4 Child development
Introduction
Assessing an individual child’s development depends on:
• How that child is developing over time
• How that child’s development compares with other normally developing children of the same age.
Taking a history
The history can give a picture of a child that cannot always be obtained from observation so it is important to allocate sufficient time. It is a good idea to have a format so that you can make sure that important details are not missed. This is covered in Chapter 1. Particular areas of importance when considering a developmental disorder are detailed below.
1. What are the parents’ concerns?
2. The birth history; where, how, gestational age and birth weight are important details. Did the baby require neonatal intensive care? Has anyone expressed concern about the baby?
3. Social history and family tree; include a history of the parents’ educational attainment and developmental concerns about other family members.
4. Find out if the child attends a playgroup or nursery; they may be with a child minder or family member for much of the day. Do they go to special groups and activities?
The developmental milestones are best asked about in a systematic way:
• Gross motor skills. Most parents can provide accurate information about the age of their child when they sat and walked. The Personal Child Health Record (‘red book’) is also a useful source of information
• Fine motor skills. Many parents find it difficult to remember dates when these milestones were achieved but are able to describe what their child can do now
• Speech and hearing. The results of hearing tests should be in the Personal Child Health Record. Most parents will remember when their child said their first word. They may recall that a professional expressed concern or told them that their child’s language development was normal. Health visitors, nursery nurses and pre-school staff are very astute in detecting delay in communication skills
• Play and social skills. It is difficult to remember the fine detail of these rapidly evolving abilities and often an accurate picture of current skills is the most useful information. Ask about whether the children play with, or alongside, others. Are they very shy? Do they have difficulty in separating from a parent or carer? What do they like to play with? Is there imaginative play? Do they enjoy looking at books? Is there pointing, copying and anticipation?
The motor skills
Babies develop motor skills if:
• They have a normal central nervous system
• They have the motivation to practise new skills
• They have the opportunity to practise new skills.
• Children who are visually impaired may lack confidence to walk independently (as in Case 4.1). They cannot see a really interesting toy so they may be less motivated to go in search of it.
• Case 4.2 shows an example of how a child has been given limited opportunity or motivation to lie in a prone position and to experiment with crawling.
• For some conditions, such as Down’s syndrome, condition-specific developmental milestones are available.
The motor milestones
Newborn to 3 months
Gross motor
A. Grasp reflex. Babies will grasp hold of an object stroked across the palm of their hands.
B. The Moro or startle reflex. A sudden noise causes babies to symmetrically extend their arms and legs.
C. Rooting reflex. If babies’ cheeks are gently stroked they will turn their heads to locate the touch.
D. Walking and placing reflex. If babies are held upright and the sole of the foot is placed on a firm surface they will extend the leg; if the dorsal surfaces of the feet are stroked they will pick up their feet as if to walk.
Play skills
Television is not an adequate substitute for playing with, and talking to, a baby.
The key milestones
There are three milestones, which, if not met, should ring ‘alarm bells’. These include:
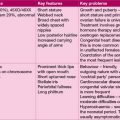
Learning difficulty (mental retardation)
Learning difficulties are defined by IQ. A severe learning difficulty, as in the above case, is defined as an IQ of less than 35, moderate as an IQ of between 35 and 50, and mild as an IQ of between 50 and 70. The lower the IQ the more likely an organic explanation exists for the child’s difficulties. Increasingly, genetic causes of learning difficulties are being discovered. Inquire into alcohol use in pregnancy as fetal alcohol syndrome is a significant cause of mental retardation (see Chapter 18, page 266). A detailed family tree and questioning about the academic ability of relatives is useful; referral to a clinical geneticist may be of value, particularly if there are dysmorphic signs. Careful physical examination should seek any evidence of associated health problems and a careful search for dysmorphic features which might suggest a genetic problem. Investigation should be tailored to the individual case. See Table 4.1 for a list of tests, which should be considered.
Table 4.1 Investigations to be considered in a child with learning difficulties
| Blood and urine tests |
| Full blood count and film Haemoglobin electrophoresis Thyroid function ToRCH Screen Creatine kinase Uric acid Calcium Cholesterol Low resolution micro-array (or Karyotype) Specific genetic tests: Fragile X, MECP2 gene analysis, telomere analysis as indicated Plasma and urine amino acids Urine organic acids Urine mucopolysaccharides White cell enzymes Acylcarnitines |
| Radiological investigations |
| Skull X-ray MRI or CT scan |
| EEG |
| Retinal examination |
Other common developmental disorders
Dyspraxia
Case 4.4 is an example of dyspraxia, which describes impaired execution and planning of motor tasks due to immaturity or impairment of the motor cortex, manifesting as clumsiness and impaired spatial awareness (motor dyspraxia), and impaired vocalization and tongue movement (verbal and oral dyspraxia). Affected children, more often boys (M:F = 4:1), are usually of normal intelligence.
Delay in bladder and bowel control
Nocturnal enuresis
Enuresis is defined as involuntary voiding of urine after the age of 5 years – most commonly at night – nocturnal enuresis (as in Case 4.5). By the age of 5 years, 93% of boys and 97% of girls are dry by day and night. By the age of 10 years, half of those with enuresis at the age of 5 years will be completely dry. If the child has previously been dry, the condition is described as secondary enuresis, and may be triggered by urinary tract infection, emotional upset or rarely, neurological problems.
In nocturnal enuresis, a careful history and examination are needed, but investigation other than urine dipstick testing is rarely necessary. The child with diurnal (daytime) enuresis, on the other hand, might need an ultrasound examination, including post-voiding to look for evidence of congenital anomalies and voiding dysfunction (‘irritable bladder’) (see Chapter 11, p. 125).
Treatment:
Second-line treatment includes:
• Use of alarms that awaken the child on wetting. Alarms are effective, but often unpopular with the rest of the family!
• Desmopressin (DDAVP) to reduce urine output. This is effective in reducing enuresis, but there is a high relapse rate. It is best reserved for special occasions, e.g. sleep-overs or holidays.