Chapter answers
Chapter 2
1 A. The conduction velocity of the AV node results in a PR interval that is always between 120–200 ms in a normal heart.
3 C. Since the T wave denotes the period during which ventricular repolarization takes place, the end of this wave corresponds to repolarization of the longest duration action potentials, which are those in the endocardial cells.
4 B. The duration of the QRS complex denotes the time taken for depolarization of the entire ventricular myocardium.
5 F. The AV valves open when ventricular muscle relaxation is complete and close at the beginning of ventricular contraction.
6 B. The normal velocity of impulse propagation through the ventricular syncytium causes depolarization of the whole muscle mass within 50–80 ms. If the time taken for ventricular depolarization is greater than 80 ms, then the velocity of action potential propagation is abnormally slow OR the normal conduction pathway is blocked at some point.
Chapter 3
2 D. Release of catecholamines increases contractility of all myocardial cells, but it is only atrial contraction that can contribute to ventricular filling. Other factors that aid filling are decreased intrathoracic pressure during inspiration and muscle pumping causing compression of limb veins. Increased heart rate may increase end-systolic volume, but does not affect ventricular filling.
3 C. Ventricular filling is limited by the increased stiffness of both myocardium and pericardium at high filling volumes and by the fact that the calcium channels that determine ventricular action potential plateau duration have a finite minimum cycle time, so that above a certain heart rate the diastolic filling time is shortened. With exercise modalities that elevate diastolic blood pressure, this rise in afterload also limits ventricular emptying. Sympathetic activation and catecholamine secretion continue to rise proportionately to exercise intensity up to maximum work capacity.
Chapter 4
1 E. Sympathetic activation increases stroke volume both by increasing cardiac filling (due primarily to mobilizing blood from venous reservoirs) and by increasing cardiac emptying (due to increased myocardial contractility). The effect on peak blood pressure of this larger stroke volume is enhanced by faster ejection by more rapid myocardial depolarization and by reduced aortic distension because of vascular muscle contraction.
2 A. Remember that the formula for calculation of mean blood pressure at rest is DBP + ⅓ PP or (SBP + 2DBP). Only at the high heart rates that occur during heavy exercise, DBP + 2/5 PP, may be slightly more accurate.
3 A. Conversion of laminar to turbulent flow is enhanced by increased velocity of flow and increased vessel diameter. This situation occurs where blood whose flow velocity has been increased by vessel compression under the cuff enters the wider, non-compressed segment immediately downstream. With cuff inflation to pressures between systolic and diastolic pressures, flow is necessarily intermittent. However, with the high flow velocities associated with high cardiac outputs, Korotkow sounds may still be heard when the cuff is inflated to pressures significantly below DBP and flow is continuous.
4 C. Decreased peripheral resistance will reduce DBP. If stroke volume and heart rate remain constant, then the pulse pressure will remain constant. Pulse pressure is inversely proportional to heart rate if all other factors remain unchanged, and is greater in peripheral arteries than in aorta because aortic compliance damps the pressure oscillations.
5 D. Peripheral resistance = mean BP/CO = 96/16 PRU. Remember that the PRU unit varies in magnitude depending on the way in which cardiac output is expressed. Here, the PRU incorporates cardiac output as expressed in l/min. If cardiac output was expressed in ml/min, then peripheral resistance would be 96/16 000 or 0.006 PRU.
Chapter 5
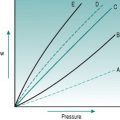
1 D. When sympathetic tone is high, a greater intravascular pressure is needed to balance the tendency of the vessel wall to contract inwards. Wall tension is proportional to transmural pressure and to the ratio of luminal diameter:wall thickness, so it rises with BP and is higher in large vessels with high intravascular pressures. The elastic properties of the aortic wall make it stretch in response to increased BP; the presence of collagen limits this expansion and the risk of rupture.
Chapter 6
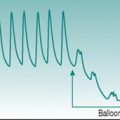
1 C. Vasomotion describes the process of intermittent opening and closing of metarterioles supplying different areas of a tissue capillary bed. This is due to local oscillations in critical closing pressure dependent on the rate of interstitial metabolite accumulation. The cycle time in a resting tissue is typically of the order of 20–30 s.
2 B. The rapid onset of hyperaemia at the beginning of muscle activity is probably due to liberation of potassium ions from the contracting cells. The subsequent sustained hyperaemia, which may reach 10–20 times resting flow, is due primarily to muscle-derived metabolites, with smaller contributions from endothelium-derived factors, catecholamine-induced β-adrenoreceptor activation and, particularly in oxidative motor units, muscle-derived NO and PGs.
3 A. The process of eccrine sweat secretion liberates into the glandular interstitium both kallidin and the associated vasodilator peptide, bradykinin.
Chapter 7
1 E. Baroreceptor firing inhibits the hindbrain neurons that activate sympathetic vasomotor drive to kidney, digestive tract and skeletal muscle. The low-pressure atrial baroreceptor pathway also inhibits hypothalamic release of vasopressin. As the baroreceptors function by detecting mechanical distortion of the axon endings, arterial baroreceptor discharge varies less with intravascular pressure when the arterial wall is less distensible.
2 D. The kidney is a major source of peripheral resistance elevation during exercise, but this is achieved primarily by increasing arteriolar resistance distal to the glomeruli, so that the effect on filtration of reduced glomerular blood flow is balanced by the increased glomerular capillary hydrostatic pressure.
3 C. Resetting of the operating point is thought to be due to input from the central command. The sustained elevation of BP is useful in maintaining nutritional perfusion to those tissues in which vascular resistance has been increased by the exercise response.
4 B. The more pronounced pressor response to upper-body exercise is due mainly to the greater total peripheral resistance that results from sympathetic vasoconstriction in the inactive muscles of the lower body. BP elevation is greatest during static activity due to input from muscle metaboreceptors and at high static loads the reduction in venous return may lead to a fall in stroke volume and SBP.
5 A. Coronary blood flow rises proportionately to cardiac workload and this is reflected by cardiac output. Since even at rest there is some degree of functional hyperaemia in the coronary circulation, all coronary capillaries are always open. As the left heart produces more work than the right, functional hyperaemia must be greater on the left side. Around 25% of the exercise-induced coronary hyperaemia is due to β-adrenoreceptor activation by sympathetic nerves and circulating adrenaline (epinephrine).
6 E. The pressor response to static exercise is pronounced even with contraction of small muscle groups and is due primarily to metaboreceptor stimulation and central command. Because of the absence of muscle perfusion, peripheral resistance rises in response to the increased sympathetic drive, and so both DBP and SBP increase proportionately. At maximal workloads, the mechanical restriction to venous return often causes a fall in stroke volume sufficient to lower BP slightly.
Chapter 8
1 C. Although both ventilation and perfusion are lower at the lung apices than the lung bases in a standing individual, blood flow is reduced to a greater extent due to the difficulty in pumping blood against a gravitational head.
2 E. The relatively low right ventricular systolic pressure means that cardiac workload is always lower in right than in left heart and that the right coronary vasculature is not occluded during cardiac contraction. The small pressure loss between pulmonary arteries and veins means that wedge pressure can be used to approximate beat-to-beat left atrial pressure.
3 D. The combination of increased tidal volume, increased right heart stroke volume and pulmonary arteriolar dilatation produces more efficient gas exchange in areas of lung that are either not fully perfused or not fully ventilated at rest.
4 C. Since there is equilibration between air and plasma by the time the plasma has travelled about ⅓ of the length of the pulmonary capillary, cardiac output can rise around threefold before O2 uptake begins to be impaired. Shifts in the haemoglobin curve affect offloading of O2, but have no effect on haemoglobin uptake of O2 at normal PaO2.
Chapter 9
1 A. Sweat in non-heat acclimatized individuals contains around 2.5 g sodium chloride/l and cannot be secreted at rates greater than around 1 l/h. Secretion is less efficient in children and older adults. When relative humidity is low, evaporative heat loss is more efficient and so less sweat is needed to achieve thermal stability.
2 E. Absorption of fluid is enhanced by ingestion of hypotonic fluid containing around 20 g glucose/l. Gastric emptying is slowed if the fluid is very cold or if a large volume is ingested.
3 E. Muscle perfusion is reduced both by diversion of some cardiac output to skin to service thermoregulatory demands and by the progressive fall in plasma volume due primarily to sweating. These factors result in greater encroachment on heart rate reserve, with reduced efficiency of cardiac filling. The rise in heart rate and the increased blood viscosity caused by plasma depletion increase cardiac workload for any given exercise intensity.
Chapter 10
1 D. The reduction in cerebral perfusion induced by the Valsalva manoeuvre is exaggerated by hypocapnia and by circulating adrenaline (epinephrine), both of which raise cerebral vascular resistance, and by reduced plasma volume associated with voluntary weight reduction.
2 D. Ecstasy increases thyroid hormone release and, therefore, up-regulates basal metabolic rate in chronic users.
3 B. Abnormality of the RYR1 gene causes excessive calcium release from skeletal muscle sarcoplasmic reticulum onto the sarcomeres, with local heat-induced muscle damage and generalized hyperthermia.
4 A. Hyperthermia is more likely when reduced plasma volume jeopardizes sweat production and skin perfusion, but may occur without fluid depletion if the individual is wearing clothing that prevents heat exchange. Highly motivated athletes are sometimes able to continue exercise even in the face of severe hyperthermia. Because of reflex vasoconstrictor responses to skin cooling, immersion in tepid rather than cold water is the more effective treatment for most cases of hyperthermia.
5 C. The countercurrent organization of the microcirculation in renal medulla and intestinal villi means that these areas are especially sensitive to hypoxic damage when blood flow is reduced. Hypotension results from falls in blood volume above around 20% and, in the upright position, cerebral perfusion will be most sensitive to this. The collapse consequent upon plasma volume depletion is termed heat exhaustion to distinguish it from the direct effect of hyperthermia, known as heat stroke.
Chapter 11
1 B. Age-dependent HR maximum is 190 beats/min, so nominal heart rate reserve = (190–72) = 120 beats/min. A sedentary person can increase cardiac output to around four times the resting value = 22 l/min. Normal maximal sweat secretion is around 1 l/h and normal sweat sodium content is around 50 mmol.
2 C. The increased plasma volume due to training for 3 weeks would be expected to produce a resting bradycardia of up to 10 beats/min, with a small consequent increase in maximum cardiac output. The expanded blood volume and the associated increase in peripheral aldosterone receptors will increase maximum sweat production and increase sweat duct reabsorption of sodium ion.
3 F. Training for an extended period can be predicted to produce more pronounced resting bradycardia than would occur during short term activity, due to cardiac remodelling. This will lead to a proportionate rise in maximum cardiac output.
4 C. Plasma volume is increased after only one to two training sessions due to aldosterone-mediated sodium and water retention, leading to a fall in haematocrit. Decreased resting heart rate and increased stroke volume are not seen until training has progressed for some weeks.
5 A. The process of cardiac remodelling in response to chronically increased preload occurs initially in right heart and is not complete in left heart until after around 6–9 months of training. Concentric hypertrophy, which occurs in response to increased afterload, results in a greatly thickened ventricular wall that predisposes to endocardial ischaemia and arrhythmias.
6 C. Chronic dynamic exercise leads to reduced peripheral resistance secondary to peripheral angiogenesis, more rapid endothelial turnover and reduced sympathetic gain. All of these adaptations lower blood pressure, which in turn reduces shear stress in the large arteries where flow velocity is high and lowers the risk of endothelial damage.
Chapter 12
2 E. Although normal gas exchange is maintained so that PaO2 and PaCO2 remain normal, lactate accumulation has slightly lowered blood pH.
3 C. The acute response to hypoxia is increased minute ventilation. This produces hypocapnia and so increases blood pH.
4 B. Acclimatization to a hypoxic environment reduces the inhibitory effect of hypocapnia on respiratory drive and so allows greater minute ventilation. As well, renal acid–base compensations to alkalosis take place. As a result, blood pH falls to a value close to normal despite further ventilation-induced hypocapnia.