Choroidal Rupture and Subretinal Hemorrhage
Clinical Features:
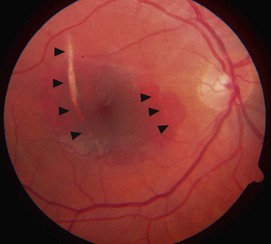
Choroidal ruptures typically occur concentrically to the optic nerve, most commonly temporally and involving the macula (Fig. 19.2.1 and Fig. 19.2.2). There is usually associated hemorrhage in the acute setting, which may be intraretinal or subretinal in location. Over time, the hemorrhage will clear, leaving an arc-shaped area of subretinal de-pigmentation with clumps of hyperpigmentation. Secondary CNV can occur months or years after trauma resulting in further visual loss.
OCT Features:
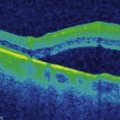
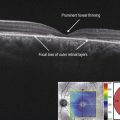
In the acute setting, associated hemorrhage often obscures the presence of a choroidal rupture from view with OCT. As the hemorrhage clears, it becomes more visible and more easily imaged. In the acute or subacute setting, a choroidal rupture appears as an elevated, nodule-like abnormality spanning Bruch’s membrane, the RPE, and inner choroid (Figs 19.2.3). With time, the nodular abnormality flattens, leaving a noticeably deformed area that exhibits negative shadowing from focal loss of the RPE (Fig. 19.2.4 and 19.2.5).
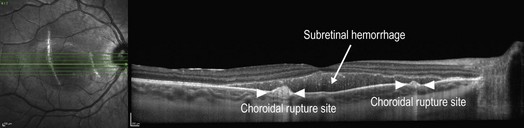
Figure 19.2.3 OCT through two separate choroidal rupture sites two weeks following injury. Overlying subretinal hemorrhage is also present. (Courtesy of Jeffrey S. Heier, MD.)
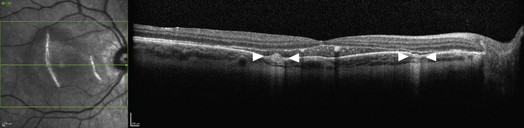
Figure 19.2.4 OCT through the same choroidal rupture sites, one month following injury, shows a decrease in size of the nodule-like elevations spanning Bruch’s membrane, the retinal pigment epithelium, and inner choroid. (Courtesy of Jeffrey S. Heier, MD.)
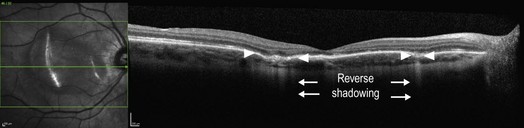
Figure 19.2.5 OCT through the same choroidal rupture sites, three months following injury, shows a continued flattening of the choroidal rupture sites. There is negative shadowing due to focal loss of retinal pigment epithelium that is highlighted (between arrowheads). (Courtesy of Jeffrey S. Heier, MD.)
Ancillary Testing:
Fluorescein angiography and/or indocyanine green angiography can be helpful in identifying the presence of a choroidal rupture site (Fig. 19.2.2) if the diagnosis is in question. FA can also be helpful to evaluate for the presence of an associated CNV membrane, which can develop later in up to 10% of eyes.