CHAPTER 2 Chondral Lesions
ANATOMY AND PATHOANATOMY
Historically, arthroscopic techniques of the hip have been limited by the unique anatomy of the hip joint. The complex three-dimensional bony structures of the proximal femur, pelvis, and acetabulum create a small window through which instruments must be passed and manipulated. This unique anatomy limits arthroscopic access to certain intra-articular zones1 with respect to osteochondral grafting and even microfracture in some cases. Adequate visualization of the central and peripheral compartments requires arthroscopy performed with and without traction using varying degrees of capsulotomies.
The articular surfaces of the acetabulum and femoral head are covered by hyaline cartilage. A film of synovial fluid between the articular surfaces is maintained by the labrum, which acts as a seal, allowing for the distribution of contact forces. Ferguson and colleagues2 have used a finite model and hypothesized that the labrum’s sealing effect during load application maintains a pressurized layer of fluid, which prevents solid on solid, contact thus reducing wear. Loss of labral function may lead to increased cartilage degeneration or cartilage defects. The structure of hyaline cartilage can be divided into layers—superficial (tangential), middle (transitional), deep (radial), and calcified layers. The calcified layer plays an important role in chondral injuries sustained during increases in shear forces as seen in femoroacetabular impingement. As the chondral surface of the acetabulum encounters increased shear forces during impingement, the force is transmitted to the calcified layer, which is relatively weak and ultimately the site of failure. This produces the characteristic cleavage delaminations at the labrochondral junction. This shear force can also lead to a wave sign or chondral blister, and eventual deep delamination (carpet delamination) of the articular cartilage from the subchondral bone.
The causes of cartilage injuries vary. Cartilage defects may be associated with avascular necrosis (AVN), femoroacetabular impingement (FAI), dysplasia, Legg-Calve-Perthes (LCP) disease, osteochondritis dissecans, or trauma. FAI is a common cause of chondral lesions. Injuries to articular cartilage may vary in presentation from damage to the cellular matrix to osteochondral defects. Damaged cartilage may be visible, as characterized by the Outerbridge3 classification, or appear normal on initial inspection. Probing the articular cartilage will occasionally reveal softening or deep delamination that is not evident on initial inspection.
Cartilage lesions may be found on the femur, acetabulum, or both. Femoral lesions appear to be less common than acetabular lesions in patients who meet the indications for hip arthroscopy. Focal femoral chondral injuries can be iatrogenic, the result of hip dislocation or subluxation, or seen in association with AVN and Perthes (see Fig. 2-13A). For some conditions, such as FAI, the femoral surface may remain well preserved until late in the disease course. Thus, articular involvement on the femoral side is often reflective of advanced bipolar degenerative changes. Acetabular lesions can be associated with hip subluxation and dislocation, FAI, or secondary degenerative lesions as a result of femoral cartilage defects.
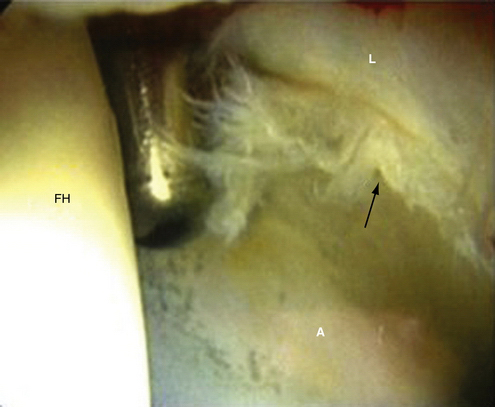
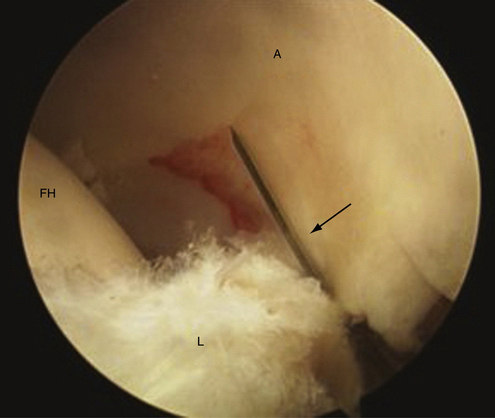
Chondral injuries may be found within specific locations on the femur or acetabulum according to cause. Most cartilage lesions treated in our practice arise in the setting of FAI. Chondral injuries seen in association with FAI have locations based on the type of impingement. Anterolateral cam impingement typically results in labrochondral disruption in the anterosuperior zones (zones 2, 3, and 4) with eventual cleavage delamination of the acetabular articular cartilage in this region (Fig. 2-1). Anterior-superior pincer impingement can lead to a more linear posterior acetabular chondral lesions (zones 4, 5) described as a contrecoupe lesion. Cam, Pincer, and mixed-type pathology can result in chondral blistering of the acetabular cartilage described as the wave sign (Fig. 2-2). This wave sign can indicate a predelamination injury or a deep carpet delamination of the articular cartilage or labrochondral complex without intra-articular extension. Chondral lesions can also be seen that involve detachment of the acetabular articular cartilage away from the labrochondral junction (toward the lunate fossa; see Fig. 2-17A). Each of these patterns has specific management options. In more advanced cases, full-thickness chondral lesions with exposed subchondral bone are seen (Fig. 2-3). Our observations are similar to those reported by McCarthy and Lee.4 They reviewed their findings of 457 hip arthroscopies and found the anterior and superior acetabulum to be the location of 73 % of the cartilage lesions. They also found that most anterior lesions were Outerbridge III or IV.
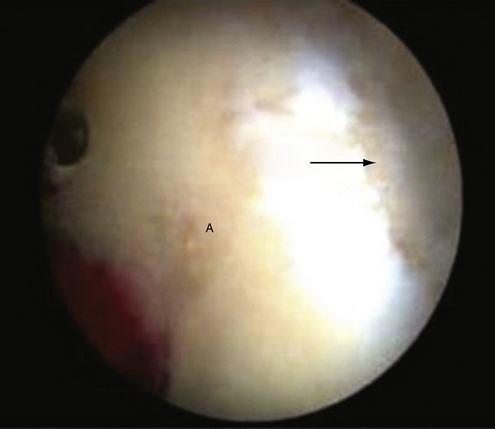
FIGURE 2-3 Full-thickness chondral defect in the anterosuperior acetabulum (arrow) in a left hip viewed through the anterior peritrochanteric portal. A, acetabulum.
Chondral injuries associated with dysplasia predominantly involve both the anterosuperior acetabulum and femoral head.5 Lesions involving the femoral head in the setting of dysplasia typically involve the superior weight-bearing portion of the head as opposed to involvement of the lateral, non–weight-bearing head-neck junction seen in FAI. In a series of hips that sustained lateral impact injuries, chondral lesions were located medially, with three patients demonstrating lesions on the medial weight-bearing region just superior to the cotyloid fossa and one patient with a lesion of the medial femoral head.6 Traumatic subluxation of the hip or dislocation may also result in osseous and chondral injuries. Philippon and associates7 reported on 14 professional athletes who were treated for traumatic dislocations of the hip, and each patient was reported to have an associated chondral lesion. Of these patients, 2 had isolated femoral head chondral defects, 6 had isolated acetabular chondral defects, and 6 had chondral defects on both surfaces. Moorman and coworkers8 have described an MRI triad for patients who sustained traumatic hip subluxations. The triad included a lesion located at the acetabular rim, based on the direction of injury, with a posterior osteochondral and labral avulsion from the acetabulum being most common. Traumatic subluxation or dislocation may also result in AVN or osteonecrosis of the femoral head. Nontraumatic causes of AVN are also common. Regardless of the cause, AVN most commonly results in osteochondral lesions of the anterosuperior femoral head. If subchondral collapse occurs, this typically leads to further degenerative changes throughout the hip.
HISTORY
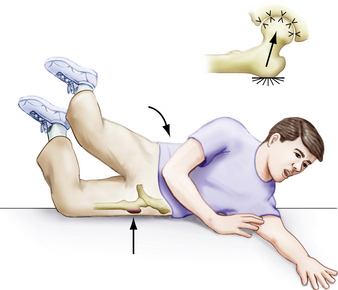
A thorough history and physical examination are essential when evaluating patients with suspected chondral lesions. A history of traumatic injury may be noted, such as hip subluxation, dislocation, or a fall directly onto the lateral hip (Fig. 2-4). More often, there is an insidious onset of hip pain, as seen in patients with FAI (Fig. 2-5). Patients with intra-articular pathology may complain of pain in the groin or anterior or deep lateral aspect of the hip. Occasionally, symptoms are referred to the posterior-buttock region or are a combination of anterior and posterior pain, as indicated by the C sign.9 Pain and discomfort are often exacerbated by activities such as running, cutting and pivoting in athletic endeavors, getting in and out of a car, arising from a seated position, and prolonged sitting. Patients occasionally note mechanical symptoms such as clicking, catching, or locking. In our experience clunking is more often associated with coxa saltans and not labral or chondral pathology. These complaints are indicative of intra-articular pathology and not specific to chondral injuries.
PHYSICAL EXAMINATION
Physical examination findings associated with chondral lesions tend to be vague and nonspecific. Gait evaluation is most often normal or mildly antalgic in patients with focal chondral lesions, with the exception of acute traumatic injuries. Inspection of the patient in the supine position is helpful. In the setting of acute trauma associated with a hip effusion or hemarthrosis, the patient may hold the leg in slight flexion, external rotation, and abduction. This position places the joint capsule at maximal volume and is a more comfortable position. Palpation of the involved hip should include the following areas: groin, trochanteric and peritrochanteric regions, anterior and inferior iliac spines, buttocks, lumbar spine, pubic rami and symphysis, insertion of the rectus abdominus, external oblique, and adductor origins. Extra-articular pain often accompanies intra-articular pathology and the primary or initial source of pain should be sought. Motion may be limited by guarding in the traumatic or chronic setting because of synovitis of the hip. The Stinchfield test and supine log roll test assess hip irritability and are suggestive of an intra-articular process.9 ROM, in particular internal rotation and flexion, may be limited in the setting of FAI. Alternatively, ROM may also be relatively increased in the setting of dysplasia or increased femoral anteversion. When performing provocative tests, it is imperative to verify whether the elicited pain is in fact the presenting complaint.
DIAGNOSTIC IMAGING
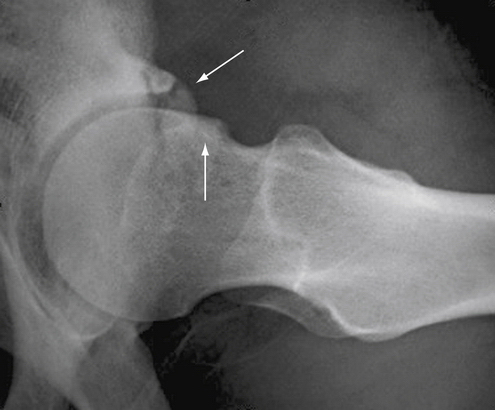
Initial imaging evaluation includes anteroposterior pelvis, false profile, and lateral hip radiographs. The anteroposterior radiograph should have the coccyx centered over the symphysis with 0 to 3 cm between these two structures. Plain radiographs can reveal rim fractures in the setting of hip dislocation or subluxation and structural abnormalities such as FAI, dysplasia, AVN, LCP, or loose bodies. Any significant joint space narrowing should be noted as this may significantly impact the success of hip arthroscopy. In the setting of hip subluxation or dislocation, Judet views allow for better assessment of the acetabulum, specifically the acetabular rim. Various radiographic measurements are routinely performed to understand the cause of the intra-articular pathology better. Our routine measurements and evaluation include the lateral center edge angle, anterior center edge angle, Tonnis angle, presence of femoral head lateralization, AP and lateral alpha angles, presence of a crossover sign, prominent ischial spines, coxa profunda or protrusio, os acetabuli or rim fractures, neck shaft angle, and Tonnis grading for degenerative changes.
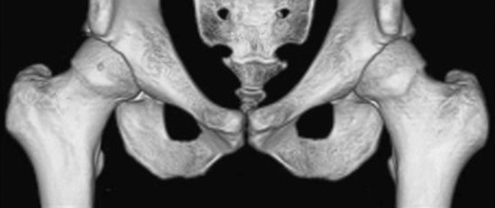
Computed tomography (CT) scans are helpful for further defining fractures, loose bodies, and structural abnormalities. In the setting of an acute subluxation, a CT scan is helpful to assess for posterior or, less commonly anterior, rim fractures. A concomitant radiographically guided aspiration can also aid in decompressing a traumatic hemarthrosis when present. We frequently obtain three-dimensional reconstructions for patients with FAI (Fig. 2-6). We find that it is helpful for defining the extent of impingement and planning the rim resection and proximal femoral osteochondroplasty commonly associated with most chondral lesions.
Magnetic resonance imaging (MRI) and MR arthrography (MRA) provide better assessment of soft tissues as well as more accurate staging of AVN. Nonarthrography MRI offers the advantage of being noninvasive but with less accuracy in identifying labral and chondral pathology. When assessing labral tears, Czerny and colleagues12 found that the sensitivity of MR arthrography was 90% and its accuracy was 91%, whereas the sensitivity of MRI was 30% and its accuracy was 36%, compared with open surgical findings. MRA, however is less sensitive for diagnosing chondral lesions in comparison to labral pathology. Keeney and associates13 published their results comparing MRA with hip arthroscopy. With respect to articular cartilage pathology, MRA had a sensitivity of 47%, specificity of 89%, positive predictive value of 84%, negative predictive value of 59%, and accuracy of 67%. The addition of a diagnostic anesthetic injection is helpful to verify the hip joint proper as the source of pain.33 New delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC) MRI techniques may lead to improved detection of subtle chondral lesions.15
INDICATIONS AND CONTRAINDICATIONS
Contraindications to arthroscopic treatment of chondral injuries must be kept in perspective to optimize outcomes. Patients with moderate or severe osteoarthritis and a predominance of aching pain provide little opportunity for significant improvement, even in the short term. A recent study by Larson and coworkers15 found a high rate of failure in hips with more than 50% joint space narrowing, bipolar grade 3 and 4 lesions seen on MRI scans, and a predominance of aching pain at rest. Chondral lesions greater than 2 cm in diameter also resulted in high rates of failure. Patients with significant dysplasia (center edge angle less than 20 degrees) cannot have normal joint reaction forces re-established with an arthroscopic procedure. It is critical to differentiate FAI from dysplasia because cam lesions have been reported in the presence of acetabular dysplasia.34 The inability to restore relatively normal biomechanics can lead to failure of any cartilage restoration procedure and is therefore considered a relative contraindication to arthroscopic surgery. In addition, aggressive capsulotomies and labral débridements could lead to increased instability and failure rates in these individuals. Patients with dysplasia and superior and/or lateral subluxation on preoperative radiographs should not be considered candidates for hip arthroscopy. Finally, patients with significant acetabular retroversion and a severely deficient posterior rim may be better served with an open procedure, such as a reverse periacetabular osteotomy, at which time any chondral defects may be addressed.
TREATMENT
Conservative Management
Patients with degenerative arthritis are poor candidates for arthroscopy. We currently recommend therapy and symptomatic treatment, including injections and nonsteroidal anti-inflammatory drugs (NSAIDs). We will allow patients to have repeated corticosteroid injections in this setting. Kullenberg and colleagues16 have found that pain and range of motion significantly improve at 3 and 12 weeks following an intra-articular corticosteroid injection in the setting of osteoarthritis. There is evidence in the literature to support viscosupplementation in the setting of degenerative changes in the hip,17 but the level of evidence is low and viscosupplementation did not provide the same level of relief when compared with corticosteroids.18
Surgical Management
Arthroscopic Technique
Anesthesia and Positioning.
A general anesthetic or spinal anesthesia can be used for hip arthroscopy. Although muscle relaxation is required for adequate distraction, paralysis is not necessary in most cases. Although hip arthroscopy can be performed in the supine or lateral position, we prefer the supine position. The patient is placed supine on a standard fracture table or standard table with the various distraction attachments available (Fig. 2-7). The involved hip is positioned in 5 to 10 degrees of flexion, neutral or slight abduction, and internal rotation. The contralateral hip is maximally abducted with external rotation. A thorough fluoroscopic evaluation of the hip is then performed. The bed is rotated, aligning the anterior superior iliac spines parallel to the floor, allowing for accurate assessment of acetabular version and rim resection if indicated. The femoral head neck junction is evaluated with the following “around the world” fluoroscopy technique. The hip is flexed to about 45 degrees with maximal internal, neutral, and external rotation. It is then extended with maximal internal, neutral, and external rotation. Finally, a cross-table lateral view with maximal internal rotation completes the evaluation of the femoral head neck junction. Distraction is then applied to verify that adequate distraction has been achieved; the distraction is then released prior to prepping and draping.
Procedure.
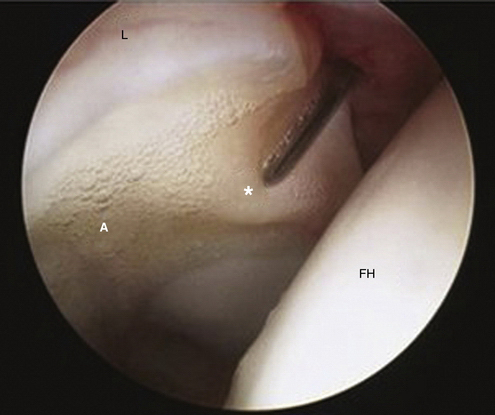
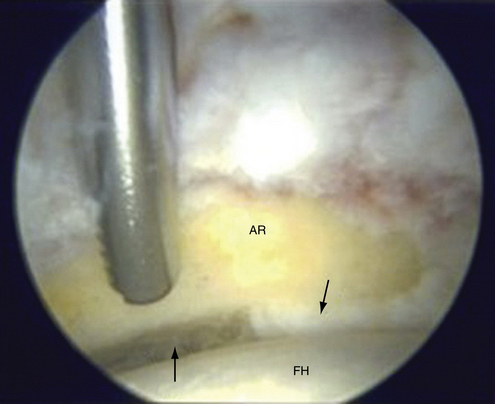
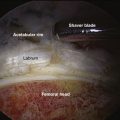
A routine diagnostic evaluation of the central compartment is performed. A thorough evaluation is essential for defining and confirming any pathologic process, anticipated or unanticipated.35 The anterior, superior, and posterior acetabulum, acetabular labrum, femoral head, and ligamentum teres and associated lunate fossa are carefully inspected. Chondral lesions may be obvious, as with exposed subchondral bone for full-thickness lesions or obvious displaced chondral flaps (Fig. 2-8). It is not uncommon to encounter less obvious labrochondral disruptions and it is imperative to probe the labrochondral junction thoroughly. Chondral softening or deep delamination may be noted by probing the articular cartilage; these are typically located at the anterosuperior acetabulum (Fig. 2-9). These can indicate pre-delamination injuries or deep “carpet delamination” without intraarticular extension. The size and location of the chondral injuries are recorded using the geographic zone method, as described by Ilizaliturri and associates1 (Fig. 2-10).
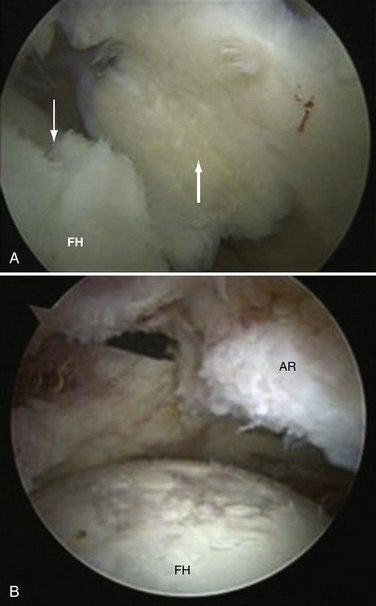
FIGURE 2-8 Cartilage defects. A, Loose cartilage flap (thick white arrow) from the right femoral head (black arrow) viewed through the anterior peritrochanteric portal. B, Full-thickness cartilage loss of a right femoral head as viewed through the anterior peritrochanteric portal with an ablation probe in the anterior portal. AR, acetabular rim; FH, femoral head.
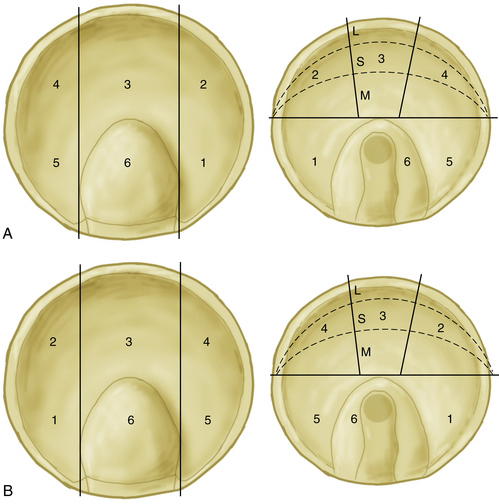
FIGURE 2-10 Regional zone method for recording the location of intra-articular lesions. The acetabular zones are to the left. Two vertical lines are drawn using the anterior and posterior notch walls as a reference. A horizontal line is drawn at the top of the acetabular notch. These lines divide the acetabulum into six different zones. Progressive numbers are assigned to each one of the zones, starting with 1 at the anterior-inferior zone; 6 is assigned to the acetabular notch. The femoral head is to the right. Lines are positioned following the pattern of the lines used for the acetabulum. The head is presented dislocated in an open book fashion; therefore, the head is a mirror image of the acetabulum. Zone 6 contains the ligamentum teres. In the femoral head, zones 2, 4, and 5 are subdivided into three areas: medial (M), superior (S), and lateral (L). Dashed line, area that corresponds to the acetabular notch. A, Left hip zones. B, Right hip zones.
The specific management technique used depends on the pattern of chondral injury and associated pathology, such as FAI. Full-thickness chondral lesions are typically addressed using the microfracture technique. Initially, any loose chondral fragments and flaps are débrided with a combination of an angled punch, ring curette, and/or shaver, taking care to leave a stable chondral edge (Fig. 2-11). It is important to verify that the surrounding chondral surface and opposing chondral surface (femur or acetabulum) have relatively healthy cartilage to ensure a contained lesion. Chondral repair techniques may not be appropriate in lesions that are not contained. Failure of containment occurs when the articular cartilage of the femoral head contacts the subchondral bone of an acetabular defect after débridement and release of traction. Similarly, failure in containment of a femoral head defect occurs when the subchondral bone of the femoral lesion contacts the articular cartilage of the acetabulum. Containment can be verified after the release of traction under direct visualization through the arthroscope or indirectly by the use of intraoperative fluoroscopy. Chondral lesions on the acetabulum are typically located at the rim and containment is readily verified with direct visualization (Fig. 2-12). Alternatively, indirect verification by observation of a well-maintained joint space on anteroposterior, frog-leg, and cross-table lateral intraoperative fluoroscopy views may indicate appropriate containment.
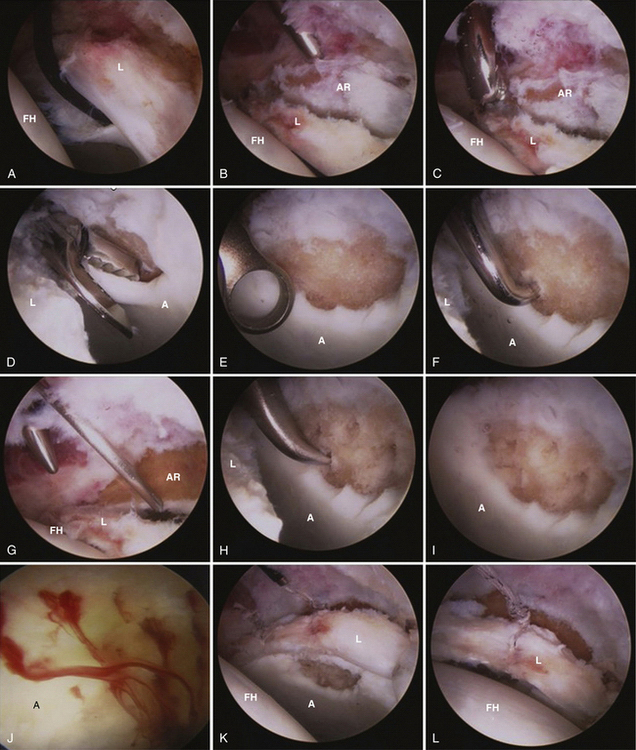
FIGURE 2-11 Left hip in a patient with combined pincer-type and cam FAI. A, Typical labrochondral disruption with delamination of the articular cartilage extending medially as viewed through the anterior peritrochanteric portal. B, After labral takedown. C, Burr in the anterior portal performing a rim resection. D, Punch used to débride the unstable chondral flap. E, Ring curette used to débride the articular cartilage back to a stable rim. F, 90-degree microfracture awl placed through the anterior portal. G, Establishing a more distal and lateral accessory anterior portal with a spinal needle. H, 45-degree awl placed through the accessory anterior portal, I, Lesion after débridement and microfracture. J, Bleeding from the microfracture holes. K, After labral refixation. L, Traction is released, demonstrating a contained lesion with intact labrum. A, acetabulum; AR, acetabular rim; FH, femoral head; L, labrum.
After removal of unstable chondral flaps, a ring curette is used to remove the calcified cartilage layer. Microfracture awls are then used to penetrate the subchondral plate, with visualization of fat droplets and or marrow elements. Microfracture begins at the periphery and ends at the center of the lesion, placing perforations 3 to 4 mm apart. Performing microfracture often requires the use of an awl through various portals. This technique provides access to the most lesions on both the acetabular and femoral head, with the exception of lesions located on the most central portion of the femoral head (medial aspect of zones 2M, 3M, 4M, and 6). Fortunately, these lie outside the major weight-bearing zones, and tend to be associated with more significant degenerative changes that would not be as appropriate for microfracture. When the microfracture is complete, the flow is stopped and subchondral bleeding is assessed to ensure an adequate depth of penetration. For hips with AVN, chondral flaps are removed to a stable edge (Fig. 2-13). Although the underlying bone is generally avascular, microfracture or deeper penetration with a drill or Kirschner wire can be performed if an appropriate angle can be achieved in an attempt to reach the deeper vascular bone.
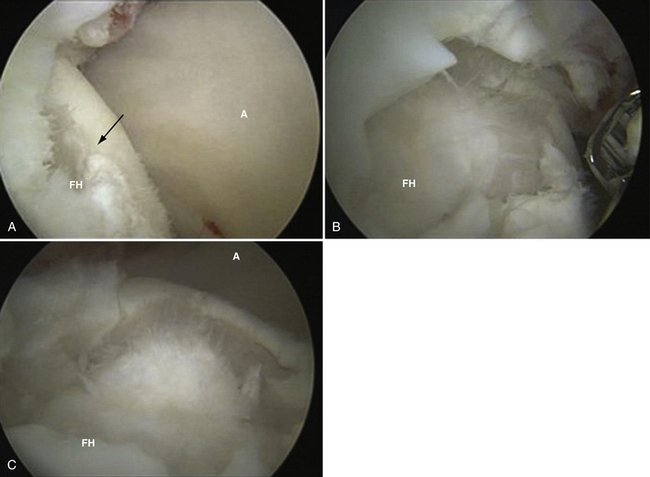
FIGURE 2-13 Right femoral head with AVN, subchondral collapse, and full-thickness cartilage lesions viewed through the anterior peritrochanteric portal and instrumentation in the anterior portal. A, Full- thickness defect (arrow) on the anterosuperior femoral head. B, Further débridement with a basket punch. C, After removal of unstable chondral flaps. A, acetabulum; FH, femoral head.
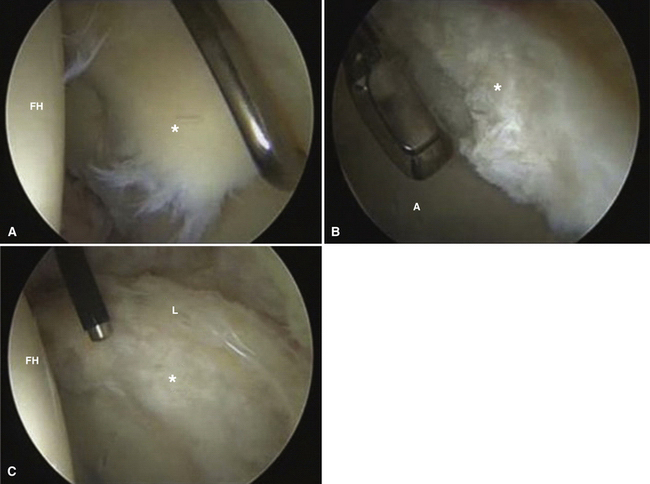
There are other lesions with characteristic patterns of associated impingement that deserve special note. It is imperative to address any underlying femoroacetabular impingement to eliminate the cause of associated chondral lesions. This includes correction of pincer-type impingement with acetabular rim resection and cam-type impingement with femoral resection osteochondroplasty, as dictated by the nature of the impingement. Chondral treatment will likely fail if hip impingement is not corrected. For patients with pincer impingement, rim resection may eliminate or significantly decrease the size of the chondral lesion requiring treatment. Deep chondral delamination involving the labrochondral junction without intra-articular extension (carpet delamination) is another characteristic finding that can be associated with FAI (Fig. 2-14). In this situation, the labrum either requires labral resection or débridement or a careful detachment of the labrum from the articular cartilage to access the deep delamination.
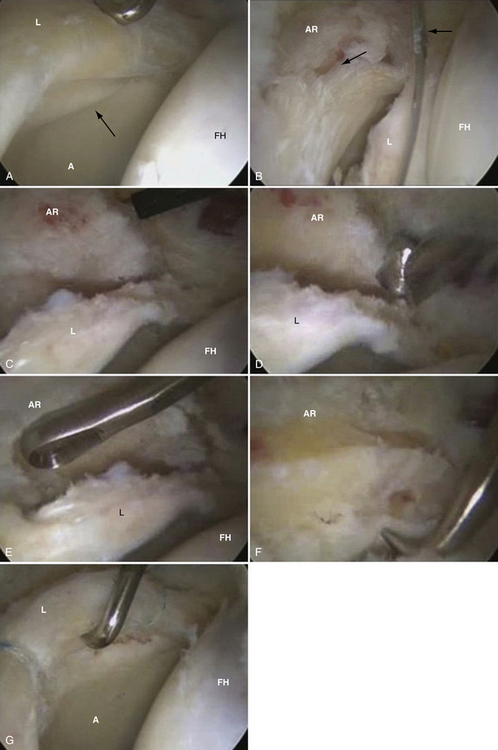
FIGURE 2-14 Deep chondral delamination without labrochondral disruption in a patient with combined cam–pincer-type FAI of the right hip. All views are through the anterior peritrochanteric portal, with instrumentation via the anterior portal. A, Wave sign, or carpet delamination (arrow). B, Delamination of the articular cartilage (thick arrow) from the acetabular rim (AR) is evident after the labrum (L) has been taken down with an arthroscopic knife (thick arrow) and displaced toward the femoral head (FH). C, Anterosuperior overcoverage of the acetabular rim. D, Rim trim with high-speed burr. E, Removal of the delaminated and unstable cartilage with a ring curette. F, Microfracture with a 90-degree awl. G, Significant decrease in the size of the lesion after rim resection and labral refixation.
We prefer to detach the labrum from the rim with a beaver blade. This is begun with the beaver blade introduced through the anterior portal and detaching the labrum to the superior extent of the lesion. The arthroscope can then be switched to the anterior portal and the labrum can be further detached superiorly and posteriorly, if necessary, with visualization obtained by inserting the arthroscope between the detached labrum and acetabulum. The beaver blade is then introduced through the anteroparatrochanteric portal between the previously detached portion of the labrum and acetabular rim (Fig. 2-15). The chondral wave, or deep delamination, is then removed with a biter and shaver, and appropriate rim resection is performed. Microfracture is then performed as described earlier and the labrum is refixed with suture anchors placed 1 cm apart (typically, three or four anchors). Labral refixation can be performed with one limb of the suture passed under and around or through the labrum. Passing the suture through the labrum creates a mattress stitch, which may better preserve the labrum-sealing function (Fig. 2-16). Microfracture can be completed after labral refixation if the labrum obstructs the view of the chondral lesion prior to refixation. Another pattern of injury involves chondral detachment–delamination away from the labrochondral junction (closer to the lunate fossa; Fig. 2-17). In this case, the articular cartilage is excised with a shaver and biter to the edge of the labrum. If pincer impingement is not present, the labrum can be débrided on the articular side if the periphery is stable or the labrum can be repaired with a similar technique as described earlier if the labrum is torn to or through the periphery. For any of these lesions, if delaminations or disruptions are partial thickness, the remaining stable cartilage is left in place and microfracture is not typically performed.
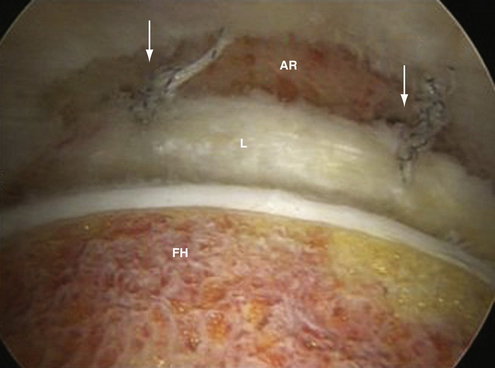
FIGURE 2-16 Passing the suture through the labrum (arrows) creates a mattress stitch, which allows the labrum to sit on the edge of the acetabular rim and may restore the sealing function of the labrum better. AR, acetabular rim; FH, femoral head; L, labrum.
The final portion of the procedure involves an evaluation of the peripheral compartment and femoral resection osteoplasty is performed, when indicated. It should be noted that in patients with mild dysplasia, rim trimming should be avoided or minimal, and every attempt should be made to preserve the acetabular labrum. Additionally, closure of any extended capsulotomies should be considered to avoid destabilization of the hip joint. Capsular closure is performed with multiple heavy, braided absorbable sutures passed with a curved suture lasso device, tying the knot blindly on the periphery of the capsule (Fig. 2-18). The hip should be in extension and neutral rotation when tying the sutures to avoid overtightening of the capsular ligaments. Although we routinely perform closure of capsulotomies in mild or borderline dysplasia, it is unclear whether routine capsular closure in all cases has any affect on outcomes.
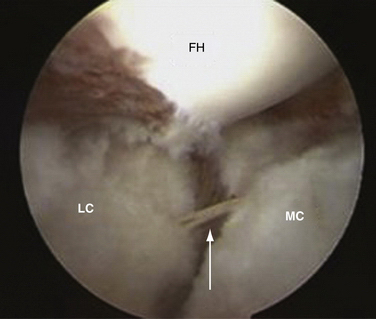
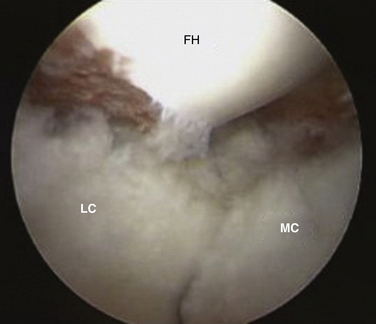
FIGURE 2-18 Capsular closure after capsulotomy for arthroscopic treatment of FAI in the right hip viewed through the anterior portal with the femoral head (FH) oriented at the top of the images. A, Suture (arrow) is passed through the medial (MC) and lateral (LC) portions of the remaining capsule. B, It is then tied using an arthroscopic technique. This is typically done without visualization of the knot.
COMPLICATIONS
PEARLS& PITFALLS
PEARLS
PITFALLS
OUTCOMES
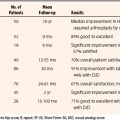
Current treatment of chondral lesions ranges from simple débridement to partial resurfacing with nonbiologic materials. Simple debridement provides modest relief.19 Microfracture remains the mainstay for treatment of grade IV chondral defects, regardless of location.20 Several authors have reported results of microfracture in the hip in small subsets of larger case series or as case reports.21–24 Byrd and Jones25 have reported on 21 patients with a mean follow-up of 2 years who underwent microfracture for grade IV chondral defects. Indications included a well-circumscribed grade IV articular lesion with intact subchondral bone and healthy surrounding cartilage, and the ability of the patient to participate in the 3-month structured postoperative rehabilitation protocol. The average size of the lesion was 122 mm2. The mean improvement was 23.9 points (preoperative, 51.4; postoperative, 75.2). Quantitative improvement was maintained in 86% of patients. Philippon and associates26 have reported their findings in 9 patients during revision hip arthroscopy who had undergone microfracture of acetabular lesions at the time of their index procedure. The time from index arthroscopy to revision arthroscopy ranged from 10 to 36 months. The original lesion size averaged 163 mm2. Eight of 9 patients had 95% to 100% coverage of an isolated acetabular chondral lesion or acetabular lesion associated with a femoral head lesion, with a grade 1 or 2 appearance of the repair product at an average of 20 months follow-up. One patient with diffuse osteoarthritis failed, with only 25% coverage 10 months after index arthroscopy. Despite the small numbers in the current literature, the initial outcomes demonstrate promising results.
Pridie drilling has been discussed in association with open surgical approaches27 but with no reported outcomes or arthroscopic applications. The concept is similar to that of microfracture, with introduction of pluripotent stem cells from the bone marrow that differentiate and produce fibrocartilage that fills the defect. Arthroscopic autologous chondrocyte transplantation (ACT) has not been reported in the hip with first-generation techniques and would be technically challenging. This is probably best done via an open approach. However, second- and third- generation techniques using bioabsorbable scaffolds that do not require suture stabilization may prove beneficial and applicable for arthroscopic surgery. Fontana28 has reported non–peer-reviewed results of arthroscopic ACT versus débridement. The BioSeed-C scaffold was used for delivery of the cultured chondrocytes in a staged method. The average postoperative Harris hip score (HHS) improved in both groups. However, a greater increase was seen in the ACT group when compared with débridement alone, with scores of 86 and 65, respectively. Osteochondral autograft transplantation (OATS) and osteochondral allograft can technically be done arthroscopically for femoral chondral lesions. Medial lesions do not allow for appropriate angles of implantation but other lesions, in which an appropriate angle is achieved, can be treated with 8- to 10-mm grafts taken from the anterolateral femoral head-neck junction, with the hip out of traction. The grafts can then be implanted with or without traction, depending on the location of the lesion. This has been performed, but no peer-reviewed case reports or series have been published to date. Rittmeister and coworkers29 have reported the results of mosaicplasty performed in five patients with osteonecrosis of the femoral head. The procedure was performed through an open approach. Four of the five had unsatisfactory results, with eventual THA at a mean of 49 months. Hart and colleagues30 have reported their 6-month follow-up of a single patient treated with mosaicplasty. This was also done through an open approach and the patient demonstrated complete resolution of pain, full ROM, and an HHS of 100. Osteochondral allografts have also been used in the setting of AVN. Short-term results have been satisfactory,31 but longer term results are not available in the literature. HemiCAP partial resurfacing (Arthrosurface, Franklin, Mass), has also been applied to the hip.32
Most of these procedures have been described through an open approach and have yet to be reported in the literature as part of an arthroscopic approach. Microfracture remains the mainstay for the primary treatment of focal chondral lesions.
1. Ilizaliturri VMJr, Byrd JWT, Sampson TG, et al. A geographic zone method to describe intra-articular pathology in hip arthroscopy: cadaveric study and preliminary report. Arthroscopy. 2008;24:534-539.
2. Ferguson SJ, Bryant JT, Ganz R, Ito K. The acetabular labrum seal: a poroelastic finite element model. Clin Biomech (Bristol, Avon). 2000;15:463-468.
3. Outerbridge R. The cause of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752-754.
4. McCarthy JC, Lee JA. Arthroscopic intervention in early hip disease. Clin Orthop Relat Res. 2004;429:157-162.
5. Noguchi Y, Miura H, Takasugi S, Iwamoto Y. Cartilage and labrum degeneration in the dysplastic hip generally originates in the anterosuperiorweight-bearing area: an arthroscopic observation. Arthroscopy. 1999;15:496-506.
6. Byrd JWT. Lateral impact injury: a source of occult hip pathology. Clin Sports Med. 2001;20:801-815.
7. Philippon MJ, Kuppersmith DA, Wolff AB, Briggs KK. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:169-174.
8. Moorman CTIII, Warren RF, Hershman EB, et al. Traumatic posterior hip subluxation in American football. J Bone Joint Surg Am. 2003;85:1190-1196.
9. Byrd JWT. Operative Hip Arthroscopy, 43. 2nd ed. New York: Springer; 2005.
10. Reider B, Martel J. Pelvis, hip and thigh. In: Reider B, Martel J, editors. The Orthopedic Physical Examination. Philadelphia: WB Saunders; 1999:159-199.
11. Philippon MJ, Stubbs AJ, Schenker ML, et al. Arthroscopic management of femoroacetabular impingement; osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571-1580.
12. Czerny C, Hofmann S, Neuhold A, et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology. 1996;200:225-230.
13. Keeney JA, Peell MW, Jackson J, et al. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004;429:163-169.
14. Clohisy JC, Beaulé PE, O’Malley A, et al. AOA Symposium. Hip disease in the young adult: current concepts of cause and surgical treatment. J Bone Joint Surg Am. 2008;90:2267-2281.
15. Larson CM, Giveans MR, Taylor M. Effect of osteoarthritis on outcomes after management of femoroacetabular impingement, Paper presented at: American Orthopaedic Society for Sports Medicine Specialty Day Las, Vegas: American Orthopaedic Society for Sports Medicine; February 2009.
16. Kullenburg B, Runesson R, Tuvhag R, et al. Intra-articular corticosteroid injection: pain relief in osteoarthritis of the hip. J Rheumatol. 2004;31:2265-2268.
17. van den Bekerom MPJ, Lamme B, Sermon A, Mulier M. What is the evidence for viscosupplementation in the treatment of patients with hip osteoarthritis? Systematic review of the literature. Arch Orthop Trauma Surg. 2008;128:815-823.
18. Qvistgaard E, Christensen R, Torp-Pedersen S, Bliddal H. Intra-articular treatment of hip osteoarthritis: a randomized trial of hyaluronic acid, corticosteroid, and isotonic saline. Osteoarthritis Cartilage. 2006;14:163-170.
19. Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578-587.
20. Steadman JR, Briggs KK, Rodrigo JJ, et al. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 2003;9:477-484.
21. Kelly BT, Williams RJ3rd, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020-1037.
22. Hardy P, Hinojosa JF, Coudane H, et al. Osteochondritis dissecans of the acetabulum. Apropos of a case. Rev Chir Orthop Reparatrice Appar Mot. 1992;78:134-137.
23. Roy DR. Arthroscopic findings of the hip in new onset hip pain in adolescents with previous Legg-Calve-Perthes disease. J Pediatr Orthop B. 2005;14:151-155.
24. McCarthy J, Barsoum W, Puri L, et al. The role of hip arthroscopy in the elite athlete. Clin Orthop Relat Res. 2003;406:71-74.
25. Byrd JWT, Jones KS. Microfracture for grade IV chondral lesions of the hip (SS-89). Arthroscopy. 2004;20(suppl 1):e41.
26. Philippon MJ, Schenker ML, Briggs KK, Maxwell RB. Can microfracture produce repair tissue in acetabular chondral defects? Arthroscopy. 2008;24:46-50.
27. Beck M, Leunig M, Parvizi J, et al. Anterior femoroacetabular impingement. Part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67-73.
28. Fontana A. Arthroscopic approach in hip defects. In: Zanasi S, Brittberg M, Marcacci M, editors. Basic Science, Clinical Repair and Reconstruction of Articular Cartilage Defects: Current Status and Prospects. Bologna, Italy: Timeo Editore; 2006:419-422.
29. Rittmeister M, Hochmuth K, Kriener S, Richolt J. Five-year results following autogenous osteochondral transplantation to the femoral head. Orthopade. 2005;34:320-326.
30. Hart R, Janecek M, Visna P, et al. Mosaicplasty for the treatment of femoral head defect after incorrect resorbable screw insertion. Arthroscopy. 2003;19:e1-e5.
31. Meyers MH, Jones RE, Bucholz RW, Wenger DR. Fresh autogenous grafts and osteochondral allografts for the treatment of segmental collapse in osteonecrosis of the hip? Clin Orthop Relat Res. 1983;174:107-112.
32. Jager M, Begg MJW, Krauspe R. Partial hemi-resurfacing of the hip joint—a new approach to treat local osteochondral defects. Biomed Tech. 2006;51:371-376.
33. Byrd JWT, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668-1674.
34. Ganz R, Leunig M. Morphological variations of residual hip dysplasia in the adult. Hip Int. 2007;17:S22-S28.
35. Bond JL, Knutson ZA, Ebert A, Guanche CA. The 23-point arthroscopic examination of the hip: basic setup, portal placement, and surgical technique. Arthroscopy. 2009;25:416-429.