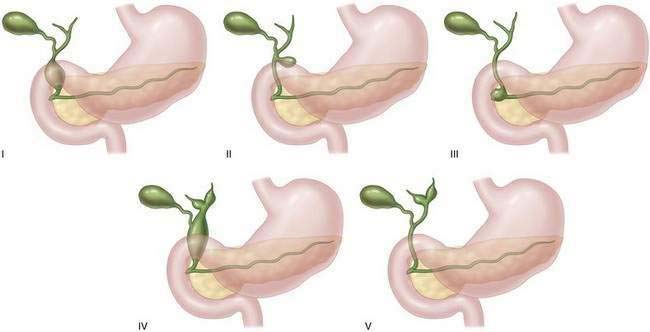
CHAPTER 24 Choledochal Cysts
Step 1: Surgical Anatomy
 Types II, III, and V choledochal cysts are rare variants.
Types II, III, and V choledochal cysts are rare variants.
Step 2: Preoperative Considerations
Presentation
Diagnosis
Treatment Strategy
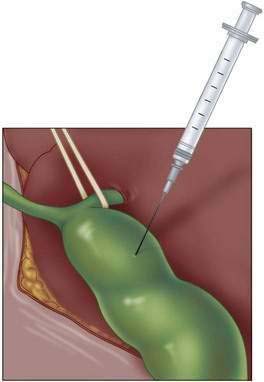
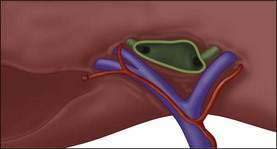
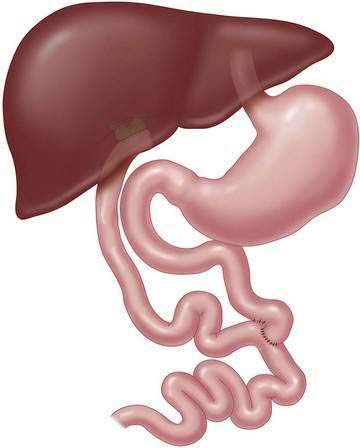
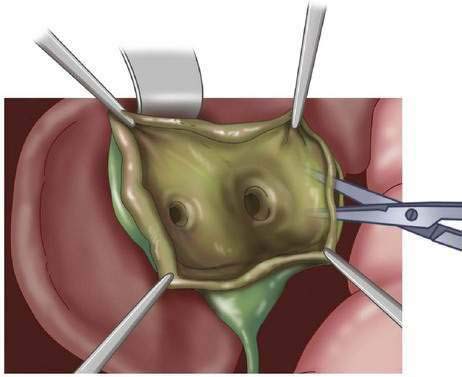
Step 3: Operative Steps
Types I and IV Choledochal Cyst
Type II Choledochal Cyst
Type III Choledochal Cyst
Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Crombleholme TM, Harrison MR, Langer JC, Longaker MT. Biliary appendico-duodenostomy: a nonrefluxing conduit for biliary reconstruction. J Pediatr Surg. 1989;24(7):665-667.
Jun YY, Chen HM, Chen MF. Malignancy in choledochal cysts. Hepato-Gastroenterol. 2002;49:100-103.
Lee H, Hirose S, Bratton B, Farmer D. Initial experience with complex laparoscopic biliary surgery in children: biliary atresia and choledochal cyst. J Pediatr Surg. 2004;39(6):804-807.
Lipsett PA, Pitt H, Colombani P, Boitnott J, Cameron J. Choledochal cyst disease: a changing pattern of presentation. Ann Surg. 1994;220(5):644-652.
MacKenzie TC, Howell LJ, Flake AW, Adzick NS. The management of prenatally diagnosed choledochal cysts. J Pediatr. 2001;36(8):1241-1243.
Schimpl H, Sauer H, Goriupp U, Becker H. Choledochocele: importance of histological evaluation. J Pediatr Surg. 1993;28(12):1562-1565.
Shimotakahara A, Yamataka A, Kobayashi H, et al. Forme fruste choledochal cyst: long-term follow-up with special reference to surgical technique. J Pediatr Surg. 2003;38(12):1833-1836.
Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263-269.
Todani T, Watanabe Y, Toki A, et al. Reoperation of congenital choledochal cyst. Ann Surg. 1988;207(2):142-147.