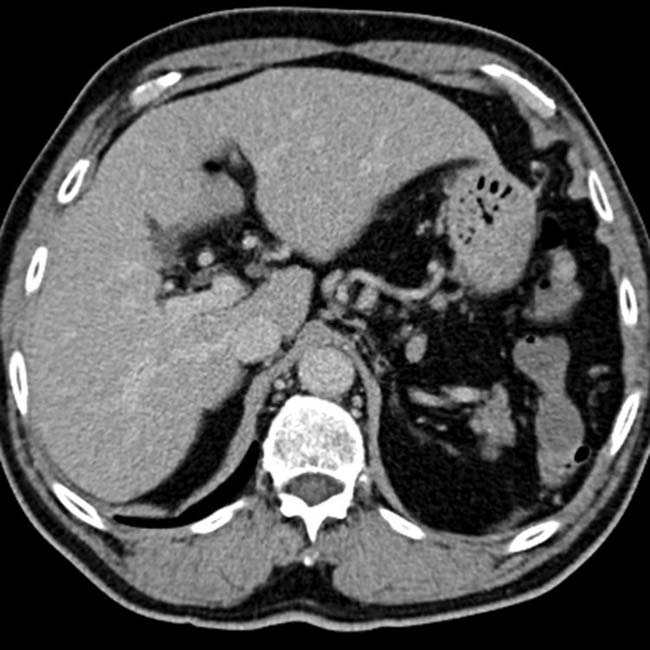
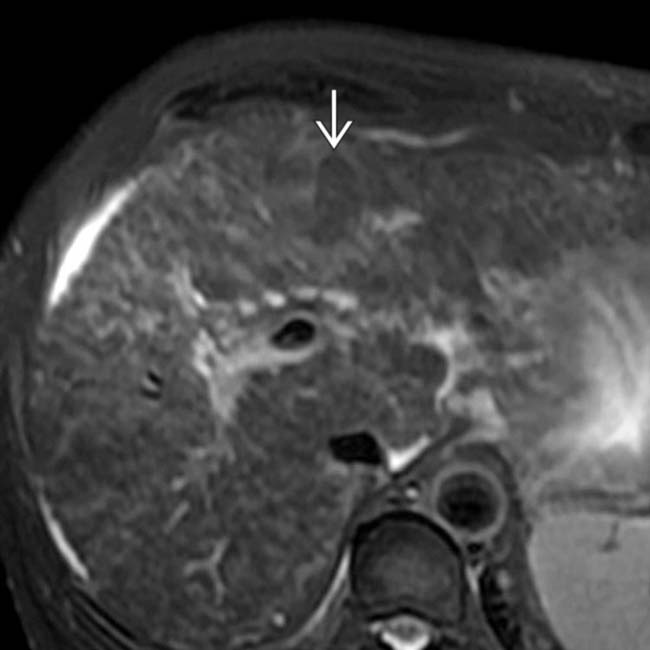
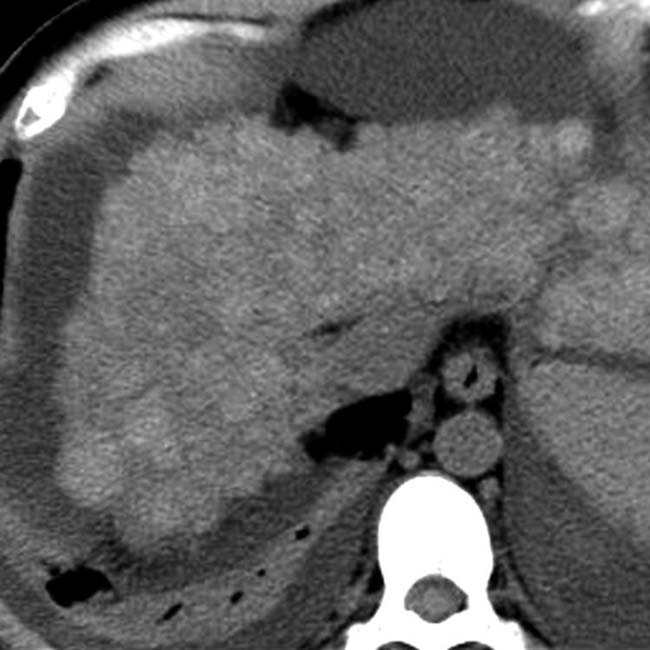
 within the anterior and medial segments; the overlying hepatic capsule is retracted. These findings are characteristic of confluent hepatic fibrosis, which is common in advanced cirrhosis.
within the anterior and medial segments; the overlying hepatic capsule is retracted. These findings are characteristic of confluent hepatic fibrosis, which is common in advanced cirrhosis.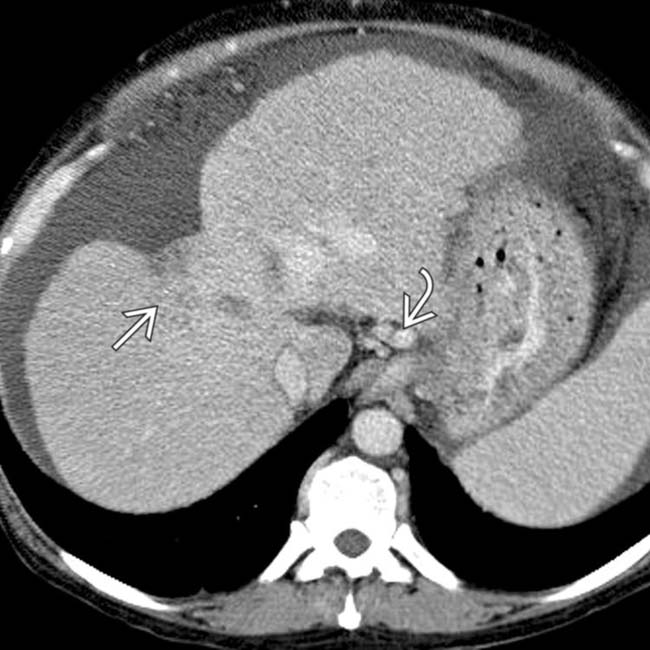
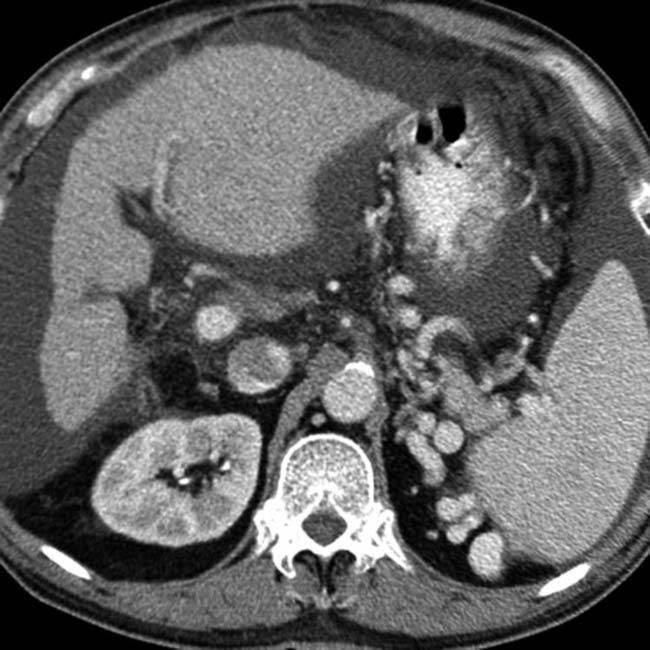
 in the same patient becomes almost isodense to the liver on this portal venous phase CECT. Also evident are varices
in the same patient becomes almost isodense to the liver on this portal venous phase CECT. Also evident are varices  , splenomegaly, and ascites, typical manifestations of portal hypertension.
, splenomegaly, and ascites, typical manifestations of portal hypertension.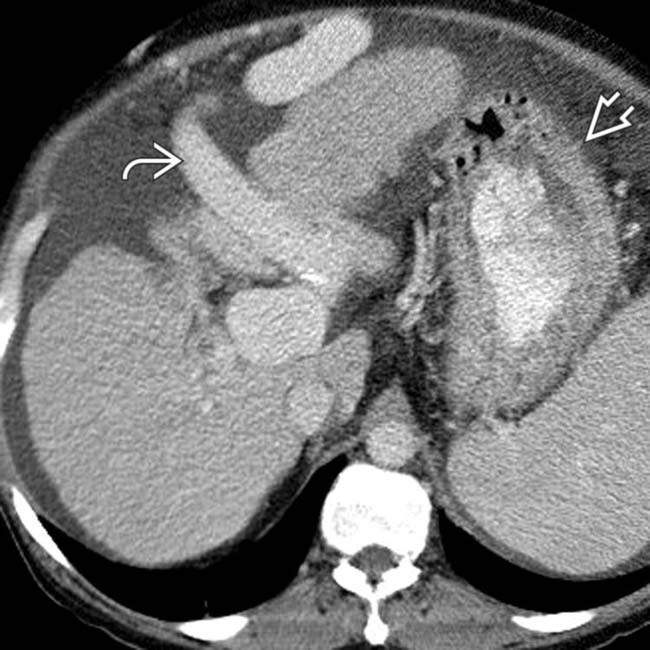
 and a thick-walled stomach
and a thick-walled stomach  that might represent portal hypertensive gastropathy.
that might represent portal hypertensive gastropathy.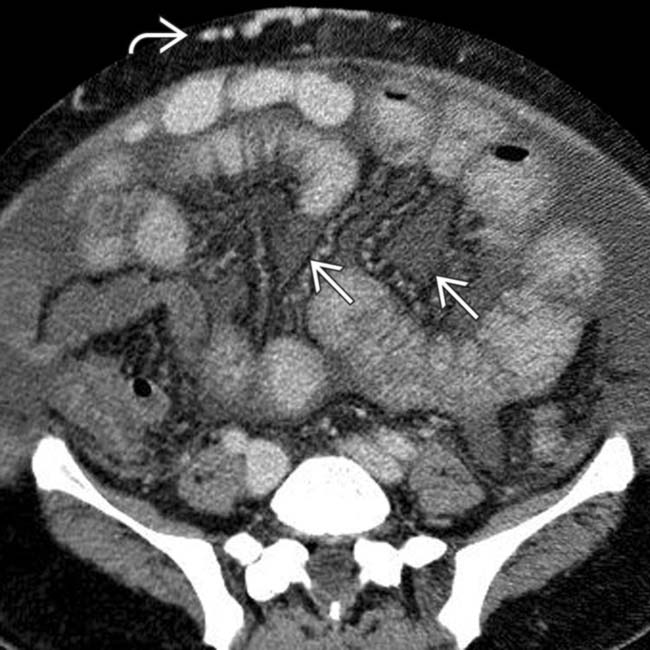
 , ascites, and mesenteric edema
, ascites, and mesenteric edema  that accentuates the mesenteric vessels and their enveloping fat.
that accentuates the mesenteric vessels and their enveloping fat.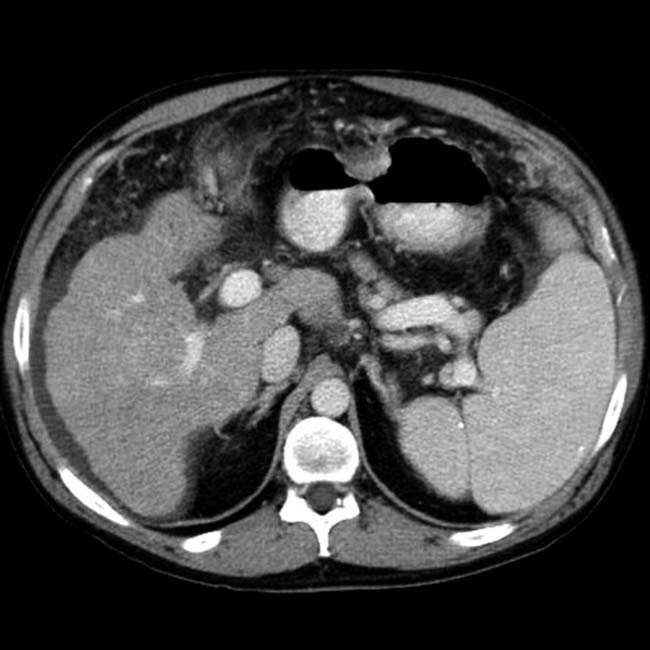
 , which simulates findings seen with colitis. On colonoscopy, there was no mucosal inflammation, only venous engorgement, known as portal hypertensive colopathy.
, which simulates findings seen with colitis. On colonoscopy, there was no mucosal inflammation, only venous engorgement, known as portal hypertensive colopathy.


































































































































 is hepatocellular carcinoma.
is hepatocellular carcinoma.