Cesarean Section
Cesarean section is one of the most commonly performed operations in the United States. A transverse or vertical entry laparotomy is performed. A transverse incision is selected more frequently (by a ratio of 10 to 1). The uterus may be left in situ within the abdominal cavity, or it may be exteriorized.
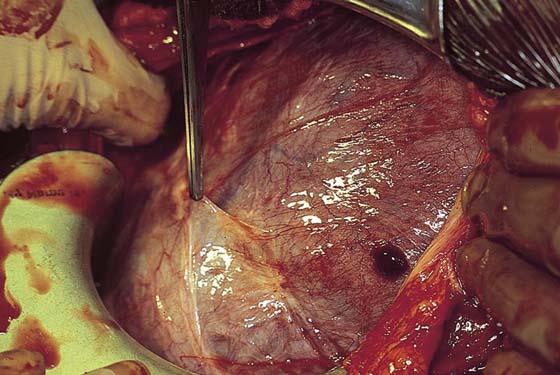
The technique of low transverse cesarean section is performed as follows. The bladder is emptied by the insertion of a Foley catheter. First, a bladder blade is inserted anteriorly (Fig. 18–1). The small and large intestines are packed away with moistened abdominal (laparotomy) pads, which should be carefully counted and tagged. The round ligaments should be identified so the degree and direction of uterine rotation can be determined. Identification of enlarged or aberrant vessels should be documented.
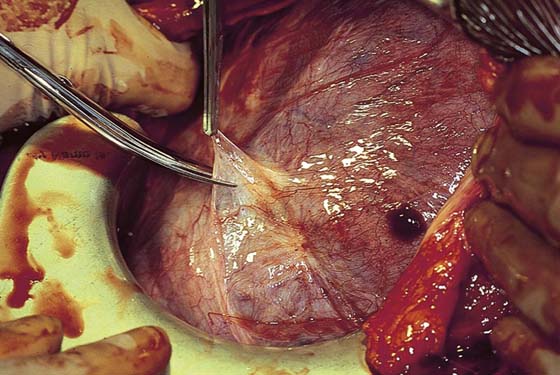
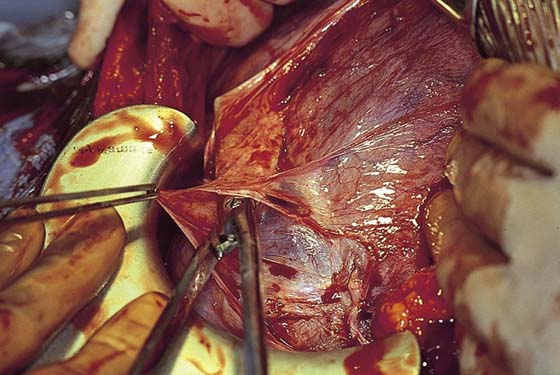
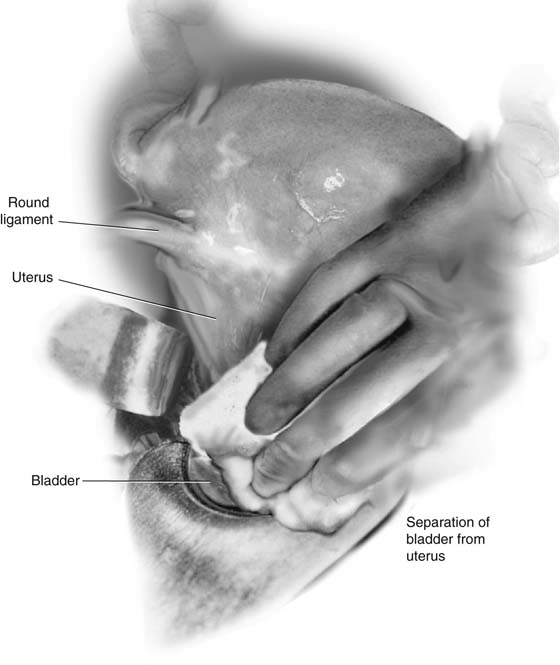
The reflection of peritoneum from the bladder dome to the uterus is grasped with a Kelly clamp (Fig. 18–2). The peritoneal reflection is elevated. With a Metzenbaum scissors, the bladder peritoneal reflection is sharply divided and is extended transversely for the length of the proposed uterine incision, typically 8 to 10 cm (Figs. 18–3 and 18–4). The bladder is gently pushed inferiorly away from the lower uterine segment. This not uncommonly results in small-vessel disruption and light bleeding (Fig. 18–5).
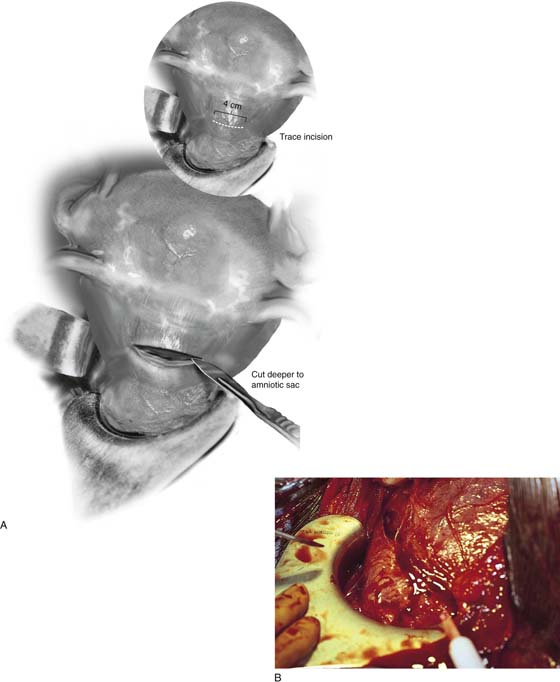
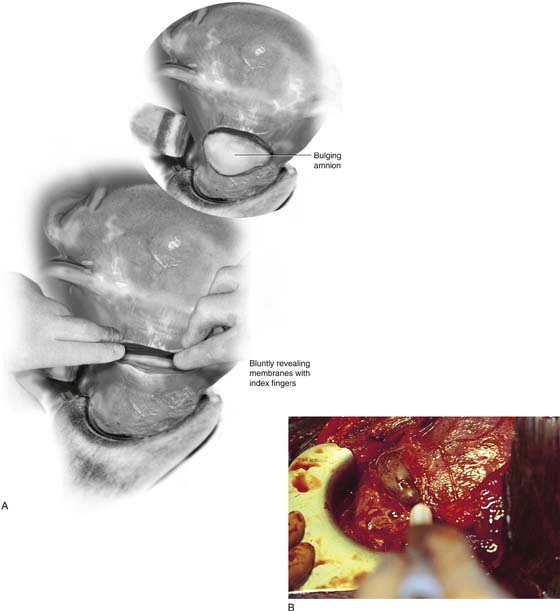
A trace incision is made into the uterus above the bladder reflection (Fig. 18–6). With the use of a scalpel, a deeper central cut, approximately 4 cm in length, is carried down to the amniotic sac, which bulges through the wound (Fig. 18–7A, B). Alternatively, the sharp incision is stopped just short of entry into the uterine cavity. At this point, the muscle may be spread with the surgeon’s index fingers and the cavity entered bluntly (Fig. 18–8A, B).
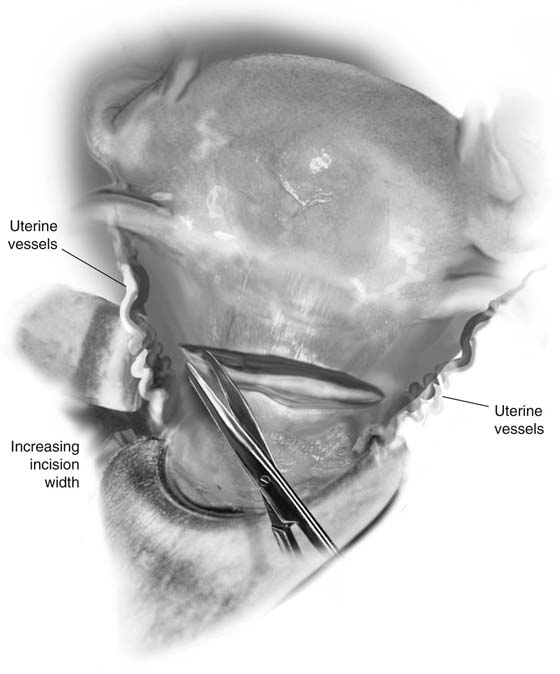
In either case, once the bulging membranes have been identified, the incision may be extended to right and left by using scissors or by spreading with fingers (Fig. 18–9). The location of the uterine arteries should be ascertained to avoid inadvertent extension of the incision through them. The membranes are opened, and amniotic fluid is suctioned as it pours out into the wound.
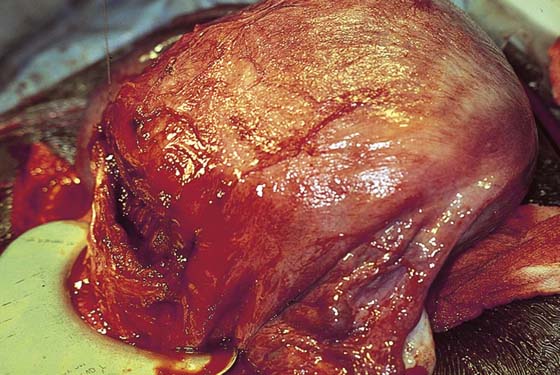
The head of the infant (cephalic presentation) appears beneath the incision (Fig. 18–10). It is grasped beneath the chin and occiput and is gently delivered. It is rotated to facilitate delivery of the shoulders, and this is followed by delivery of the breech. The umbilical cord is clamped (doubly) and cut. The placenta is now seen in the depths of the wound (Fig. 18–11). It is separated and extracted. The uterine cavity is manually explored and clots are evacuated. The edges of the incision are grasped with Babcock clamps. A 10-mm Hegar dilator is passed through the cervix. Alternatively, a 36-French Pratt dilator may be passed through the cervix to facilitate lochial drainage. The incision is inspected for any extensions. The uterine vessels and bladder are checked for any injuries.
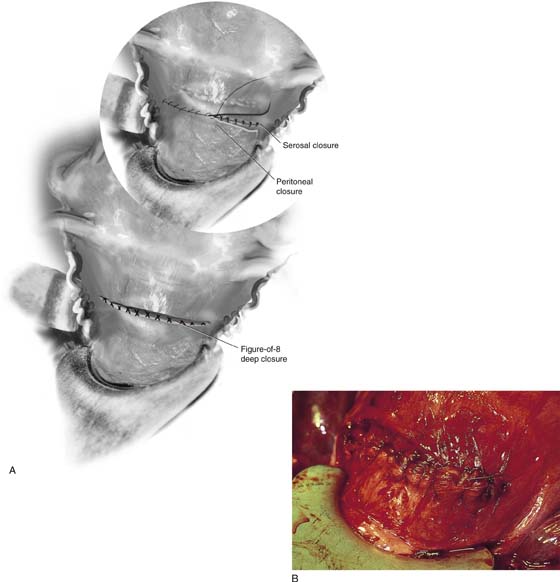
The incision is closed in layers. The deep muscle is approximated with interrupted figure-of-8 suture ligatures of 0 Vicryl (Figs. 18–12 and 18–13A). The superficial muscle and the uterine serosa are closed by a running 0 Vicryl (see Fig. 18–13A, Inset, and 18–13B). The bladder flap peritoneum is sutured over the incision with running 3-0 Vicryl or PDS suture.
The uterus is massaged and replaced into the abdominal cavity. Retractors and packs are removed and carefully counted to ensure that each and every implement has been accounted for.
A low vertical section may be performed by incising vertically through the lower uterine segment. Care must be taken to avoid extension of this incision into the bladder. The only advantage of this incision is that it permits further extension superiorly into the active portion of the uterus to gain greater space to manipulate the fetus (e.g., in the delivery of a transverse presentation).
FIGURE 18–1 Full-term pregnant uterus exposed and exteriorized. A bladder retractor is seen in the foreground. The edges of the entry incision are beneath the obstetrician’s hands.
FIGURE 18–2 The peritoneal reflection between the bladder and the uterus is elevated.
FIGURE 18–3 The bladder peritoneum is incised sharply in an avascular plane. Vascularization of this peritoneum may be seen in cases of placenta previa or accreta.
FIGURE 18–4 The dissection is completed along the length of the anticipated deeper uterine incision.
FIGURE 18–5 The operator gently pushes the bladder inferiorly, detaching it from the lower uterine segment.
FIGURE 18–6 The lower uterine segment is now exposed. The uterine arteries are palpated to determine the lateral extreme of the uterine incision.
FIGURE 18–7 A. A small (3- to 4-cm) trace incision is made, then is extended deeper through the myometrium. B. At this point, bleeding is brisk, and suctioning is essential to detect when the uterine cavity has been entered.
FIGURE 18–8 A. Alternatively, the cavity may be entered bluntly by spreading the index fingers through the last thin layer of myometrium. B. The appearance of bulging membranes signals entry into the endometrial space.
FIGURE 18–9 With the membranes intact, the small entry incision may be widened laterally.
FIGURE 18–10 The membranes are now ruptured and widely opened. The infant’s head comes into view, and delivery is implemented.
FIGURE 18–11 The placental location is observed and recorded. Next, the placenta is manually removed. The uterine cavity is explored and cleared of any adherent membranes.
FIGURE 18–12 The deeper muscle is closed with interrupted 0 Vicryl figure-of-8 sutures.
FIGURE 18–13 A. The superficial muscle and uterine serosa are closed with running or running lock sutures of 0 Vicryl. B. After the serosa is closed, the bladder peritoneum is sutured to the uterus at the upper margin of the incision.