Children in the Wilderness
What Makes Children Different
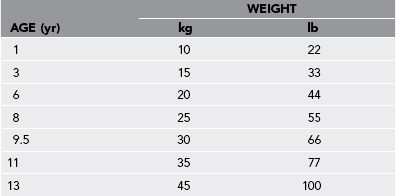
1. Medications and fluids must be calculated on the basis of the weight of the child (Table 62-1). One should also be aware of normal ranges of vital signs according to age (Table 62-2).
Table 62-1
From U.S. Centers for Disease Control and Prevention, National Center for Health Statistics (http://www.cdc.gov/nchs/).
Table 62-2
Age-Specific Resting Heart Rate and Respiratory Rate*
| AGE | HEART RATE (Beats/Min) | RESPIRATORY RATE (Breaths/Min) |
| 0-5 mo | 140 ± 40 | 40 ± 12 |
| 6-11 mo | 135 ± 30 | 30 ± 10 |
| 1-2 yr | 120 ± 30 | 25 ± 8 |
| 3-4 yr | 110 ± 30 | 20 ± 6 |
| 5-7 yr | 100 ± 20 | 16 ± 5 |
| 8-11 yr | 90 ± 30 | 16 ± 4 |
| 12-15 yr | 80 ± 20 | 16 ± 3 |
2. Children experience greater toxicity from envenomation because of the increased dose of venom per kilogram of weight.
3. Children are more likely to have incomplete “greenstick” fractures or injuries involving the growth plates.
4. Children are more susceptible to blunt chest and abdominal injuries due to their height and flexible ribs, which affords less protection of internal organs.
5. Children experience greater exposure to environmental factors such as cold, heat, and solar radiation because they have a larger body surface area–to–mass ratio than do adults.
6. Thermoregulation is less efficient in children, making them more susceptible to heat illness and hypothermia.
7. Children experience a greater number of infections than do adults.
8. Children are at greater risk for dehydration than are adults.
9. Small children tend to explore their environment with hands and mouths.
Age-Specific Expectations for Wilderness Travel
Table 62-3
Age-Specific Expectations for Wilderness Travel
| AGE | EXPECTATION | SAFETY ISSUES |
| 0-2 yr | Distance traveled depends on adults Use child carriers |
Provide “safe play area” (e.g., tent floor, extra tarp laid out), bells on shoes |
| 2-4 yr | Difficult age; stop every 15 min, hike 1-2 miles on own | Dress in bright colors, teach how to use whistle |
| 5-7 yr | Hike 1-3 hr/day, cover 3-4 miles over easy terrain, rest every 30-45 min | Carry whistle (three blows for “I’m lost”), carry own pack with mini first-aid kit and water |
| 8-9 yr | Hike a full day with easy pace, cover 6-7 miles over variable terrain; if over 1.2 m (4 feet) tall, can use framed pack | As for 5-7 yr, plus teach map use and route finding, precondition by increasing maximal distances by <10%/wk, watch for overuse injuries, keep weight of pack <20% of bodyweight |
| 10-12 yr | Hike a full day at moderate pace, cover 8-10 miles over variable terrain | As for 8-9 yr; expand route planning role, compass use |
| Teens | Hike 8-12 miles at adult pace; may see a decrease in pace or distance with growth spurt | As for 10-12 yr, but expand survival and wilderness first-aid knowledge. |
Environmental Illnesses
Treatment
1. Replace fluids and electrolytes.
a. Oral rehydration with water and oral rehydration solution (ORS) is the most important treatment for dehydration in the backcountry. Simply drinking plain water is inadequate replacement.
b. Gatorade can be used but should be diluted to half-strength with water.
c. Add commercial ORS containing sodium chloride, 3.5 g; potassium chloride, 1.5 g; glucose, 20 g; and sodium bicarbonate, 2.5 g to 1 L (1 quart) of drinking water.
d. Improvise an ORS by adding 5 mL (1 teaspoon) of table salt and 40 mL (8 teaspoons) of table sugar to 1 L (1 quart) of drinking (disinfected) water. A rice cereal–based rehydration solution is made by adding 5 mL (1 teaspoon) of table salt and 50 g (1 cup) of rice cereal to 1 L (1 quart) of drinking (disinfected) water.
e. For rapid treatment of mild to moderate dehydration, 50 to 100 mL/kg (1 to 1.5 oz/lb) of ORS should be administered over the first 4-hour period, followed by maintenance fluid volumes (75 to 150 mL/kg/day or 1 to 2 oz/lb/day). An additional 10 mL/kg, or 4 oz, can be given for each diarrhea stool and 5 mL/kg, or 2 oz, for each episode of emesis. If vomiting develops, most children will still tolerate ORS if given small volumes (5 to 10 mL [1 to 2 teaspoons]) every 5 minutes. Severe dehydration requires prompt medical attention and administration of IV fluids for rehydration.
Hypothermia (see Chapter 3)
Signs and Symptoms (Table 62-4)
Table 62-4
Signs and Symptoms of Hypothermia*
| RECTAL TEMPERATURE | SIGNS AND SYMPTOMS |
| Mild (33°-35° C) (91.4°-95° F) |
Sensation of cold, shivering, increased heart rate, progressive incoordination in hand movements, developing poor judgment |
| Moderate (28°-32° C) (82.4°-89.6° F) |
Loss of shivering, difficulty walking or following commands, paradoxical undressing, increasing confusion, decreased arrhythmia threshold |
| Severe (<28° C) (<82.4° F) |
Rigid muscles, progressive loss of reflexes and voluntary motion, hypotension, bradycardia, hypoventilation, dilated pupils, increasing risk for fatal arrhythmias, appearance of death |
Treatment
1. Remove any wet clothing, and replace with dry, insulating garments. Cover the child’s head and neck.
2. Place the child in a sleeping bag with a normothermic person.
3. Place hot water bottles insulated to prevent burns at the axillae, neck, and groin.
4. If the child is alert, administer oral hydration with warm fluids containing glucose.
High-Altitude Illness (see Chapter 1)
1. Avoid abrupt ascent to a sleeping altitude higher than 3000 m (9843 feet).
2. Spend two or three nights at 2500 to 3000 m (8202 to 9843 feet) before going higher.
3. Avoid abrupt increases of greater than 500 m (1640 feet) in sleeping altitude per night.
4. Provide acetazolamide prophylaxis (5 mg/kg/day, in two divided doses, up to a maximum daily dose of 250 mg started 24 hours before ascent and continued while at altitude) in children with a history of recurrent acute mountain sickness despite graded ascent.
Treatment
1. Descend at least 500 to 1000 m (1640 to 3281 feet).
2. Administer acetaminophen for headache.
3. Ondansetron (Zofran) or promethazine (Phenergan) may be used to relieve nausea and vomiting. Dystonia in response to phenothiazines, such as promethazine, occurs disproportionately in young children, so ondansetron is preferred. Ondansetron is given orally at 0.1 to 0.15 mg/kg up to 4 mg every 4 hours; promethazine is given at 0.2 to 0.5 mg/kg/dose up to 25 mg every 6 hours, preferably per rectum.
4. Administer oxygen if available.
5. Administer acetazolamide 5 mg/kg/day divided q12h up to 250 mg/day if symptoms persist despite descent.
6. Administer dexamethasone 0.6 mg IM/IV/PO q6h for children with deterioration of consciousness, truncal ataxia, or severe vomiting. The symptoms of high-altitude cerebral edema or high-altitude pulmonary edema demand immediate descent and possible evacuation.
Traveler’s Diarrhea
Treatment
1. Provide oral rehydration to correct dehydration and electrolyte losses (see earlier).
2. Give rice, bananas, and potatoes as supplements to ORS. Fats, dairy products, caffeine, and alcohol should be avoided.
3. If the patient is older than 2 years of age and does not have bloody diarrhea or fever, administer loperamide (Imodium). Weight-adjusted dose is 13 to 20 kg (1 mg q8h); 20 to 30 kg (2 mg q12h); greater than 30 kg (2 mg q8h).
4. In a severe case (fever, bloody stool, or abdominal distention), consider giving an antibiotic (azithromycin 10 mg/kg on day 1, then 5 mg/kg once daily for 2 days).
5. Consider using a probiotic agent such as Lactobacillus acidophilus for prevention and treatment. This is available over the counter with dosing of one tablet or capsule a day for children younger than 2 years and two capsules a day for children older than 2 years. Capsules can be opened and placed into food or drink for children unable or unwilling to take pills.






