26 Chronic Arthritis
Clinical Presentation
Oligoarticular Juvenile Idiopathic Arthritis
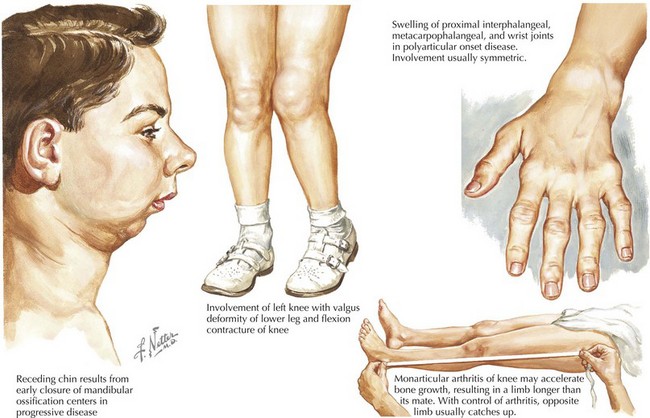
Oligoarticular JIA is defined by arthritis in four or fewer joints during the first 6 months of disease. Oligoarticular JIA is the most common form of JIA, typically occurs before age 4 years, and affects girls more often than boys at a ratio of 4 : 1. The knee is the most commonly affected joint followed by the ankles and small joints of the hand (Figure 26-1). The temporomandibular joint (TMJ) is also commonly affected. Children often experience morning stiffness, gelling (transient stiffness), and pain, but up to 25% may have painless arthritis. There are two subsets of oligoarthritis; persistent oligoarthritis affects a maximum of four joints throughout the disease course, and extended oligoarthritis affects more than four joints after the first 6 months of disease. Extended disease is associated with a worse prognosis.
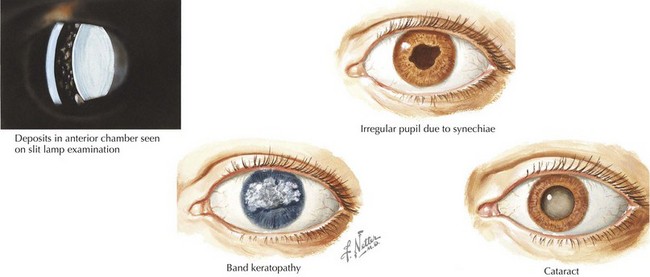
Although children with oligoarticular JIA have the greatest likelihood of remission among the JIA subtypes, complications can cause long-lasting morbidities. Asymmetric joint disease (particularly at the knee) can lead to leg length discrepancy caused by hyperemia of inflammation. Severe disease of the TMJ can lead to difficulty chewing, malocclusion, or micrognathia. Asymptomatic iridocyclitis (anterior uveitis that affects the iris and ciliary body) is common in oligoarthritis, particularly among young girls who are ANA positive, and must be screened for at disease presentation and serially thereafter. Complications of uveitis include visual impairment, posterior synechiae, cataracts, band keratopathy, and glaucoma (Figure 26-2).
Systemic Juvenile Idiopathic Arthritis
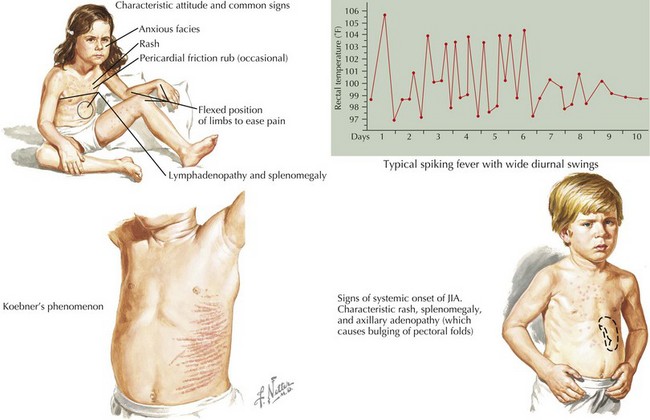
Systemic JIA is defined by arthritis; fever for at least 2 weeks with high quotidian spikes for at least 3 days; and at least one of the following: evanescent and erythematous rash, lymphadenopathy, hepatosplenomegaly, and serositis (often pericarditis or pleuritis). The disease affects boys and girls equally and can occur at any age but most commonly in early childhood. Children often appear ill during fevers and appear well when afebrile. Arthritis is generally symmetric and polyarticular but may be absent at onset. The rash consists of discrete, salmon-pink macules that are more pronounced during fever and may be associated with the Koebner phenomenon (linear streaks on the skin elicited by scratching) (Figure 26-3).
Psoriatic Arthritis
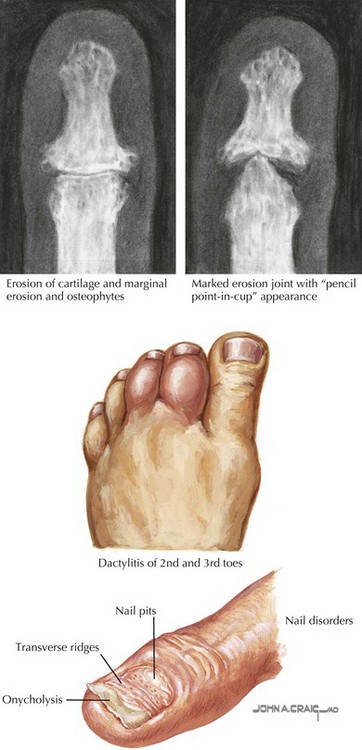
Psoriatic arthritis is defined by presence of arthritis and psoriasis, or if the rash is absent, arthritis and at least two of the following: dactylitis, nail pitting or onycholysis, and psoriasis in a first-degree relative (Figure 26-4). The disease affects girls slightly more often than boys and has a bimodal onset, with peaks in the preschool years and early adolescence. The arthritis is usually an asymmetric monoarthritis or polyarthritis affecting large and small joints and may develop several years before the rash. Patients may be ANA positive and are at risk for developing uveitis.
Enthesitis-Related Arthritis
On physical examination, enthesitis is identified by tenderness where the tendons insert into the bones. Some common enthesitis sites include the inferior pole of the patella, Achilles tendon insertion, plantar fascia insertion, and sacroiliac joints. Progression to JAS is most likely among children with episodic arthritis of the lower extremity large joints, enthesitis, and tarsitis within 1 year of ERA symptom onset. Extraarticular manifestations of ERA include symptomatic anterior uveitis (red, painful, photophobic eye), aortic insufficiency, aortitis, muscle weakness, and low-grade fever. ERA can also be the initial manifestation of IBD (see Chapter 110). Thus, it is important to screen for gastrointestinal symptoms, growth failure, erythema nodosum, and aphthous stomatitis.
Differential Diagnosis
The differential diagnosis of children with suspected JIA is broad given the heterogeneity of disease subsets. The most common classes of disorders that must be considered in the differential diagnosis of JIA include other rheumatologic diseases such as sarcoidosis, infection or postinfectious phenomena, malignancies, orthopedic conditions, and other inflammatory arthropathies (Box 26-1). The differential diagnosis of JIA is influenced by whether the presentation is acute, subacute, or chronic; whether the child has monoarticular or polyarticular arthritis; and the presence of systemic features.