Chapter 99 Children in the Wilderness
Once the realm of a few adventurous individuals, the wilderness today attracts an ever-broader range of explorers. This includes many in the pediatric age group, as parents seek to share the joys and lessons of wilderness travel with their children. In 2008, of the more than 60 million people participating in backpacking and camping, nearly 25% were younger than 17 years.57 Millions of other children annually visit national parks and recreation areas.
What Makes Children Different?
Size and Shape
Children are distinct from adults in a variety of physical, physiologic, and psychological ways. The most obvious difference is size. During development, children may grow from the average 7-lb (3.18-kg) baby to a 140-lb (63.5-kg) adolescent, a 20-fold difference. Accordingly, medications and fluids must be calculated on an individual basis, based on the weight of the child. Table 99-1 lists average weights for age.
| Age | Weight | |
|---|---|---|
| yr | kg | lb |
| 1 | 10 | 22 |
| 3 | 15 | 33 |
| 6 | 20 | 44 |
| 8 | 25 | 55 |
| 9 | 30 | 66 |
| 11 | 35 | 77 |
| 13 | 45 | 100 |
From U.S. Centers for Disease Control and Prevention National Center for Health Statistics (http://www.cdc.gov/nchs/).
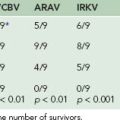
Children are not only smaller than adults, they also have a larger surface-area-to-mass ratio. For example, a 7-lb (3.18-kg) infant has 2.5 times more body surface area per unit weight than a 140-lb (63.5-kg) adult. Not only is the surface area of the young child’s body larger, the head, which is the part of the body most often left exposed, also takes up a larger proportion of the body (Figure 99-1). As a result, children experience greater exposure to environmental factors, such as cold, heat, and solar radiation. They are also more likely to suffer toxic effects from topical agents, such as medications.
Musculoskeletal System
Another key difference between the musculoskeletal systems of children and adults is that children have an open growth plate, or physis, at the ends of long bones. The physis connects the metaphysis to the epiphysis and consists of soft cartilaginous cells that have the consistency of rubber and act as shock absorbers (Figure 99-2). They protect the joint surfaces from suffering the grossly comminuted fractures seen in adults. However, because the growth plate is more vulnerable to injury than are the strong ligaments or capsular tissues that attach to the epiphysis, a true sprain in a child is rare. Any significant juxta-articular tenderness in a child should be assumed to be a growth plate injury and immobilized accordingly. Such an injury is most common at the ankle (lateral malleolus), knee (distal femur), and wrist (distal radius). Physeal fractures have been classified into five Salter–Harris groups (see Figure 99-2). Salter–Harris I and II fractures generally heal without complications. Salter–Harris III and IV fractures often require open reduction of displaced fractures to realign the joint and growth plates and to permit normal growth. A Salter–Harris V fracture has a poor prognosis; impaction and crushing of some or all of the growth plate may result in a bony bridge that inhibits further growth or causes unequal, angulated growth. Consequently, any significant injury, especially if it involves the growth plate, requires full evaluation in a medical facility.
Cardiovascular and Respiratory Systems
Basic physiologic parameters change greatly during the transitions from infancy to childhood to adulthood. Recognizing these differences is important to avoid unnecessary and potentially harmful interventions in healthy children, and to intervene aggressively when abnormal vital signs are truly present. For example, a blood pressure of 70/35 mm Hg, pulse rate of 160 beats/min, and respiratory rate of 50 breaths/min are considered ominous vital signs for an adult. However, these vital signs are normal in a 2-month-old infant. Although blood pressure readings may not be available in a wilderness setting, it is possible to assess the general appearance, work of breathing, respiratory rate, pulse, and peripheral circulation of an ill child. These observations can accurately predict how sick a child is. In general, infants and children have higher respiratory and heart rates and lower blood pressure than do adults. The normal values for various age groups are presented in Table 99-2. It is important to note that children can often maintain normal blood pressure in the face of significant fluid or blood losses. Once blood pressure drops, however, children can deteriorate very rapidly. Therefore, prompt and aggressive fluid resuscitation is essential when other signs of dehydration or volume loss (e.g., tachycardia, increased capillary refill time, cool extremities) are present.
TABLE 99-2 Age-Specific Resting Heart Rate and Respiratory Rate*
| Age | Heart Rate (beats/min) | Respiratory Rate (breaths/min) |
|---|---|---|
| 0-5 mo | 140 ± 40 | 40 ± 12 |
| 6-11 mo | 135 ± 30 | 30 ± 10 |
| 1-2 yr | 120 ± 30 | 25 ± 8 |
| 3-4 yr | 110 ± 30 | 20 ± 6 |
| 5-7 yr | 100 ± 20 | 16 ± 5 |
| 8-11 yr | 90 ± 30 | 16 ± 4 |
| 12-15 yr | 80 ± 20 | 16 ± 3 |
Thermoregulation
Because environmental extremes are often encountered when traveling in wilderness areas, it is important to recognize that thermoregulation is less efficient in children than in adults. A number of physiologic and morphologic differences make children more susceptible than adults to heat illness. During exercise, children generate more metabolic heat per unit mass than do adults. Children also have lower cardiac output at a given metabolic rate, resulting in lower capacity to convey heat from the body core to the periphery. Because they have a larger surface area–to-mass ratio, children also gain heat more rapidly from the environment than do adults when ambient temperature exceeds skin temperature. In hot environments, cooling from conduction, convection, and radiation ceases to be effective, leaving evaporation (sweating) as the only effective means of heat dissipation. Unfortunately, children have a lower capacity for evaporative cooling, presumably because of decreased sweat volume, regional differences in sweat patterns, and a higher sweat point (the rectal temperature when sweating starts).42 Finally, children acclimatize to hot environments at a slower rate than do adults.
Children are also at greater risk for hypothermia. Their larger surface area–to-mass ratio causes them to cool more rapidly than adults in cold environments. Children also have less subcutaneous fat and, therefore, less body insulation. Infants, in particular, have an inefficient shivering mechanism. This makes them particularly vulnerable to cold environments because shivering is the primary means of generating extra heat when humans are cold.4 In general, humans are poorly adapted for cold environments and must rely on adaptive behavioral responses, such as seeking shelter and dressing appropriately, to maintain body heat. Infants and young children are not capable of these responses and must rely on caregivers to provide shelter and appropriate clothing.
Trauma
Blunt trauma is the leading cause of morbidity and mortality in children ages 1 to 18 years. Closed head injuries are responsible for 80% of pediatric trauma deaths.44 Although pedestrian and motor vehicle accidents are the source of many of these injuries, falls and drowning are close behind. Children differ from adults in their susceptibility to injuries from blunt trauma, and the injuries themselves differ. By nature of their smaller size, children’s airways are more prone to obstruction, particularly by their relatively large tongues. Their rib cages are more pliable and hence provide less protection to the lungs and mediastinum. Similarly, the abdominal musculature in children is underdeveloped relative to adults, leaving the intra-abdominal organs more vulnerable to injury. Pelvic fractures are uncommon in children; when they do occur, they rarely result in life-threatening bleeding or genitourinary injury.
General Considerations and Expectations
Children of different ages have different needs and abilities. Expectations regarding distances of travel, pace, and safety issues vary depending on age (Table 99-3). This section explores the key issues regarding wilderness travel with children of various ages and provides general expectations for each age group. A number of helpful books that discuss different aspects of wilderness activities with children are listed under Suggested Readings.
| Age | Expectation | Safety Issues |
|---|---|---|
| 0-2 yr | Distance traveled depends on adults. Use child carriers | Provide “safe play area” (e.g., tent floor, extra tarp laid out), bells on shoes |
| 2-4 yr | Difficult age; stop every 15 min, hike 1-2 miles on own | Dress in bright colors, teach how to use whistle |
| 5-7 yr | Hike 1-3 hr/day, cover 3-4 miles over easy terrain, rest every 30-45 min | Carry whistle (three blows for “I’m lost”), carry own pack with mini first-aid kid and water |
| 8-9 yr | Hike a full day with easy pace, cover 6-7 miles over variable terrain; if 1.2 m (>4 feet) tall, can use framed pack | As for 5-7 yr, plus teach map use and route finding, precondition by increasing maximal distances by <10%/wk, watch for overuse injuries, keep weight of pack <20% of bodyweight |
| 10-12 yr | Hike a full day at moderate pace, cover 8-10 miles over variable terrain | As for 8-9 yr; expand route planning role, compass use |
| Teens | Hike 8-12 miles or more at adult pace; may see a decrease in pace or distance with growth spurt | As for 10-12 yr, but expand survival and wilderness first-aid knowledge. |
First 2 Years
Equipment
Because infants and young children are not capable of extended hikes, they are typically transported in carriers. Most front carriers work well from infancy until an age when babies can sit fairly well, typically 6 to 9 months (Figure 99-3). It is important that a front carrier extend up high enough in the back to completely support a young baby’s head. Once a child is sitting well, back carriers are better (Figure 99-4). Back carriers function on the same principle as framed backpacks, redistributing the weight off the shoulders and onto the hips. Many back carriers are able to stand alone and can double as a highchair. Children must be strapped into back carriers, because it is easy for a child to be catapulted out of a carrier if the adult bends over or falls.
2 to 4 Years
Safety
When selecting campsites, dangerous features, such as steep drop-offs and fast, deep water, should be avoided. Children should be dressed in brightly colored clothing, so they are more easily located if they become lost (Figure 99-5). As children get older, they may carry a whistle to call for help when they are lost. The standard distress signal is three blows to indicate “I’m lost” or “I need help”; the response is two blows to indicate “help is coming.” Parents should teach children to stay put once they discover they are lost and wait to let help come to them. If children panic and start running when they realize they are lost, they increase the chance not only of getting injured but also of traveling farther from the family. The concept of “hug a tree” will be described later in the chapter.
School Age (5 Years and Up)
Travel Expectations
When parents are planning hiking trips, it is important that they have appropriate expectations for children’s evolving abilities (see Table 99-3). Children enrolled in organized sports activities are likely to have greater endurance in the wilderness. A child’s hiking ability can be estimated by walks around the neighborhood or in a local park. If this practice becomes a routine, children become preconditioned, increase their endurance, and learn to pace themselves. More importantly, parents can learn what to expect and can test methods for motivating their children. It is better to underestimate than to overestimate a child’s ability. Parents should also remember that children, like adults, have good and bad days, so allowances should be made.
Environmental Illnesses
Dehydration
Symptoms
As little as a 2% decrease in bodyweight through fluid loss results in mildly increased heart rate, elevated body temperature, and decreased plasma volume. Water losses of 4% to 5% of bodyweight reduce muscular work capacity by 20% to 30%.42 Symptoms of dehydration include weakness, fatigue, nausea, vomiting, and, ultimately, lethargy. In a young child, the first sign may be irritability and loss of appetite. Dehydration also predisposes a child to other environmental hazards, such as hypothermia, hyperthermia, and acute mountain sickness.
Treatment
It is the caregiver’s responsibility to provide fluids and coax the child to drink frequently. For short (<2-hour) periods of activity, water is as efficacious a rehydration solution as are carbohydrate-electrolyte drinks.42 That being said, a small amount of juice or other sweetener diluted in a larger volume of water will often enhance the fluid intake of a child. Avoid undiluted juices or heavily sweetened drinks because they can worsen dehydration; the high carbohydrate load in these drinks promote an osmotic diuresis. A child eating a normal diet does not require electrolyte replacement unless sweating is prolonged or excessive. By closely monitoring a child’s urine output, fluid deficits can be recognized and promptly managed. A child with decreased urine output or dark, concentrated urine needs extra fluids.
Hypothermia
Children cool more rapidly than do adults because they have a relatively large surface area and often lack the knowledge and judgment to initiate behaviors that maintain warmth in a cold environment (see Chapter 5). In addition, they have a more difficult time, physiologically, maintaining body temperature in cold climates, predominantly because they do not shiver as effectively.4 As a result, parents participating in cold weather recreation with children should be able to recognize, treat, and preferably prevent hypothermia and frostbite.
Hypothermia is defined as core body temperature below 35° C (95° F). At this temperature, the body no longer generates enough heat to maintain body functions. The condition is considered mild when the core temperature is 33° to 35° C (91° to 95° F); moderate at temperatures between 28° and 32° C (82° and 90° F), and severe when it is less than 28° C (82° F). The signs and symptoms of hypothermia are listed in Table 99-4, although these may be quite variable. The most important clue to significant hypothermia is altered mental status. An infant may become lethargic and difficult to arouse. An older child may be shivering, stumbling, or appear confused. These signs merit prompt treatment for hypothermia. Of note, the presence or absence of shivering is not a reliable marker of the severity of hypothermia. Physicians should also caution parents that hypothermia can develop at moderate ambient temperatures if adverse climatic conditions are compounded by illness, fatigue, dehydration, inadequate nutrition, or wet clothing.
| Rectal Temperature | Signs and Symptoms | |
|---|---|---|
| Mild | 33°-35° C | Sensation of cold, shivering, increased heart rate, progressive incoordination in hand movements, developing poor judgment |
| (91°-95° F) | ||
| Moderate | 28°-32° C | Loss of shivering, difficulty walking or following commands, paradoxical undressing, increasing confusion, decreased arrhythmia threshold |
| (82°-90° F) | ||
| Severe | <28° C | Rigid muscles, progressive loss of reflexes and voluntary motion, hypotension, bradycardia, hypoventilation, dilated pupils, increasing risk of fatal arrhythmias, appearance of death |
| (<82° F) | ||
Prevention
When preparing for cold weather activities, children should dress in layers to allow clothing to be added or subtracted as necessary (Figure 99-6). This avoids excessive perspiration while maintaining warmth. An inner, wicking layer should be followed by a middle, insulating layer and, finally, by an outer, protective layer.
Because children generally avail themselves of any opportunity to get wet, clothing that maintains low thermal conductance when moist is particularly important. Conductive heat loss may increase fivefold in wet clothing and up to 25-fold if the child is completely immersed in water. Traditional wool retains warmth when wet because of its unique ability to suspend water vapor within the fibers; however, it is heavier than synthetics and takes much longer to dry. Cotton has a high thermal conductance that increases greatly when wet and is, therefore, a poor choice for wilderness activities in cold weather. Synthetic materials (polypropylene, Capilene, Thermax, Coolmax) wick moisture away from the skin and dry quickly, making them ideal for an inner layer. Finely woven merino wool also provides these same advantages as a wicking layer. The middle, insulating layer may incorporate wool, polyester pile or fleece, down, or similar materials. Finally, windproof and water-resistant outer garments (e.g., Gore-Tex) decrease heat loss from convection and keep children dry. Hats and mittens are also essential; the uncovered head of a child dissipates up to 70% of total body heat production at an ambient temperature of 5° C (41° F).4
Frostbite
Localized cold injury can result in frostbite (see Chapter 8). Predisposing factors include wet skin, constricting garments that hinder blood circulation, fatigue, dehydration, contact with cold surfaces, and wind. If skin temperature drops below 10° C (50° F), cutaneous sensation is generally abolished and injury may go unnoticed. Skin cooled to −4° C (25° F) freezes.
Frostbite has traditionally been divided into degrees of injury, much like burns. Determination of depth of injury should occur 24 to 48 hours after rewarming; prior to this, frostbitten skin generally appears hard and feels numb. Skin with superficial frostbite is typically swollen, pink or erythematous, painful, somewhat warm, and often blistered. Sites with deep frostbite are cooler, not edematous, pale, anesthetic, and do not have blisters or bullae. In children, frostbite that extends into bone may affect the growth plate and result in skeletal deformities.4 Verbal children will frequently report cold hands and feet, but adults should be vigilant about checking the extremities and noses/ears of nonverbal children, particularly those poorly visible in back carriers. A mirror, frequently used, can assist in this regard. Reports of small children developing frostbite and hypothermia while being carried on the backs of adults engaged in outdoor winter pursuits are not infrequent.
Hyperthermia
Families participating in wilderness activities in hot climates must take special precautions to avoid heat illnesses (see Chapters 10 and 11). Children do not tolerate the demands of exercise in the heat as well as adults. They generate more heat per kilogram and are less able to disperse heat from the core to the periphery. Parents planning wilderness ventures with children in hot climates can follow some simple guidelines for avoiding heat illness. The most obvious entails reducing the duration and intensity of activities under conditions of high climatic heat stress. The likelihood of heat illness depends on relative humidity, wind velocity, and radiant heat, as well as standard dry-bulb thermometer temperature. Figure 99-7 gives a rough guide for activity levels based on temperature and relative humidity.
Prevention
Children should be fully hydrated before prolonged exercise and actively encouraged to drink fluids at regular intervals.42 Infants and neonates are most vulnerable to heat illness. Under high climatic heat stress, infants fed undiluted cow’s milk or formula may develop marked salt retention and dehydration. They should be given extra water or dilute feedings. The lower osmolar load of breast milk appears to protect against heat illness and hypernatremia.
Sun Damage
Hazards of overexposure to sunlight include sunburn, photoaging, skin cancer, and phototoxic and photoallergic reactions (see Chapter 14). Climatic changes such as global warming and ozone degradation have increased these hazards.54 Preventing ultraviolet damage to skin should begin in childhood, as 50% to 80% of a person’s lifetime sun exposure occurs before 21 years of age.25,48 Adolescence is the period when children are most at risk. In one study, 83% of children 12 to 18 years old reported at least one sunburn per summer; 36% reported three or more sunburns per summer.25 Recent evidence suggests that the risk of developing malignant melanoma increases significantly with the number of sunburns in childhood.19 This risk is even higher if a child is light-skinned with a propensity to burn rather than tan. Tolerance to sun exposure is determined by the amount of melanin in skin and ability of skin to produce melanin in response to sunlight. In general, children have lower melanin levels and thinner skin than do adults and are, therefore, at greater risk of sun damage.
The harmful effects of ultraviolet radiation from the sun can be reduced if parents are educated regarding the dangers of sun exposure and encouraged to use sun-protective clothing and sunscreens early in their children’s lives. One study demonstrated 60% reduction in childhood sunburns with good parental role-modeling and sunscreen vigilance.48 Regular use of sunscreen with sun protection factor (SPF) of at least 15 for the first 18 years of life reduces a person’s lifetime risk of developing nonmelanoma skin cancer by 78%.27
Prevention
The most effective means of preventing sun damage is use of protective clothing and avoidance of excessive sun exposure. Midday hours, particularly around highly reflective surfaces (e.g., water, sand, snow), at high altitude and at the equator are the most dangerous in terms of quantity of ultraviolet exposure. Shady areas should be used for activities during these times. Hats with wide brims and neck drapes help to protect the face and neck from sun exposure (Figure 99-8). Clothing made from tightly woven fabrics is more protective than is clothing made from loosely woven fabric. For example, loosely woven fabrics, such as those used in most T-shirts, have an SPF of only 5. Most clothing loses more of its sun protective effect when wet. Several manufacturers are marketing high-SPF (25 to 50) protective clothing (http://www.coolibar.com; http://www.sunprotectiveclothing.com). This specialized clothing is cool and lightweight, dries quickly, and can maintain its full SPF capabilities when wet (Figure 99-8). Caution is advised on overcast days, because 80% of the sun’s rays still reach the earth even when the sun is not visible.27 In addition, because clouds filter out heat from infrared rays, children feel more comfortable and tend to stay out longer, therefore increasing their overall UV exposure.

FIGURE 99-8 Child with appropriate sun wear: protective clothing, wide-brimmed hat, and sunglasses.
(Courtesy Judith R. Klein, MD.)
Proper eye protection is often overlooked in infants and young children. Excessive ultraviolet light, particularly during snow and water activities, can result in ultraviolet keratitis (see Chapter 28) with even brief exposures. Properly fitting sunglasses that transmit less than 10% of ultraviolet rays should be part of a child’s outdoor activity armamentarium (Figure 99-8). Side shields and polarizing lenses are particularly important in snow conditions.
Sunscreens
Sunscreens formulated with a variety of different agents to prevent UV damage to the skin include physical blocks, chemical blocks, and antioxidants. Physical blocks, such as zinc oxide and titanium dioxide, reflect ultraviolet light and do not penetrate the skin. Chemical blocks prevent ultraviolet light from entering skin, and are themselves absorbed into skin. Chemical blocks have ingredients that block UVB, UVA, or both. Agents that block UVB include PABA, cinnamates, salicylates, and anthranilates; those that block less potent UVA rays include avobenzone and the anthranilates. Benzophenones, oxybenzone, and the physical blocking agents protect against both UVA and UVB.27 Antioxidants present in sunscreens include Vitamins C and E, resveratrol, and pomegranate. These agents help to repair skin damage. Sunscreens that combine protective ingredients with antioxidants are the most effective. The sun protection factor (SPF) is a measure of a sunscreen’s effectiveness. It is measured in terms of the minimal dose (in length of time) of UV radiation required to cause skin erythema. Sunscreens with SPF 30 or higher provide a superior degree of photoprotection and almost completely prevent cellular changes seen with sunburn.27
Overall, there is little difference between child and adult sunscreens except for price. Parents should select sunscreens based on ingredients. Physical blocks are preferred for children because they are difficult to wash/rub off and do not degrade in the sun. Therefore, they do not need to be reapplied with as great frequency as do chemical sunscreens. Zinc oxide can be quite colorful, whereas titanium dioxide is colorless. Apply a thick coat of sunscreen at least half an hour before outdoor activity. Sunscreens must be applied in adequate quantity to provide the SPF indicated on the bottle.51 Select a sunscreen with an SPF of at least 15, but preferably greater than 30. Waterproof sunscreens are preferred if children are anywhere near water, because these products maintain efficacy for up to 80 minutes of water immersion. Sunscreens should be reapplied at least every 2 hours (or more frequently) during prolonged water immersion or excessive sweating. Cream and lotion sunscreens provide superior coverage to spray-on formulations because they can be applied evenly and in the quantities required to provide effective sun protection. Infants younger than age 6 months should be outfitted with hats and protective clothing and should placed in the shade. Sunscreens in this age group should be limited to small areas of skin only, because infant skin is thin and chemically sensitive.
Drowning
According to the Centers for Disease Control, drowning (see Chapter 75) is the number two cause of injury-related death in children, resulting in more than 900 fatalities in children under 14 in 2005.66 Of all deaths among children age 1 to 4 years in 2005, 30% were the result of drowning.66 Those most at risk are unsupervised toddlers and male teenagers, in particular, those with inadequate swimming skills and poor judgment. Morbidity and mortality result from asphyxiation, hypothermia, and/or trauma.
High-Altitude Illness
High-altitude illness (see Chapter 1) can be viewed as a continuum from acute mountain sickness (AMS) to life-threatening conditions such as high-altitude pulmonary edema (HAPE) and high-altitude cerebral edema (HACE). AMS usually develops within 24 hours of ascent. The incidence and severity of AMS depend on individual susceptibility, as well as rate of ascent and altitude attained. In one study, 37% of children who ascended rapidly to 3500 m (11,500 feet) developed AMS.6 Other studies have shown even higher incidences of AMS in children and have suggested that children are more susceptible to hypobaric hypoxia than are adults.43
Prevention
The safest and most effective method of preventing high-altitude illness is to allow for acclimatization via graded ascent. No precise, scientifically proved guidelines exist, given the markedly variable individual susceptibility to altitude illness. However, general recommendations for children (and adults) without altitude experience are listed in Box 99-1. After day trips to higher altitude, children should return to lower altitude to sleep in order to aid acclimatization. The sleeping altitude is particularly important with regard to development of symptoms. A high-carbohydrate diet and plenty of fluids can also help to reduce the risk of high-altitude illness.
BOX 99-1 Preventing High-Altitude Illness
Acetazolamide has been convincingly shown to reduce the incidence of AMS in adults.20 Pretreatment with this agent mimics the acclimatized state by inducing hyperchloremic metabolic acidosis, allowing for a compensatory increase in respiration. There are no published studies of its efficacy in children, but clinical experience suggests that it is beneficial. The primary indication for acetazolamide prophylaxis in children is a history of recurrent AMS despite graded ascent.43 Acetazolamide is given at 5 mg/kg/day, in two divided doses, up to a maximum daily dosage of 250 mg. It should be started 24 hours before ascent and continued for 3 to 5 days while at maximal altitude. It can be discontinued once descent has begun. Side effects include nausea, mild somnolence, and paresthesias that can be particularly bothersome in children. Dexamethasone also prevents or reduces symptoms of AMS in adults, but its use is discouraged in the prevention of AMS in children, because it masks early symptoms of mountain sickness and thereby encourages continued ascent. Ginkgo biloba has also been studied recently as an herbal alternative to acetazolamide for the prevention of AMS; unfortunately, its efficacy is uncertain because of variability in commercially available gingko formulations.36 Salmeterol, an inhaled long-acting β-agonist, has also been studied as a prophylactic agent against HAPE in adults, but it has not been evaluated in children.
Treatment
Treatment of mild AMS requires prompt recognition of symptoms, cessation of ascent, and allowance of time for acclimatization to occur. Proceeding to higher altitude in the presence of symptoms is strongly contraindicated and may lead to the life-threatening conditions HAPE and HACE. Symptomatic therapy includes rest, acetaminophen for headache, and adequate hydration. Promethazine (Phenergan) or ondansetron (Zofran) may be used to relieve nausea and vomiting. Dystonia in response to phenothiazines, such as promethazine, occurs disproportionately in young children, so ondansetron is preferred. Promethazine is given at 0.2 to 0.5 mg/kg/dose up to 25 mg every 6 hours, preferably per rectum; ondansetron is given orally at 0.1 to 0.15 mg/kg up to 4 mg every 4 hours. If symptoms resolve, the child may continue to ascend slowly. However, if symptoms progress or fail to improve, descent is mandatory. Although descent should proceed as far as necessary for improvement, 500 to 1000 m (1600 to 3200 feet) is often sufficient. If immediate descent is not possible, oxygen should be administered if available. Studies examining dexamethasone and acetazolamide for treatment of AMS suggest that both are effective.20 Dexamethasone should be reserved for patients with severe AMS or HACE. The symptoms of HACE or HAPE demand immediate descent and possible evacuation.
Bites and Stings
Bites and stings occur commonly in the pediatric age group. In 2008, the American Association of Poison Control Centers reported that more than 25,000, or roughly one-third, of reported bites and stings occurred in individuals under the age of 20 years.8 Remarkably, no fatalities were reported in this age group. This emphasizes the need for appropriate triage to determine which children require aggressive therapy so that potentially harmful field interventions can be avoided.
Snakes
Of the 8000 venomous snakebites that are estimated to occur in the United States each year, about 20% occur in people under the age of 20 years.8 Although mortality from domestic snakebites is uncommon, about 20% of snakebite-related deaths typically occur in children under the age of 5 years. More than two-thirds of bites in children are on the lower extremities; these are predominantly in younger children walking or running over rocks and in brush. Most snakebites can be prevented. Children should be instructed not to handle snakes, not to reach blindly into crevices, and to avoid turning over rocks and fallen limbs. A useful adage is that hands and feet should never go where the eyes cannot see. When walking through endemic areas, hikers should stay on trails and wear long, loose pants, and boots that extend above the ankle. Campsites should be on open ground, away from wood piles or rock piles.
If a bite occurs, the child should back well away from the snake and be calmed. Agitation and movement of the bitten extremity promote venom circulation. The wound should be cleansed rapidly and any constricting items of clothing or jewelry removed. The bitten extremity should be immobilized promptly and positioned at the level of the heart. No incision over the bite should be made. The use of mechanical suction (e.g., Sawyer extractor) is ineffective at removing snakebite venom and can worsen tissue ischemia in the 99% of endemic snakebites that are inflicted by members of the crotalid family (rattlesnakes, cottonmouths, copperheads).1 Advanced techniques for potentially limiting venom spread, particularly with exotic snake envenomations, are discussed in detail in Chapters 54 and 55. All victims of potentially poisonous snakebites should be transported to a medical facility for prompt evaluation, local wound care, and possible antivenom administration. Crotalidae Polyvalent Immune Fab antivenom (CroFab, Protherics Inc.) has been shown to be safe and effective in children, particularly if administered early.28
Hymenoptera
Hymenoptera (bees, wasps, hornets, and ants) stings are the most common cause of envenomations in children (see Chapter 50). Although Hymenoptera venom possesses intrinsic toxicity, the amount delivered is small and multiple stings are necessary for significant human morbidity. However, the venom components are potent antigens capable of producing IgE-mediated anaphylaxis in sensitized individuals. Although children appear less susceptible to systemic reactions than are adults, physicians should educate parents in the management of Hymenoptera stings, particularly if a child has previously had a severe reaction.
Hymenoptera stings usually produce local pain, swelling, and erythema. If a stinger is imbedded, it should be removed as quickly as possibly by whatever means available, because the speed of removal of the stinger is far more important than the method of extraction.65 Within 20 seconds, 90% of the contents of the venom sac are discharged into the victim, and 100% within 1 minute.52 Applying ice or cool compresses reduces pain and swelling. Elevation and immobilization are indicated for large local reactions on extremities. In older children, oral antihistamines may provide additional symptomatic relief.
Mosquitoes
Mosquitoes not only present a high nuisance potential but also serve as vectors of disease (see Chapter 48). A number of steps can be taken to avoid mosquito bites and the diseases they carry (Box 99-2). A proper wardrobe provides an excellent physical barrier and is the first defense against mosquitoes. This should include ankle-high footwear, pants cinched at the ankles or tucked into socks, a long-sleeved shirt, and a full-brimmed hat. Mosquito head netting draped over a child’s hat will protect the face and neck (Figure 99-9). Mosquito netting, especially in the sleeping area, has been found to reduce the mosquito attack rate by 97%.59
BOX 99-2 Mosquito Avoidance
Repellents containing DEET (N,N-diethyl-m-toluamide) are effective against mosquitoes, ticks, black flies, and many other arthropods. Although generally of low toxicity, high concentrations of DEET can cause dermatitis with erythema, bullae, skin necrosis, and residual scarring. DEET is also absorbed cutaneously, and rare toxic encephalopathy associated with its use has been reported. A large study based on data from the American Association of Poison Control Centers refuted the commonly held belief that children are more susceptible to DEET toxicity. The study demonstrated that children actually have less severe outcomes after DEET exposures than do adults.5 Although products containing 100% DEET are commercially available, long-acting formulations of ≤35% DEET appear equally effective in protecting against mosquitoes, with much less potential for toxicity.47,63 Although available data do not permit precise safety guidelines, infants younger than 6 months should avoid DEET, but those older than 6 months can use products with up to 30% to 35% DEET. The repellent effect can last up to 8 hours, but heavy perspiration or swimming should prompt reapplication every 6 to 8 hours. Dawn and dusk are particularly risky times; outdoor activities should be limited at these times if possible. Parents should not allow children under 8 years old to apply DEET to themselves, because of the risk of DEET exposure to eyes or mouth in this age group. DEET products can be applied over other creams such as sunscreen to minimize absorption and maximize repellent effect. Parents should also be cautioned to keep DEET out of the reach of small children, because ingestion may be fatal.
Picaridin (Bayrepel) is a more recently developed alternative to DEET. Commonly used in Europe and Australia, it is odorless, minimally toxic, and considered by the World Health Organization (WHO) and the U.S. Environmental Protection Agency (EPA) to be an effective insect repellent. Anecdotal reports, however, suggest that it might not be as effective as DEET and may not repel as broad an array of arthropods (e.g., flies). Oil of lemon eucalyptus is an EPA-approved insect repellent, but its efficacy is similar to that of low-concentration DEET products. Therefore, its use is not recommended in areas heavily infested with mosquitoes. Other alternative insect repellents are widely available and often more appealing to parents, because their active ingredients are “natural.” Unfortunately, agents such as citronella, lavender oil, and soybean oils have demonstrated very limited efficacy in repelling arthropods.59 Although natural products may be acceptable in areas where mosquitoes do not carry disease, in U.S. areas with persistently active West Nile Virus, and certainly in much of the tropical developing world where malaria and dengue fever are endemic, these products are simply inadequate. In addition, the above oils have been associated with aspiration pneumonitis when accidentally ingested by young children.
The pesticide permethrin, available as a 0.5% spray or soaking liquid (Permanone, Duranon Tick Repellent), is safe and effective against arthropods, especially ticks. Unlike DEET repellents, these permethrin products are applied to fabric or netting, not to skin. Permethrins as a class have low toxicity in mammals. The combination of DEET applied to exposed skin and permethrin treatment of clothing is particularly effective in protecting against mosquito bites and ticks. This combination can reduce mosquito bites by up to 99% for up to 8 hours.59 The protective effect of mosquito netting is also greatly enhanced when the netting is impregnated with permethrin. These effects are longer lasting with permethrin soaks (up to 20 washings) than with permethrin spraying of clothing or netting.
West Nile Virus (WNV) continues to be a concern across the United States, although the number of cases (>700 in 2009) and fatalities (33 in 2009) have dropped since the peak in 2006 (see Chapter 48).67 WNV is a zoonotic disease transmitted from animal hosts to humans via infected Culex mosquitoes. Twenty percent of infected individuals develop a mild nonspecific febrile illness lasting less than a week. More than one-half of reported cases in 2009 developed neurologic manifestations.67 Protection against mosquito bites is the only means of prevention of WNV-related disease in humans.
Ticks
Like mosquitoes, ticks serve as vectors for disease, most notably Lyme disease (see Chapter 51). Lyme disease is rare on the Pacific coast but endemic in the Northeast, where up to 30% to 50% of Ixodid ticks are carriers.21 The number of cases in the United States each year continues to rise, numbering nearly 30,000 in 2008.50 Transmission of the Lyme spirochete, Borrelia burgdorferi, typically requires 48 to 72 hours or more of tick contact.56 Therefore, tick checks should be conducted regularly while traveling through wilderness areas. If a tick is found imbedded in skin, it should be grasped with forceps close to the skin surface and gentle traction should be applied. The use of alcohol or open flames for removal is strongly discouraged, because these techniques do not tend to work and can induce tick salivation or regurgitation into the wound.
Lost Children and Survival
Lost children in the wilderness is a common, preventable problem. Children should be taught to recognize landmarks and to turn around and look backward periodically to familiarize themselves with the terrain. Those who are capable of reading a compass and topographic map should carry these items at all times. Young children should wear brightly colored clothing to facilitate a search should they become lost (Figure 99-5). They should carry a whistle around their necks and be taught the universal signal for help: three blasts in a row. It should be emphasized to the child that the whistle is intended for emergency use only. Portable two-way radios can also be used for emergency communication if a child is lost. Depending on the model, the range can extend 2 to 5 miles, but mountains and ridges can cause interference. As soon as they are able to carry a backpack, children should also be equipped with some survival items. A flashlight, bottle of water, extra food, and a few brightly colored garbage bags can make all the difference for a child forced to spend several hours or a night out in the wilderness. Also, all children should either know or carry with them a piece of paper with their parent’s name, address, and phone number. Older children who venture out without their parents should always tell an adult where they are going, with whom, and when they expect to return.
A few programs, such as Hug-a-Tree (http://www.gpsar.org/hugatree.html), instruct children in the basics of survival when lost. The title of the program is intended to remind children of three important tenets of survival when lost: stay in one place to facilitate any search, take advantage of the natural shelter provided by a tree, and feel the security and calming effects of a large natural protector. By hugging a tree and not wandering around, children can work on making signals out of rocks or branches, thereby indicating their location. Children should be taught to make themselves look big/loud (coats/arms in the air, blow whistle) or to lay down with arms out if they hear a helicopter. Children should learn to avoid getting wet (e.g., wear garbage bag if raining, avoid rivers or lakes), to wear a hat, and to stuff pine needles or dry grasses into their clothes to insulate themselves if they are cold. Children can practice making temporary shelters out of logs, branches, and leaves and thereby experience the warmth and protection provided by these natural features. They should avoid laying directly on the ground and should use leaves and branches to insulate themselves from the cold earth or snow. Children should be advised not to eat anything with which they are not familiar. The program also reminds children that there are no animals “out there” in the United States that will hurt them (e.g., “lions, tigers, bears”) and that they should yell at any noises that they hear. Finally, children should be reminded that they will not be punished for getting lost and that lots of people will be looking for them, so they should just stay put. Parents should also be encouraged to mobilize search and rescue resources early, before time and foul weather obscure a child’s tracks.
Older children and adolescents who plan on spending time in the wilderness should be encouraged to participate in a program that teaches basic survival and first-aid skills. Several organizations, such as Lifeschool’s Go Adventures in Bodega, California (http://www.goadventure.org/) and the National Outdoor Leadership School (NOLS: http://www.nols.edu), provide instruction for children. Lifeschool is intended as an introduction to the backcountry for children ages 12 to 18 years, whereas NOLS provides more technical instruction in various forms of wilderness travel, in addition to first-aid and survival training.
Homesickness
Most children experience some degree of distress when faced with separation from home, particularly when they are not accompanied by a parent. Predisposing factors to the depression and anxiety referred to as homesickness include young age, little prior separation experience, high parental separation anxiety, great perceived distance from home, few initial positive experiences after separation, preexisting anxiety or depression, and little perceived control over the situation.62 Parents should be encouraged to introduce short periods of separation from home and family, leading up to longer periods. They should discuss the exciting aspects of any future adventure and encourage active decision making regarding activities and destination. Parents should also try to alleviate their own separation anxiety and ensure positive early post-separation experiences for their child.62 The presence of familiar faces, such as friends or favorite playmates, can significantly reduce a child’s feeling of homesickness. Activities that include a child’s favorite games and meals will be remembered by the child as fun experiences in which he or she would like to reengage. Through careful planning and coordination, parents can do much to allay the fear and anxiety of children as they travel away from home.
Foreign Travel with Children
Visits to foreign countries provide superb educational, social, and cultural experiences for children. An estimated 1.9 million children travel abroad each year.63 Unfortunately, traveling to wilderness or rural areas within developing nations entails not only the risks of wilderness travel but also of poor sanitation conditions with exposure to bacteria, viruses, protozoa, and helminths not usually seen in the developed world. Although there is little consensus among experts, parents should be made aware of the greater risks of traveling to a developing country with a child under 2 years of age. The increased risk is the result of incomplete immunizations, an underdeveloped or naive immune system, poor hygiene, and age- and weight-based contraindications for vaccinations and various medications.
It is the role of some physicians to provide guidance and information to parents planning foreign travel. The emergence and widespread availability of the Internet has provided both physicians and travelers with easily accessible and up-to-the-minute guides to disease outbreaks, immunizations, and symptoms/treatments for various tropical diseases. Reliable sources for this type of information are listed in Table 99-5.
TABLE 99-5 Resources for Current Travel Immunizations and Malaria Prophylaxis Recommendations
| Resource Name | URL | Comments |
|---|---|---|
| U.S. Centers for Disease Control and Prevention (CDC) | http://www.cdc.gov | General website |
| http://www.cdc.gov/travel/ | Index of travel information, vaccines, disease outbreaks by destination country | |
| http://www.cdc.gov/mmwr | Morbidity and Mortality Weekly Report online: International bulletin on disease outbreaks | |
| http://www.cdc.gov/nip | National Immunization Program—vaccine information | |
| World Health Organization | http://www.who.int/en/ | Latest information on disease outbreaks |
| Travel Medicine Providers | http://www.tripprep.com | Vaccinations, epidemics, travel medicine providers |
| Travel Internationally with Your Kids | http://www.travelwithyourkids.com/ | Parent-friendly website with much practical information |
General Recommendations
Physicians should emphasize to families that risk avoidance is the most important aspect of safe travel. The basic tenets of safe foreign travel with children are listed in Box 99-3. Parents should select transportation, activities, and overnight settings carefully to avoid unnecessary hazards. Freshwater swimming should be avoided in developing countries to prevent parasitic infections such as schistosomiasis. Where swimming is appropriate, parents should provide close supervision. In one study in Washington State, drowning was the leading cause of pediatric mortality in the wilderness, followed by closed head injury and exposure.46 Because traumatic injury is the leading cause of morbidity and mortality among children, prevention is key. Protective devices such as car seats, helmets, personal flotation devices, and protective clothing and pads should be used as often as possible (Figure 99-10). Do not assume any of these items is available in the destination country. Skin protection is also vital in the outdoors, particularly in tropical environments. The use of closed shoes can prevent infections with various hookworms, Strongyloides, and other parasites that enter through the skin. Closed shoes also protect feet from injuries that can result in wounds infected with Staphylococcus aureus and other organisms that grow vigorously in the tropics. Clothing should be selected carefully based on ambient temperature and expected conditions. Even in hot, sunny climates, light, high-SPF clothing should cover as much body surface as possible to provide protection from parasites, insects, and ultraviolet light. Sunscreen should be used liberally and reapplied every few hours, particularly after swimming.
BOX 99-3 Risk Avoidance During Travel
Parents should be advised to take great care in selecting foods and safe drinking water for themselves and their children, who are particularly vulnerable to disease (Box 99-4). All foods should be either well cooked, canned, or peeled. All milk products should be either pasteurized or boiled to avoid diarrheal illness and tick-borne encephalitis. Water should never be consumed from the tap; only bottled, 1-minute-boiled, or ultraviolet (SteriPEN) or chemically treated (iodine) and microfiltered (0.2-µm pore size) water should be ingested. In certain areas, even bottled water is suspect. Breastfeeding is safest for young infants. If formula is used, only properly disinfected water should be used for its preparation. Finally, good and frequent hand-washing, particularly with infants and toddlers and especially around mealtimes, successfully interrupts the fecal–oral passage of disease.
Parents should also focus their efforts on avoiding contact between their children and insects or wild animals. Mosquitoes and ticks can be avoided by limiting outdoor activities between dusk and dawn and by wearing protective clothing and repellent (see Box 99-2). As mentioned previously, DEET is an effective repellent but should not be used at concentrations greater than 35% in children because of the risk of toxicity.59 Children’s hands should be free of DEET to prevent accidental eye and mouth contact. Picaridin is an alternative but anecdotal reports have suggested that it is not as effective as DEET and scientific studies have not confirmed its efficacy against flies (e.g., tsetse). Therefore, it should not be considered the repellent of choice in areas with disease-carrying insects. Outer clothing and bed netting should be treated with permethrin. Check for ticks daily when in tick-infested areas. Children should be warned to watch where they place their hands and feet (in crevices, unattended shoes, sleeping bags) to avoid the unexpected arthropod or snake.
Immunizations
Foreign travel with children requires advance planning because vaccines recommended for travel to certain countries may take up to 6 weeks to complete. The Centers for Disease Control and Prevention (CDC) website (http://www.cdc.gov/travel) provides up-to-date information on immunizations and prophylaxis based on the following:
Vaccines may be categorized as routine (hepatitis B, polio, diphtheria–tetanus–pertussis, Haemophilus influenzae B, pneumococcus, rotavirus, measles–mumps–rubella, varicella, hepatitis A, meningococcus), seasonally or geographically indicated or required (influenza, yellow fever, typhoid, immunoglobulin [Ig]), and indicated for extended stay (Japanese encephalitis, rabies)64 (Table 99-6). The indications, dosages, and schedules for administration of these immunizations are listed in Table 99-7. The risk of acquiring diseases covered by many routine childhood immunizations is greater when traveling to developing countries because of inconsistencies in local immunization practices and subsequent loss of herd immunity. Children who have not completed their primary series of immunizations may require acceleration of the vaccination schedule or extra doses to maximize protection before travel. The minimum age at which some vaccinations can be given is listed in Table 99-7. In addition, seasonal influenza A vaccine should be given to all children older than 6 months traveling during influenza season: December to April in the northern hemisphere and April to October in the southern hemisphere. Rotavirus vaccine (Rotateq) is also strongly recommended for young infants traveling abroad. Rotavirus is the most common cause of acute gastroenteritis (AGE) in young children, with 80% of children infected by the age of 5 years prior to vaccine introduction.15 In the developing world, it is responsible for the deaths of more than 500,000 children under 5 years. As with many other diseases, children are more likely to develop AGE while traveling, so vaccination is an important preventive tool. Finally, the vaccine against meningococcus (MPSV4 or MCV4), now routine in adolescents, should be administered to all children older than age 2 years traveling to endemic areas or locales with regional epidemics. If travel to such an area is essential for a younger child, the vaccine (MPSV4) does have some, albeit modest, efficacy in infants as young as 3 months.64 Generally, children younger than age 2 years should avoid travel to such areas.
| Type of Vaccine | Examples |
|---|---|
| Routine | Hepatitis B, polio, diphtheria–tetanus–pertussis (DTaP), Haemophilus influenzae B (Hib), pneumococcal (PCV-13), rotavirus (Rotateq) measles–mumps–rubella (MMR), varicella (VZV), Hepatitis A, meningococcal |
| Required or seasonally/geographically indicated for travel | Yellow fever, typhoid, meningococcal, influenza (seasonal), immunoglobulin (Ig) |
| Extended stay | Rabies, Japanese encephalitis |
From U.S. Centers for Disease Control and Prevention (http://wwwnc.cdc.gov/travel/yellowbook/2010/chapter-7/vaccine-recommendations-for-infants-and-children.aspx).
Ideally, a medical visit to discuss travel plans and start immunizations should be made 6 weeks before travel. Not all immunologic agents recommended for travel are compatible and some require multiple doses. Therefore, selection of immunizations to be given at any one time and the interval between immunizations are important. Table 99-8 presents recommendations for the timing and sequence of specific travel immunizations. In general, all toxoid, recombinant, inactivated, and live-attenuated vaccines may be given simultaneously. Live-attenuated vaccines should be given either simultaneously or at least 30 days apart to avoid reduced immunoreactivity to each vaccine.
TABLE 99-8 Recommended Timing and Sequence of Non-routine Immunizations for Foreign Travel
| 4-6 Weeks Before Departure | 1 Week After Initial Visit | Week of Departure |
|---|---|---|
| Hepatitis A (need second dose 6-12 mo later) | — | or Immunoglobulin (Ig) for hepatitis A prevention |
| Yellow fever | — | |
| Typhoid ViCPS or Ty21a | — | |
| Meningococcal | — | Meningococcal (if not given at initial visit) |
| Japanese encephalitis Rabies |
Japanese encephalitis Rabies |
Japanese encephalitis Rabies |
Give only immunizations indicated for area of travel, length of stay, and age of child.
Simultaneous administration of routine and travel-related vaccines is acceptable with the exception of measles–mumps–rubella vaccine or varicella vaccine with Ig. Administer Ig at least 3 weeks after these live virus vaccines.
In the United States, hepatitis A vaccine is recommended for children older than age 2 years. Of note, the World Health Organization (WHO) recommendations include children age 1 year and older. For children younger than age 1 year or for those unable to receive this vaccine more than 2 weeks before travel, Ig can provide passive hepatitis A prophylaxis. Administration of Ig interferes with the humoral response to some of the live-attenuated virus vaccines, such as measles, mumps, and rubella (MMR) and varicella. If Ig is given first, then these vaccinations should be delayed by at least 6 weeks, and preferably by 3 months, to obtain an adequate immunogenic response.22 When both are needed for travel, it is best to give MMR or varicella vaccine first; the Ig can be given closer to the time of travel, at least 2 weeks and preferably 4 weeks later. Ig does not interfere with antibody production after oral polio or yellow fever vaccines and may be given at the same visit. Yellow fever vaccination is often a requirement for travel to certain countries in Africa and South America. Infants older than age 9 months can receive this live virus vaccination, but younger infants are at risk for vaccine-related encephalitis and should not travel to areas where yellow fever is endemic.64
Prophylaxis: Malaria
Globally, malaria infects roughly 300 million people each year and results in 1 million deaths.68 Children younger than 5 years are particularly vulnerable and represent more than 75% of the fatalities from this disease. In fact, in Africa, malaria is responsible for 20% of all childhood deaths. The risk of acquiring malaria (see Chapter 49) during visits to developing countries in the tropics is significant. Even areas where the overall risk is relatively low may have foci of intense transmission. Of the more than 10,000 cases of malaria diagnosed in the United States and reported to the CDC between 1997 and 2006, nearly 60% came from Sub-Saharan Africa, 14% from Asia, and 13% from Caribbean nations.41 In 2007, 20% of the roughly 1500 cases of malaria in the United States reported to the CDC were in children.
Protective measures to prevent mosquito bites help interrupt the transmission of malaria but are not foolproof (see Box 99-2). Therefore, chemoprophylaxis is highly recommended for travelers to countries where malaria is endemic. Plasmodium falciparum and Plasmodium vivax are the two species most often responsible for malaria. The most lethal plasmodium, P. falciparum, has developed widespread resistance to chloroquine and in some areas (extreme northern and southern Thailand, Cambodia, Burma) resistance to mefloquine. Therefore, the choice of prophylactic agent is based primarily on the presence of resistant malaria in the area of travel. The age/weight and medical history of the child are additional determinants of the appropriate prophylactic agent. Table 99-9 lists the available options for malaria chemoprophylaxis.
| Medication | Indications/Contraindications | Dosing |
|---|---|---|
| Chloroquine (Aralen) (liquid form is Nivaquine—not available in United States) | Travel to chloroquine-sensitive areas (Caribbean, Central America north of Panama, Middle East) | 5 mg base/kg q wk up to 300 mg for 1 wk before until 4 wk postexposure; 10 mg/ mL-form available outside United States |
| Mefloquine (Lariam) | Travel to chloroquine-resistant/mefloquine-sensitive area. Do not use in setting of epilepsy, psychiatric illness, cardiac arrhythmias | Give 1 wk pre- until 4 wk post; q wk |
| Dosage: | ||
| 5-10 kg (11-22 lb): 5 mg/kg/wk | ||
10-20 kg (22-44 lb):  tab q wk tab q wk |
||
20-30 kg (44-66 lb):  tab q wk tab q wk |
||
30-45 kg (66-99 lb):  tab q wk tab q wk |
||
| >45 kg (>99 lb): 1 tab (250 mg) | ||
| Atovaquone (A) + Proguanil (P) (Malarone) | Travel to chloroquine- or mefloquine-resistant areas Contraindicated if creatinine clearance <30 mL/min | Pediatric tab dosing: 62.5 mg A/25 mg P |
5-8 kg (11-18 lb):  tab qd tab qd |
||
8-10 kg (18-22 lb):  tab qd tab qd |
||
| 10-20 kg (22-44 lb): 1 tab qd | ||
| 21-30 kg (46-66 lb): 2 tabs qd | ||
| 31-40 kg (68-88 lb): 3 tabs qd | ||
| >40 kg (>88 lb): 1 adult tab qd | ||
| 2 days pre- until 7 days postexposure | ||
| Doxycycline | Travel to chloroquine- or mefloquine-resistant areas; >8 yr of age only. Beware photosensitivity | 2 mg/kg/day up to 100 mg/day 1-2 days preexposure and for 4 wk after exposure |
| Pyrimethamine–sulfadoxine (Fansidar) | Standby for treatment if malarial symptoms develop and medical attention >24 hr away Contraindicated if age <2 mo or sulfa allergy |
Single dose: |
2 mo-1 yr:  tab tab |
||
1-3 yr:  tab tab |
||
| 4-8 yr: 1 tab | ||
| 9-14 yr: 2 tabs | ||
| >14 yr: 3 tabs | ||
| Primaquine | Prevention of relapse with P. vivax or P. ovale Use after prolonged stay in malaria-endemic area Avoid if G-6-PD deficient |
0.6 mg/kg/day for 14 days |
G-6-PD, Glucose-6-phosphate dehydrogenase; q, every; qd, every day.
Data from Centers for Disease Control and Prevention: Information for health care providers: Prescription drugs for malaria. http://wwwnc.cdc.gov/travel/yellowbook/2010/chapter-2/malaria.aspx#990.
If a child is traveling to a chloroquine-sensitive area, such as the Caribbean, parts of Central America, or the Middle East, then chloroquine (Aralen) is the drug of choice. Chloroquine prophylaxis should be given weekly, starting 1 week before travel and continued for 4 weeks thereafter. Chloroquine passes through breast milk, but not in sufficient quantities to protect an infant. Therefore, a breastfed infant should receive chloroquine prophylaxis in standard recommended doses (see Table 99-9). Chloroquine is not readily available in a liquid form in the United States. The powder, which is extremely bitter, may be suspended in a syrup or mixed with food. Instant pudding effectively masks the bitter taste and makes the medicine more palatable. An acceptable-tasting chloroquine liquid (Nivaquine) is available outside the United States. Chloroquine should be kept out of the reach of children. As little as 300 mg may be fatal in small children.55 If a toxic chloroquine ingestion occurs, the child should be transported promptly to a medical facility.
For children traveling to chloroquine-resistant areas, the next question is whether they are traveling to a mefloquine-resistant area as well. This includes parts of Myanmar (Burma), Cambodia, and Thailand. If the area is mefloquine sensitive, then mefloquine (Lariam) is a good option. The advantage of mefloquine is that it is dosed weekly, from 1 to 2 weeks before travel until 4 weeks after return. It should be avoided in children under 5 kg (11 lb) and those with psychiatric illnesses, epilepsy, or underlying cardiac arrhythmias. If the area is mefloquine resistant (or mefloquine sensitive, but either contraindications to mefloquine exist or parents prefer not to use mefloquine), then the two options are atovaquone plus proguanil (Malarone) or doxycyline. Malarone is approved in the United States for children more than 5 kg (11 lb) in weight, but requires daily administration. It must be taken 2 days before entry into a malarial area and continued for 7 days after leaving. It is contraindicated in the setting of severe renal impairment (creatinine clearance, <30 mL/min). Both Malarone and mefloquine are available in tablet form only, but tablets may be administered crushed. Alternatively, a compounding pharmacist may prepare the child’s dose in a gelatin capsule and the contents of the capsule can be placed in food just prior to administration. Doxycycline is indicated for children older than age 8 years traveling to mefloquine-resistant areas or with contraindications to mefloquine or Malarone use. It also must be dosed daily. It should be started 1 to 2 days before and continued for 4 weeks after travel to a malarial area. Side effects include diarrhea and photosensitivity. With all antimalarials, particularly those dosed daily, timing of medication ingestion is critical. Medications should be taken at the same time each day/week, to avoid a drop in blood levels below the level of efficacy. Given the difficulties in administering medications to children, weekly dosing (mefloquine) may be preferable when it is an option. The importance of proper prophylaxis against malaria cannot be overemphasized. In a review of pediatric malaria cases, 75% to 100% of patients had received no or inadequate chemoprophylaxis.18,58
In the event that a child develops an acute febrile illness in a malaria-endemic area where medical care is not immediately available, pyrimethamine-sulfadoxine (Fansidar) may be used as standby treatment. Fansidar is given as a one-time dose. Prophylaxis with this drug is not recommended because of the risk of Stevens–Johnson syndrome. Fansidar should not be given to an infant younger than age 2 months or to anyone allergic to sulfa medications. Malarone is an alternative standby treatment that has been used successfully in Fansidar-resistant areas (parts of Southeast Asia and the Amazon basin).7 All patients who take Fansidar or Malarone for presumptive treatment of malaria should be transported to a medical facility as soon as possible for definitive care. Of note, artemisinin-derived agents are not available in the United States except under special circumstances for severe malaria in hospitalized patients. They are not used for prophylaxis because the short half-lives of these agents would require multiple daily doses.
Travel-Related Problems
Next to boredom and restlessness, motion sickness and eustachian tube dysfunction are the most common problems encountered by children during travel. Parents can minimize the first two problems by preparing small activity packs or bags with paper, pencils, crayons, stickers, cards, travel puzzles, or small toys. Once at their destination, children most frequently suffer from diarrhea, fevers, rashes, and respiratory tract infections.33 Parents should be aware of the basic elements of diagnosis, treatment, and reasons to seek immediate medical attention.
Motion Sickness
Motion sickness can occur with air, land, or sea travel (see Chapter 83), particularly in children ages 2 through 12 years. Emotional upset, noxious odors, and ear infections can make symptoms worse. Children experiencing motion sickness are often pale and diaphoretic, and they feel nauseated and weak. They may vomit, but unfortunately this does not provide prolonged relief. Children known to be susceptible to motion sickness should be seated in the middle or near the front of the boat, plane, or car, where motion is minimized. They should be encouraged to look at objects far away and avoid focusing on close objects such as books. Some children get significant relief from using headphones to listen to music or stories.
Eustachian Tube Dysfunction
Eustachian tube dysfunction is the result of disequilibrium between pressure in the eustachian tube and the surrounding atmospheric pressure. If atmospheric pressure rises (e.g., with descent in an airplane) and the pressure within the tube does not rise as quickly as the ambient pressure, the eustachian tube becomes compressed. If compressed enough, the eustachian tube cannot equalize pressure in the middle ear with that of the environment, resulting in a sense of compression on the outer aspect of the tympanic membrane. Far more children than adults (nearly 15% of the pediatric population) suffer from this problem, because of the relatively smaller, and hence more compressible, pediatric eustachian tube. Swallowing often helps relieve the pressure disequilibrium and may be facilitated by drinking, sucking on a pacifier, or, for the breastfed infant, by nursing. Older children may wish to chew gum or yawn to equalize middle ear and atmospheric pressure. Contrary to popular belief, decongestants are not useful with eustachian tube dysfunction in children and should generally be avoided in young children.9
Traveler’s Diarrhea
Traveling to wilderness areas or developing countries requires leaving behind modern sanitation and reliably disinfected tap water. Unfortunately, this places travelers at increased risk for diarrheal illness (see Chapter 68). Up to 60% of children younger than age 3 years develop prolonged diarrhea (>10 days) during travel in tropical or subtropical areas.2,11 This risk is highest in young visitors to Africa and India, followed by travelers to Asia and Latin America. Young children are at greater risk for traveler’s diarrhea (TD) and its complications because of their relatively poor hygiene, oral exploration, immature immune systems, lower gastric pH, more rapid gastric emptying, and difficulties with adequate hydration.
TD is defined by the National Institutes of Health (NIH) as a twofold or greater increase in the frequency of unformed stools, or any number of such stools when accompanied by symptoms of fever, abdominal cramping, vomiting, or blood or mucus in the stools. In small children, the course tends to be more severe and prolonged, lasting from 3 days to 3 weeks.2 The majority (>80%) of TD is caused by bacteria, followed by parasites (10%) and viruses (5% to 8%) (Table 99-10). Enterotoxigenic Escherichia coli alone is responsible for 50% of TD.40 Shigella and Campylobacter are also prominent causes of TD, along with rotavirus and norovirus. Giardia is by far the most common parasitic cause of TD and is more indolent in onset.
| Agent | Examples |
|---|---|
| Preformed toxin | Enterotoxigenic Escherichia coli* |
| Staphylococcus aureus | |
| Bacillus cereus | |
| Viral | Rotavirus* |
| Norovirus* | |
| Adenovirus | |
| Enterovirus | |
| Influenza | |
| Hepatitis | |
| Bacterial | Shigella* |
| Campylobacter* | |
| Salmonella | |
| Enteroinvasive Escherichia coli | |
| Yersinia enterocolitica | |
| Vibrio cholerae | |
| Parasitic | Giardia lamblia |
| Entamoeba histolytica | |
| Cryptosporidium |
Prevention
Standard recommendations for prevention of TD are based primarily on known potential vehicles for transmission the illness (see Box 99-4). Transmission is through fecal–oral contamination, with water, food, and fingers as the most common vehicles. Careful selection and preparation of food and beverages can decrease the risk of acquiring TD. As mentioned previously, washing hands thoroughly before eating decreases bacterial carriage and also serves as a reminder to children of the need for precautions. If soap is unavailable, gross particles can be rinsed off with water and the hands then cleansed with an alcohol-based hand sanitizer. The “boil it, cook it, peel it, or forget it” rule implies that all raw vegetables and salads should be avoided, meats and seafood should be well cooked, and fruits need to be properly peeled. See Chapter 67 for a complete discussion of water disinfection.
The use of antibiotics to prevent TD in children is not currently recommended by the CDC or the American Academy of Pediatrics (AAP) because of the risks of medication side effects and development of antibiotic resistance.2 Bismuth subsalicylate (Pepto-Bismol) has been shown in adults to be an effective form of chemoprophylaxis against TD. The few small studies in children have demonstrated modest, if any, efficacy.12 Therefore, and because of the risk of administering salicylates to children, the use of bismuth subsalicylate for TD prevention in children, particularly those younger than age 3 years, is not recommended. Probiotic agents, such as Lactobacillus acidophilus, have been studied and shown to be effective for both prevention and treatment of TD in children.10,23,31 Their mechanism of action is not entirely clear, but most likely involves competition with pathogens for intestinal receptors, improvement of immune function in the gut, or production of antibiotics by the probiotic agent with efficacy against pathogens.31 Lactobacillus is available over the counter; dosing is one tablet or capsule a day for children younger than age 2 years, and two a day for children older than 2 years. Capsules can be opened and placed into food or drink for children unable or unwilling to take pills.
Treatment
The major cause of morbidity and mortality in infants and small children with diarrhea is dehydration.60 Signs of dehydration in children are listed in Box 99-5. According to the WHO, dehydration is best categorized as mild to moderate, or severe. This distinction is based on changes in behavior and mental state, quality of mucous membranes, oliguria or anuria, changes in vital signs, and decreasing peripheral perfusion. Parental assessment of dehydration using urine output, tearing, and fontanelle contour has been shown to be accurate.60 Children young enough to be wearing diapers should have some urine output at least every 8 hours. If they do not, they are very likely dehydrated.
The cornerstone of treatment for TD is oral rehydration therapy (ORT), which, if instituted early, can be used alone in 90% to 95% of cases.3 It is as effective as intravenous hydration in mild to moderate dehydration caused by gastroenteritis. ORT is often tolerated by children who are vomiting if administered frequently in small quantities. Parents traveling to developing countries or wilderness areas with children should carry powdered oral rehydration solution (ORS) or a recipe for a homemade solution (Box 99-6). Powdered ORS is readily available in most developing countries in pharmacies and drug stores. Most available ORS is glucose based. In the past, standard WHO ORS was not particularly effective in reducing stool frequency and volume. By reducing the osmolarity of ORS, stool volumes in young children with noncholera diarrhea have decreased by roughly one-third.3,34 Many studies have looked at the efficacy of rice-based ORS relative to WHO standard and reduced-osmolarity ORS. Rice-based ORS is less expensive and often better tolerated by children, particularly those in heavy rice-consuming nations. Rice-based ORS (e.g., Ceralyte: http://www.ceraproductsinc.com) has slightly lower osmolarity and higher concentration of organic solutes, which promote enhanced absorption of Na+ and water.30 Although rice-based ORS appears superior to standard WHO ORS in several studies, there have not been studies with sufficient power to demonstrate any difference in efficacy relative to the reduced-osmolarity ORS. Therefore, either rice-based ORS or reduced osmolarity WHO ORS can be used. All ORS should be discarded 12 hours after reconstitution when left at room temperature, and after 24 hours with refrigeration.
BOX 99-6
Homemade Oral Rehydration Solutions (ORS)
Data from http://www.rehydrate.org.
For rapid treatment of mild–moderate dehydration, 50 to 100 mL/kg of ORS should be administered over the first 4-hour period to rehydrate the child. An additional 10 mL/kg can be given for each diarrheal stool and 5 mL/kg for each episode of emesis. If vomiting develops, most children will tolerate ORS if given in small volumes (5 to 10 mL) every 5 minutes. Reduced-osmolarity ORS contains 75 mEq/L of sodium, 1.5% glucose, and 20 mEq/L of potassium (Table 99-11). If a solution with more glucose is used, the osmotic pressure exerted by the carbohydrate in the intestinal lumen produces fluid losses greater than fluid absorption, thereby exacerbating diarrhea. Most colas, sports drinks, and juices contain 6% to 15% carbohydrate and are not appropriate rehydration solutions. Once the child is rehydrated, regular liquids can be resumed. Feeding of solid food, particularly complex carbohydrates and yogurt, should be resumed as soon as vomiting resolves. Solid food promotes enterocyte regeneration and reduces duration of diarrhea.2,60 Foods with high concentrations of simple sugars (e.g., juice) can exacerbate diarrhea because of their high osmotic load, and fatty foods can cause vomiting because of prolonged gastric emptying. Both should be avoided in the recovery phase.
Although oral hydration is the cornerstone of therapy for TD, medications may occasionally be helpful. Children with large volumes of diarrhea can develop zinc deficiency. Zinc is important not only for cellular immunity but also for maintenance of gut mucosal cells. Zinc deficiency can lead to a vicious cycle of increasing duration and severity of diarrhea. Presently, the WHO recommends zinc supplementation (20 mg/day for 10 to 14 days for children ≥6 months of age and 10 mg/day for children <6 months of age) with ORS in children in the developing world with acute diarrheal illness.38 It is not yet clear whether children from the developed world with TD would derive benefit from zinc.
The American Academy of Pediatrics does not support the use of antimotility agents in children because of concern for ileus and decreased mental status. A recent Cochrane Database review demonstrated a modest benefit of loperamide in children, reducing duration of diarrhea and stool frequency.37 However, children under 3 years and those who appear ill or have bloody diarrhea can develop complications from agents that slow down gut motility. Antimotility agents should be avoided in this group. Other antidiarrheal agents, such as bismuth subsalicylate or attapulgite, have not been convincingly shown to be effective in children and should be avoided, particularly in those younger than age 2 years.2,12,32
Empiric treatment with antibiotics for TD is safe and effective in reducing TD severity and duration in adults but is not currently recommended by the AAP for use in children.2 That being said, antibiotics can reduce the duration of TD in children and reduce the likelihood or severity of diaper dermatitis in non–toilet-trained infants/toddlers. This underappreciated consequence of severe diarrhea is extremely uncomfortable and puts the child at risk for bacterial superinfection of abraded perianal skin. As a result, travel medicine specialists frequently recommend the use of antibiotics in children who develop diarrhea in countries with high rates of TD.40 Antibiotics are generally recommended in children with fever, bloody stool, or abdominal distention in whom invasive bacterial diarrhea is suspected. Caution is advised if shiga-toxin producing E coli is suspected as antibiotics can increase the risk of hemolytic uremic syndrome (HUS). Under age 3 to 6 months, the risk of bacteremia with Salmonella infections is significant and antibiotic treatment is indicated. With increasing bacterial resistance to trimethoprim–sulfamethoxazole, azithromycin is now the drug of choice for treatment of bacterial diarrhea.2,60 The dosage is 10 mg/kg/day up to 500 mg a day for 3 days. Fluoroquinolones, such as ciprofloxacin, are an alternative but are approved in the United States only for children older than age 18 years. Multiple studies have, however, demonstrated safety and efficacy in children as young as age 6 months, but increasing bacterial resistance to quinolones, particularly in Southeast Asia, makes azithromycin a better choice.14,29 Severe dehydration, high fever, failure of ORT, failure of antibiotic therapy for bloody diarrhea, or altered mental status require prompt medical attention and administration of intravenous fluids for rehydration (Box 99-7). Typhoid fever caused by Salmonella typhi should be managed initially in a hospital setting with a quinolone, such as ciprofloxacin, or a third-generation cephalosporin, such as ceftriaxone, depending on regional resistance patterns.39
Constipation
Respiratory Infections and Otitis Media
Respiratory tract and otolaryngologic infections are very common in the pediatric population. The majority of infections, including acute otitis media (AOM), sinusitis, pharyngitis, croup, bronchiolitis, and bronchitis, involve the upper respiratory tract. Most of these are viral in etiology; the remainder are the result of infections with Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis.53 Because definitive diagnoses based on otoscopy and auscultation of the lungs often cannot be made in the course of wilderness travel, parents must rely on symptoms and the presence of fever to determine whether treatment is necessary. The presence of high fever, otalgia >2 days, facial pain, sore throat without cough or rhinorrhea, or mucopurulent nasal discharge lasting longer than 10 days probably merits both antimicrobial and symptomatic treatment. It should be noted, however, that 20% to 80% of AOM and 50% of streptococcal pharyngitis cases resolve without intervention.17 Furthermore, antibiotic treatment of upper respiratory tract infections, such as bronchitis, bronchiolitis, croup, and most pharyngitis, does not shorten the course, minimize symptoms, or decrease complications.53 If streptococcal pharyngitis is suspected on the basis of absence of cough or coryza and the presence of fever, cervical lymphadenopathy, and tonsillar exudate, then antibiotic therapy is warranted. Although antibiotics for streptococcal pharyngitis have minimal effect on the duration of the disease, they reduce the incidence of suppurative complications, such as peritonsillar abscess, and nonsuppurative complications, such as rheumatic fever and post-streptococcal glomerulonephritis.
With increasing use of antibiotics, bacterial resistance to these agents has risen dramatically. Resistance is highly correlated with the rate of antibiotic use in a given population. Ten percent to 50% of S. pneumoniae isolates are resistant to penicillin, and 5% to 35% are resistant to macrolides such as erythromycin.35 Up to 20% of H. influenzae and 70% of M. catarrhalis isolates are resistant to amoxicillin. However, minimal inhibitory concentration (MIC) testing has demonstrated sensitivity to high-dose amoxicillin, even among resistant strains. First-line therapy for suspected bacterial respiratory infection is, therefore, high-dose amoxicillin at 80 mg/kg/day divided into three doses per day. Second-line therapy is high-dose amoxicillin–clavulanate (80 mg/kg/day divided into two doses per day), cefuroxime (15 mg/kg twice a day), or ceftriaxone (50 mg/kg once daily). Uncomplicated AOM in children older than 2 years may be treated for 5 to 7 days; otherwise, the standard treatment for AOM is 10 days, and for sinusitis 14 days.53 Suspected streptococcal pharyngitis can be treated for 10 days with penicillin or amoxicillin, or for 5 days with azithromycin (10 mg/kg on day 1, then 5 mg/kg/day on days 2 to 5).
If influenza is suspected based on season, regional epidemics, and symptomatology (e.g., high fever, respiratory symptoms), parents should consider carrying and administering oseltamivir (3 mg/kg/dose twice daily) to high-risk children. High-risk children are those younger than age 5 years (particularly under 2 years), those with chronic lung or other organ dysfunction, those who are immunocompromised (e.g., HIV, diabetes), and those on chronic aspirin therapy.49 Treatment is most effective in reducing length and severity of disease if given within the first 48 hours of illness. Any child with suspected influenza who appears ill or has signs of lower respiratory tract infection should immediately be given oseltamivir and taken to the nearest medical facility.
Fever of Unclear Etiology
High fever that develops in a child during the course of foreign travel may be the result of a common infection (e.g., viral syndrome, pharyngitis) or the manifestation of a tropical disease. Box 99-8 lists the indications for prompt medical attention in a child with fever. If malaria is suspected, the child should immediately be taken to the closest medical facility. If this cannot occur within 24 hours, any child older than 2 months should be given Fansidar as standby treatment as recommended in Table 99-9.
BOX 99-8 Indications for Seeking Immediate Medical Attention for Children with Fever
Typhoid fever caused by S. typhi can also manifest with high fever, paradoxical bradycardia, and, at least initially, without diarrhea. Children who appear ill with high fevers may have invasive typhoidal disease and should be treated in a medical facility. Salmonella resistance is rising in developing countries, but strains are typically susceptible to third-generation cephalosporins (e.g., ceftriaxone) and/or quinolones.39
Dengue fever, caused by a mosquito-borne arbovirus, can also cause high fever, headaches, and severe myalgias. With the exception of recurrent dengue, which can result in hemorrhagic complications, the treatment of dengue fever is purely symptomatic. Of note, dengue is a disease found not only in the developing world. The southeastern United States and Hawaii are infested with the dengue-carrying Aedes aegypti mosquito.59
Headache
A child with a tender tooth or tenderness to palpation of his sinuses should be managed with analgesics (e.g., acetaminophen with or without codeine or ibuprofen) and antibiotics. Dental infections respond well to penicillin and a visit to the dentist for definitive management. (See Respiratory Infections and Otitis Media, earlier, for information on the antibiotic treatment of sinus infections.) If a child has had previous migraine headaches or has a history that is classic for migraine (e.g., unilateral headache, aura, visual scotoma, photophobia, nausea, family history of migraine), analgesics and rest in a quiet, dark room are the appropriate first-line therapies. Caffeine, in the form of a strong cup of coffee, is also a helpful improvisational treatment for migraine headaches. If a child’s headache is accompanied by high fever, neck stiffness, vomiting, confusion, neurologic abnormalities, or a recent history of trauma, the child should be brought to medical attention immediately.
Rashes
Identification of rashes in children is an art. Although parents cannot be expected to become familiar with all types of rashes, they may be able to distinguish common rashes from potentially dangerous exanthems. Petechial, purpuric, or mucosal lesions are markers for potentially serious diseases and should prompt parents to seek medical attention immediately. Standard dermatology textbooks with photographs can be used to instruct parents to recognize common viral exanthems and rashes caused by varicella, scabies, and contact dermatitis (e.g., poison oak or poison ivy). Scabies can most safely be abolished with permethrin. Contact dermatitis often can be simply treated with 1% hydrocortisone cream and diphenhydramine (see Chapter 63). When dermatitis covers the face, genitals, or large portions of the child’s skin, systemic corticosteroids may be indicated.
Animal Bites
Bites from stray dogs and other animals are more frequent during travel to the developing world. Prevention techniques primarily involve keeping children away from stray dogs and other wild animals and a strict “no feeding of animals” rule. If a bite occurs, it should be irrigated copiously. In general, lacerations from animal bites should not be repaired primarily, with the exception of certain facial wounds. All victims of animal bites should receive antibiotic prophylaxis, ideally with amoxicillin–clavulanate (80 mg/kg/day divided twice daily) or azithromycin (10 mg/kg on day 1, then 5 mg/kg/day daily for 5 days) in persons who are penicillin allergic.61
Rabies is endemic in many parts of the world, including much of South and Central America, India, Southeast Asia, and the Phillipines.13 Unlike in the United States, where bats and raccoons are the most common carriers, in the developing world, domesticated animals, such as dogs and cats, are most frequently implicated in transmission. All animal bites that occur in rabies-endemic areas, no matter how superficial, mandate postexposure rabies prophylaxis (see Table 99-7 for schedule of vaccination). In fact, any contact between a child and a raccoon, bat, fox, or skunk in an endemic area should be treated as a high-risk event and treated with rabies vaccination.61 Current CDC guidelines recommend that children traveling to endemic areas for more than a month or those who will be spending a great deal of time outdoors should receive rabies prophylaxis prior to their travels.64 If a bite occurs in a child who has been previously vaccinated, then the remaining two doses of the vaccination series should be given. If a bite occurs in a child with no preexposure vaccination, that child should begin the rabies vaccination series and receive rabies immunoglobulin (HRIG: 20 IU/kg with as much as possible in and around the wound and the remainder IM in a large muscle).
Special Considerations for Children with Chronic Medical Problems
Asthma
Parents of children with asthma face unique challenges when traveling into the wilderness or to the developing world. In both situations, access to medical care may be limited and parents may need to treat exacerbations that would normally require advanced medical attention. In addition, exposure to known asthma triggers, such as tobacco and specific allergens, may not be as controllable while traveling. A study of adult adventure travelers demonstrated that the major risk factors for asthma exacerbations while traveling include poorly controlled asthma prior to departure and intensive physical exertion.26
Sickle Cell Disease
Fever is a common and significant problem for children with sickle cell disease. By the age of 1 year, children with this disease are effectively asplenic as a result of sickling-related infarction of the spleen. As a consequence, infections with encapsulated organisms normally cleared by the spleen can rapidly lead to sepsis. Vaccinations against Haemophilus influenzae, Streptococcus pneumoniae, and Neisseria meningitidis (MCV4) are the first line of defense. In addition, the American Academy of Pediatrics recommends penicillin prophylaxis (125 mg twice a day) for sickle cell patients under the age of 5 years to effect a significant (85%) reduction in pneumococcal bacteremia.24 Children with sickle cell disease who develop fever should receive prompt medical attention. If this is not immediately available, they should be treated with an antibiotic, such as amoxicillin–clavulanate (80 mg/kg/day divided twice daily). Children under the age of 5 years are at particularly high risk for sepsis.
Infants and Neonates
Box 99-9 outlines the indications for immediate medical evaluation of young infants. As mentioned previously, parents are strongly advised against traveling to the developing world with children under the age of two. Immature immune systems, incomplete vaccination status, contraindications to prophylactic medications and travel vaccines, and frequent hand-to-mouth contact make infants and very young children extremely susceptible to disease. Only essential travel should be undertaken.
Pediatric Wilderness Medical Kits
When a family travels in remote areas, the medical kit must be adapted to meet the special needs of the children. Items carried vary depending on the ages of the children, preexisting medical conditions, length of travel, specific environmental conditions likely to be encountered, and medical sophistication of the adults. Although there is considerable room for individual preference in assembling a medical kit, certain items are essential for management of problems commonly encountered during wilderness travel with children (Box 99-10).
BOX 99-10 Pediatric Wilderness Medical Kit
Basic Supplies
To reduce weight and bulk, medications selected for a wilderness medical kit should have multiple uses (see Table 99-12). For example, diphenhydramine is effective for allergic symptoms, pruritus, motion sickness, nausea, and insomnia. Desitin, best known for its use in preventing diaper rash, is an excellent sun block, as it contains 40% zinc oxide. A broad-spectrum antifungal cream, such as miconazole or clotrimazole, covers not only tineal infections (ringworm, jock itch, and athlete’s foot) but also Candida infections (diaper rash and vaginitis). Medications in liquid form should generally be avoided because they add excess weight to the medical kit and can leak. If an infant under the age of 6 months is traveling, liquid medications can be carried in light- and leak-proof powder form. Most children are able to chew tablets once their first molars are present (by about 15 months). Before that time, chewable medications or tablets can be crushed between two spoons and mixed with food. If a child dislikes the taste of medication, it may be camouflaged in a food such as instant pudding, which is easily carried in powdered form.
TABLE 99-12 Pediatric Medications in the Wilderness Medical Kit
| Medication | Indication | Dose |
|---|---|---|
| Topical Medications | ||
| Antibiotic ointment (e.g., bacitracin or polymyxin) | Superficial skin infections | Apply as directed qd to tid |
| Topical corticosteroid (e.g., 1% hydrocortisone) | Contact or atopic dermatitis, insect bites, sunburn | Apply to affected areas bid to tid (use sunscreen aggressively; avoid >1% corticosteroid on face) |
| Antifungal cream (e.g., clotrimazole or miconazole) | Yeast at diaper area, groin, scalp, feet; ringworm | Apply bid for 7-10 days and for several days after rash has resolved |
| Desitin cream | Sun block, diaper-area erythema | Apply thick coat as sunscreen or thin coat for diaper area |
| Permethrin (Elimite) | Scabies, lice, treatment for clothing and mosquito netting | Apply 5% cream from chin to soles of feet and wash after 8-14 hr, do not use in children <2 mo of age or on eyes, nose, mouth |
| Anesthetic eye drops (e.g., proparacaine)*,† | Removal of superficial ocular foreign body | 1 drop in affected eye for removal of foreign body, must patch eye for protection for at least 1 hr |
| Antibiotic eye ointment (e.g., erythromycin)† or drops (e.g., polymyxin B sulfate plus trimethoprim [Polytrim])† | Purulent conjunctivitis, suspected corneal abrasion | Ointment: thin line upper lid margin tid to qid |
| Drops: 1 drop every 3 hr for 7 days | ||
| Antipyrine–benzocaine otic drops | Ear pain (otitis externa or media); avoid if <3 mo or TM rupture suspected | 3-4 drops in affected ear every 2-3 hr as needed to relieve pain |
| Oral Medications | ||
| Diphenhydramine | Allergy symptoms, pruritus, insomnia, nausea, motion sickness | 1.25 mg/kg/dose every 6 hr (up to 25-50 mg/dose), may cause paradoxic restlessness in children |
| 12.5 mg/5 mL elixir | ||
| 25- or 50-mg capsules | ||
| Acetaminophen | Fever control, pain | 15-20 mg/kg every 4-6 hr up to 650 mg/dose |
| 80 mg/0.8 mL drops | ||
| 160 mg/5 mL elixir | ||
| 80- and 160-mg | ||
| chewable tabs | ||
| Ibuprofen | Fever control, pain, antiinflammatory | 10 mg/kg/dose every 8 hr up to 600 mg/dose |
| 40 mg/1 mL drops | ||
| 100 mg/5 mL elixir | ||
| 50- or 100-mg chewable tabs | ||
| 100- or 200-mg caplets | ||
| Acetaminophen with codeine† | Severe pain, severe cough | As for acetaminophen, or 0.5-1.0 mg/kg of codeine every 4-6 hr |
| 120 mg acetaminophen with 12 mg of codeine/5 mL elixir | ||
| Dimenhydrinate (Dramamine) | Motion sickness | 1-1.5 mg/kg/dose 1 hr prior to departure and every 6 hr thereafter; may cause drowsiness |
| 12.5 mg/5 mL elixir | ||
| 50-mg chewable tabs | ||
| Oral Antibiotics (as appropriate for age of child) | ||
| Amoxicillin† | AOM, sinusitis, pharyngitis, pneumonia | 80 mg/kg/day for UTI or pneumonia, in divided dose TID |
| 125- or 250-mg chewable tabs | ||
| 250-mg capsule | ||
| Amoxicillin–clavulanate (Augmentin)† | Penicillin-resistant organisms, AOM, sinusitis, animal bites | 80 mg/kg/day in divided dose BID |
| 200- and 400-mg chewable tabs | ||
| 200 and 400 mg/5 mL elixir | ||
| Azithromycin (Zithromax)† | AOM, sinusitis, pharyngitis, pneumonia, traveler’s diarrhea, skin infections, animal bites | 10 mg/kg on day 1, then 5 mg/kg/day × 4 days |
| 125 and 250 mg/5 mL elixir | ||
| 250-mg tabs (best) | ||
| Ciprofloxacin (Cipro)† | In the United States, approved for >18 yr of age only: UTI, traveler’s diarrhea, wounds acquired in an aquatic environment | 20-30 mg/kg/day in divided dose BID up to 500 mg BID |
| 100, 200, 500 mg tabs | ||
| Trimethoprim–sulfamethoxazole (Septra) | Suspected MRSA skin infection 80/400 SS tab; 160/800 DS tab | 8-10 mg TMP/kg/d in divided dose BID |
| >2 mo old | ||
| Oseltamivir (Tamiflu) | Influenza treatment (12 mg/mL susp 30, 45, 75 mg caps) | Not recommended <3 mo old; Tx × 5 days |
| 3-12 mo: 3 mg/kg/dose twice daily | ||
| >12 mo: <15 kg (33 lb): 30 mg BID; | ||
| 15-23 kg (33-51 lb): 45 mg BID; | ||
| 24-40 kg (53-88 lb): 60 mg BID; | ||
| >40 kg (>88 lb): 75 mg BID | ||
| Other Preparations | ||
| Epinephrine (premeasured)† | Anaphylaxis, severe asthma | 0.15 mg SC up to 15 kg (33 lb); 0.3 mg SC if >15 kg (>33 lb) |
| 0.15 mg EpiPen Jr or Twinject 0.15 mg | ||
| 0.3 mg EpiPen or Twinject 0.3 mg | ||
| Oral rehydration packet (ORS) | Dehydration | See Table 99-11 for administration guidelines |
| Foreign Travel | ||
| Loperamide | Nonbloody diarrhea, minimally febrile, significant diarrhea older than age 2 yr | 13-20 kg (29-44 lb): 1 mg TID; |
| 1 mg/5 mL | 20-30 kg (44-66 lb): 2 mg BID; | |
| 1 mg caps | >30 kg (>66 lb): 2 mg TID; | |
| Appropriate malaria prophylaxis | — | See Table 99-9 if indicated† |
| Pyrimethamine–sulfadoxine (Fansidar)† | Standby treatment for malaria if immediate medical attention unavailable | See Table 99-9 |
| Travel to High Altitude | ||
| Acetazolamide (Diamox)† | Recurrent AMS despite graded ascent | 5 mg/kg/day divided BID up to 250 mg/day |
| 30 or 50 mg/mL suspension | ||
| 125-mg tab | ||
| Zofran ODT | Nausea and vomiting associated with AMS | 6 mo-1 yr: 1 mg |
| 4-mg tab | 1-4 yr: 2 mg | |
| >4 yr: 4 mg | ||
AMS, Acute mountain sickness; AOM, acute otitis media; BID, twice a day; qd, every day; SC, subcutaneous; TID, three times a day; UTI, urinary tract infection.
* Administration of this medication by other than trained medical personnel is strongly discouraged, given the risk of overuse and subsequent worsening of eye injury; if significant eye irritation persists, medical attention must be sought to evaluate for corneal injury.
† Available by prescription only.
Two or three antibiotics will cover most bacterial infections encountered in children. Age of children traveling, allergies, intolerance, chronic medical conditions, disease prevalence/epidemics at the destination, and past experience must be taken into account when antibiotics are selected. Given increasing bacterial resistance to common antibiotics, antimicrobial choices should be reevaluated periodically to ensure that infections likely to be encountered can be successfully treated with these agents. All oral antibiotics require a prescription. Amoxicillin is available in pleasant-tasting chewable tablets (125 and 250 mg) and in powdered form for suspension (125 and 250 mg/5 mL). Because of current resistant patterns, high-dose therapy with 80 mg/kg in divided doses, two to three times daily, is indicated. Amoxicillin is familiar to and well tolerated by most children. Amoxicillin–clavulanate provides excellent coverage when a penicillin-resistant organism is suspected for recurrent pharyngitis, soft tissue infections, animal bites, and infections. The most common side effect is diarrhea, but this has been reduced with the newer formulations. The new formulation is available in 200- and 400-mg (amoxicillin component) chewable tabs and in 200 and 400 mg/5 mL liquid. Dosing is 80 mg/kg (amoxicillin component) in divided doses twice a day. Azithromycin (Zithromax) is a long-acting macrolide without the gastrointestinal side effects of erythromycin. It is effective in the treatment of otitis media, sinusitis, pharyngitis, lower respiratory tract infections, TD, and common animal bites. It is particularly useful in children with penicillin allergies. Dosing is extremely convenient because of azithromycin’s long half-life; a 10 mg/kg dose on day 1 is followed by 5 mg/kg/day for a total of 5 days. Ciprofloxacin has broad-spectrum coverage and is useful for treatment of bacterial diarrhea, complex urinary tract infections, and wounds acquired in an aquatic environment. Its use has not been approved for children younger than age 18 years in the United States because of a potential problem with arthropathic effects on weight-bearing joints. However, a study involving more than 600 children found only a 1.3% rate of reversible arthralgia and no evidence of arthropathy.29 Nonetheless, ciprofloxacin should not routinely be recommended for children unless a special situation arises in which the benefits of its use outweigh the risks (e.g., complex pyelonephritis, typhoid fever). Trimethoprim–sulfamethoxazole (Septra) is a sulfa antibiotic useful against skin infections where MRSA is a concern. In many areas, the presence of MRSA in infected wounds and cellulitis is so high that the recommendation is to always use an agent with bactericidal activity against MRSA. The dosing is 8 to 10 mg of the TMP component/kg/day in divided doses twice daily. Finally, for children younger than age 5 years, those with chronic medical conditions or those on chronic aspirin therapy who will be traveling in areas with influenza activity, parents should consider including oseltamivir (Tamiflu) in their medical kit.49 It is available in suspension or capsule form. The dosing is roughly 3 mg/kg/day in two divided doses daily.
Parents of children with special medical conditions should carry a pertinent medical summary and have resources to gain access to specialty physicians in the destination countries. A generous supply of necessary medications with instructions for caregivers and consulting physicians on what is to be done should symptoms worsen should be included in the medical kit. An extra supply of all essential medications should be kept with either the parents or the patient in case the medical kit gets lost or separated from the patient when the medication is needed. Some travelers in areas endemic for hepatitis B/C and acquired immunodeficiency syndrome (AIDS) carry their own needles and syringes for emergency use. The International Association for Medical Assistance to Travelers (http://www.iamat.org) has a directory of qualified physicians worldwide who speak English.
Environmental Concerns and Child Health
Human activities have affected our global environment in dramatic ways. These changes have been driven primarily by increasing reliance on fossil fuels. Use of leaded gasoline has resulted in significant lead contamination of soil. Childhood exposure to lead can cause anemia, gastrointestinal problems, and neurologic damage. A more insidious and far-reaching problem associated with the use of fossil fuels is accumulation of carbon dioxide, methane, and nitrous oxide in the atmosphere. Accumulation of these so-called greenhouse gases has been linked to some of the warmest average air and sea temperatures ever recorded.16 These changes in temperature will likely result in extremes of precipitation, floods and drought, and more frequent catastrophic weather phenomena.
Because of their physical, physiologic, and cognitive immaturity, children are very vulnerable to adverse health effects from environmental hazards. Specifically, children are more susceptible to thermal stresses that can lead to dehydration and hyperthermia, particularly during exercise. Higher average temperatures will further increase this risk. The rates of sunburn in children and of subsequent melanoma are likely to rise. Warmer temperatures typically result in higher levels of ozone and other air pollutants. Because children tend to spend more time outdoors and have a higher minute ventilation, increased air pollution can significantly affect children with asthma and other respiratory diseases. Warmer winters and rising carbon dioxide levels may result in earlier and more abundant release of grass and other pollens, which could increase incidence and severity of atopic syndromes in children.54 Higher temperatures, along with changes in humidity and flood frequency, are likely to result in significant increases in vector- and rodent-borne disease transmission. Recent modeling experiments suggest that the distribution of malaria, a disproportionate killer of children, is likely to increase by 5% to 7% in Africa by 2100.54 The rate of dengue virus replication in A. aegypti mosquitoes increases directly with temperature. Higher global temperatures might result in a higher infection rate, particularly in children who are less able to protect themselves from mosquitoes. Tick-borne diseases may become more prevalent as flooding expands the rodent population that is an integral part of the tick life cycle. Extremes of precipitation, specifically flooding, increase the likelihood of drinking contaminated water and waterborne gastrointestinal illness. Children suffer disproportionate morbidity and mortality from AGE.
1 Alberts MB, Shalit M, LoGalbo F. Suction for venomous snakebite: A study of “mock venom” extraction in a human model. Ann Emerg Med. 2004;43:187.
2 Ang JY, Mathur A. Traveler’s diarrhea: Updates for pediatricians. Pediatr Ann. 2008;37:814.
3 Atia AN, Buchman AL. ORS in non-cholera diarrhea. Am J Gastroenterol. 2009;104:2596.
4 Baumgartner EA, Belson M, Rubin C, et al. Hypothermia and other cold-related morbidity emergency department visits: United States, 1995-2004. Wilderness Environ Med. 2008;19:233.
5 Bell JW, Veltri JC, Page BC. Human exposures to N,N-diethyl-m-toluamide insect repellents reported to the American Association of Poison Control Centers 1993-1997. Int J Toxicol. 2002;21:341.
6 Bloch J, Duplain H, Rimoldi SF, et al. Prevalence and time course of acute mountain sickness in older children and adolescents after rapid ascent to 3450 meters. Pediatrics. 2009;123:1.
7 Boggild AK, Parise ME, Lesis LS, et al. Atovaquone-proguanil: A report from the CDC expert meeting on malaria chemoprophylaxis. Am J Trop Med Hyg. 2007;76:208.
8 Bronstein AC, Spyker DA, Cantilena LRJr, et al. 2006 annual report of the American association of poison control centers’ National Poison Data System (NPDS). Clin Toxicol (Phila). 2007;45:815.
9 Buchanan BJ, Hoagland J, Fischer PR. Pseudoephedrine and air travel-associated ear pain in children. Arch Pediatr Adolesc Med. 1999;153:466.
10 Chen CC, Kong MS, Lai MW, et al. Probiotics have clinical, microbiologic, and immunologic efficacy in acute infectious diarrhea. Pediatr Infect Dis J. 2010;29:135.
11 Cheng AC, McDonald JR, Thielman NM. Infectious diarrhea in developed and developing countries. J Clin Gastroenterol. 2005;39:757.
12 Chowdhury HR, Yunus M, Zaman K, et al. The efficacy of bismuth subsalicylate in the treatment of acute diarrhoea and the prevention of persistent diarrhoea. Acta Paediatr. 2001;90:605.
13 Christenson JC. Preparing families with children traveling to developing countries. Pediatr Ann. 2008;37:806.
14 Chysky V, Hullman R, Schact P, et al. Safety of ciprofloxacin in children: Worldwide clinical experience based on compassionate use. Emphasis on joint evaluation. Infection. 1991;19:289.
15 Committee on Infections Diseases; American Academy of Pediatrics. Prevention of rotavirus disease: Updated guidelines for use of rotavirus vaccine. Pediatrics. 2009;123:1412.
16 Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change, 2007. http://www.ipcc.ch/publications_and_data/ar4/wg1/en/contents.html
17 Dowell SF, Schwartz B, Phillips WR. Appropriate use of antibiotics for URIs in children: Part I. otitis media and acute sinusitis. Am Fam Phys. 1998;58:1113.
18 Driessen GJ, Pereira RR, Brabin BJ, et al. Imported malaria in children: A national surveillance in the Netherlands and a review of European studies. Eur J Public Health. 2008;18:184.
19 Dulon M, Weichenthal M, Blettner M, et al. Sun exposure and number of nevi in 5- to 6-year-old European children. J Clin Epidemiol. 2002;55:1075.
20 Duster MC, Derlet MN. High altitude illness in children. Pediatr Ann. 2009;38:218.
21 Feder HM. Lyme disease in children. Infect Dis Clin North Am. 2008;22:315.
22 Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization: Recommendations of the advisory committee on immunization practices (ACIP). MMWR. 2006;55:1.
23 Floch MH, Walker WA, Guandalini S, et al. Recommendations for probiotic use—2008. J Clin Gastroenterol. 2008;47:234.
24 Gaston MH, Verter JI, Woods G, et al. Prophylaxis with oral penicillin in children with sickle cell anemia: A randomized trial. N Engl J Med. 1986;314:1593.
25 Godar E, Urbach F, Gasparro F, et al. UV doses of young adults. Photochemistry and Photobiology. 2003;77:453.
26 Golan Y, Onn A, Villa Y, Avidor Y, et al. Asthma in adventure travelers: A prospective study evaluating the occurrence and risk factors for acute exacerbations. Arch Intern Med. 2002;162:2421.
27 Gonzales S, Fernandez-Lorente M, Gilaberte-Calzada Y, et al. The latest on skin photoprotection. Clin Derm. 2008;26:614.
28 Goto CS, Feng SY. Crotalidae polyvalent immune Fab for the treatment of pediatric crotaline envenomation. Pediatr Emerg Care. 2009;25:273.
29 Grady R. Safety profile of quinolone antibiotics in the pediatric population. Pediatr Infect Dis J. 2003;22:1128.
30 Gregorio GV, Gonzales ML, Dans LF, et al: Polymer-based oral rehydration solution for treating acute watery diarrhoea, Cochrane Database Syst Rev 2:CD006519, 2009.
31 Guandalini S. Probiotics for children with diarrhea: An update. J Clin Gastroenterol. 2008;42:S53.
32 Guarino A, Albano F, Ashkenazi S, et al. European Society for Paediatric Gastroenterology, Hepatology and Nutrition/European Society for Paediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe. J Pediatr Gastroenterol Nutr. 2008;46:S81.
33 Hagmann S, Neugebauer R, Schwartz E, et al. Illness in children after international travel: Analysis from the GeoSentinel Surveillance Network. Pediatrics. 2010;125:e1072. Apr 5. [Epub ahead of print]
34 Hahn S, Kim S, Garner P: Reduced osmolarity oral rehydration solution for treating dehydration caused by acute diarrhoea in children, Cochrane Database Syst Rev 1:CD002847, 2002.
35 Karnezis TT, Smith A, Whittier S, et al. Antimicrobial resistance among isolates causing invasive pneumococcal disease before and after licensure of heptavalent conjugate pneumococcal vaccine. PLoS One. 2009;4:e5965.
36 Leadbetter G, Keyes LE, Maakestad KM, et al. Ginkgo biloba does—and does not—prevent acute mountain sickness. Wilderness Environ Med. 2009;20:66.
37 Li ST, Grossman DC, Cummings P. Loperamide therapy for acute diarrhea in children: Systematic review and meta-analysis. PLoS Med. 2007;4:e98. 27
38 Lukacik M, Thomas RL, Aranda JV. A meta-analysis of the effects of oral zinc in the treatment of acute and persistent diarrhea. Pediatrics. 2008;121:326.
39 Lynch MF, Blanton EM, Bulens S, et al. Typhoid fever in the United States, 1999-2006. JAMA. 2009;302:859.
40 Mackell S. Traveler’s diarrhea in the pediatric population: Etiology and impact. Clin Infect Dis. 2005;41:S549.
41 Mali S, Steele S, Slutsker L, et al. Malaria surveillance—United States, 2007. MMWR. 2009;58:1.
42 Meyer F, Bar-Or O, MacDougall D, et al. Drink composition and the electrolyte balance of children exercising in the heat. Med Sci Sport Exerc. 1995;27:882.
43 Moraga FA, Pedreros CP, Rodríguez CE. Acute mountain sickness in children and their parents after rapid ascent to 3500 m (Putre, Chile). Wilderness Environ Med. 2008;19:287.
44 Mytton J, Towner E, Brussoni M, et al. Unintentional injuries in school-aged children and adolescents: Lessons from a systematic review of cohort studies. Inj Prev. 2009;15:111.
45 National Center for Immunization and Respiratory Diseases. Use of influenza A (H1N1) 2009 monovalent vaccine: Recommendations of the advisory committee on immunization practices (ACIP). MMWR Morb Mortal Wkly Rep. 2009;58:1.
46 Newman LM, et al. Pediatric wilderness recreational deaths in western Washington State. Ann Emerg Med. 1998;32:687.
47 Osimitz TG, Murphy JV, Fell LA, et al. Adverse events associated with the use of insect repellents containing N,N-diethyl-m-toluamide (DEET). Regul Toxicol Pharmacol. 2010;56:93.
48 O’Riordan DL, Geller AC, Brooks DR, et al. Sunburn reduction through parental role modeling and sunscreen vigilance. J Pediatr. 2003;142:67.
49 Recommendations for use of antiviral medications for the management of influenza in children and adolescents for the 2009-2010 season—pediatric supplement for health care providers. http://www.cdc.gov/h1n1flu/recommendations_pediatric_supplement.htm.
50 Reported cases of Lyme disease by year, United States, 1994-2008. http://www.cdc.gov/ncidod/dvbid/lyme/ld_UpClimbLymeDis.htm.
51 Schalka S, dos Reis VM, Cuce LC. The influence of amount of sunscreen applied and its sun protection factor (SPF): Evaluation of two sunscreens including same ingredients at different concentrations. Photodermatol Photoimmunol Photomed. 2009;25:175.
52 Schumacher MJ, Tveten MS, Egen NB. Rate and quantity of delivery of venom from honeybee stings. J Allergy Clin Immunol. 1994;93:831.
53 Shah S, Sharieff GQ. Pediatric respiratory infections. Emerg Med Clin North Am. 2007;25:961.
54 Shea KM. Global climate change and children’s health. Pediatrics. 2007;120:1149.
55 Smith ER, Klein-Schwartz W. Are 1-2 dangerous? Chloroquine and hydroxychloroquine exposure in toddlers. J Emerg Med. 2005;28:437.
56 Sood SK, Salzman MB, Johnson BJB, et al. Duration of tick attachment as a predictor of the risk of Lyme disease in an area in which Lyme disease is endemic. J Infect Dis. 1997;75:996.
57 Sports participation survey. http://www.nsga.org/i4a/pages/index.cfmpageid=3482.
58 Stager K, Legros F, Krause G, et al. Imported malaria in children in industrialized countries, 1992-2002. Emerg Infect Dis. 2009;15:185.
59 Stauffer WM, Kamat D, Magill AJ. Traveling with infants and children. Part IV: Insect avoidance and malaria prevention. J Travel Med. 2003;10:225.
60 Stauffer WM, Konop RJ, Kamat D. Traveling with infants and young children. Part III: Traveler’s diarrhea. J Travel Med. 2002;9:141.
61 Talan DA, Citron DM, Abrahamian FM. Bacteriological analysis of infected dog and cat bites: Emergency medicine animal bite infection study group. N Engl J Med. 1999;340:85.
62 Thurber CA, Sigman MD. Preliminary models of risk and protective factors for childhood homesickness: Review and empirical synthesis. Child Dev. 1998;69:903.
63 Travel safely with infants and children. http://wwwnc.cdc.gov/travel/yellowbook/2010/chapter-7/traveling-with-infants-and-children.aspx.
64 Vaccine recommendations for infants and children. http://wwwnc.cdc.gov/travel/yellowbook/2010/chapter-7/vaccine-recommendations-for-infants-and-children.aspx.
65 Visscher PK, Vetter RS, Camazine S. Removing bee stings. Lancet. 1996;348:301.
66 Water-related injuries fact sheet. http://www.cdc.gov/ncipc/factsheets/drown.htm.
67 West Nile virus activity in the United States. http://www.cdc.gov/ncidod/dvbid/westnile/surv&controlCaseCount09_detailed.htm, 2009.
68 World Health Organization malaria factsheet. http://www.who.int/mediacentre/factsheets/fs094/en/index.html.

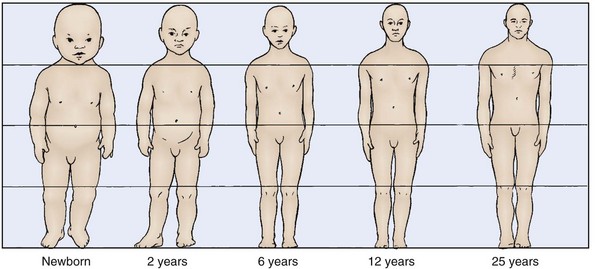

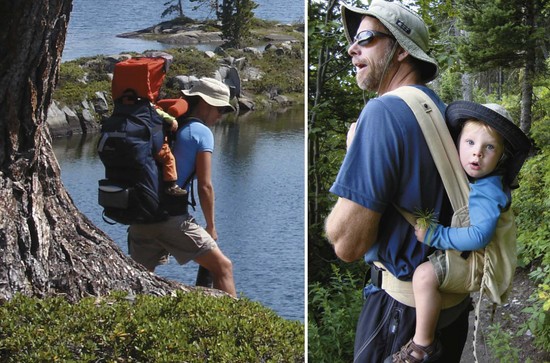

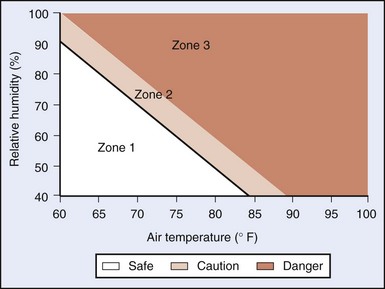


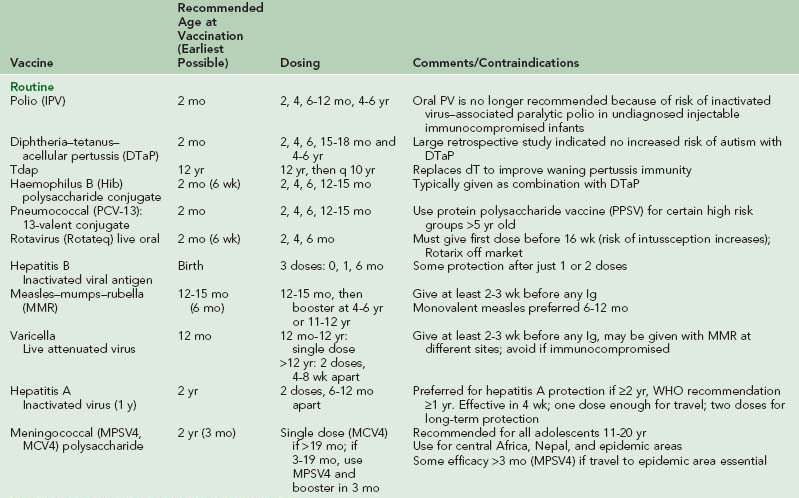
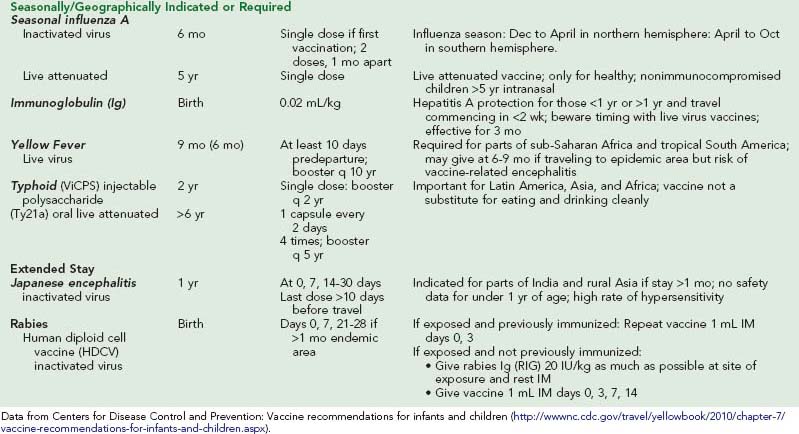
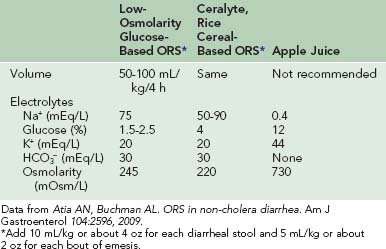
 tsp of salt in 1 cup of water) instilled into the nares a few minutes before aspiration helps to loosen mucus. Nasal aspiration should be reserved for times of most need, such as before feeding and sleep, because the procedure is irritating to a child. Other uses for a clean bulb syringe include flushing foreign bodies from ears and administering enemas.
tsp of salt in 1 cup of water) instilled into the nares a few minutes before aspiration helps to loosen mucus. Nasal aspiration should be reserved for times of most need, such as before feeding and sleep, because the procedure is irritating to a child. Other uses for a clean bulb syringe include flushing foreign bodies from ears and administering enemas.