Cervical Stump Excision (Trachelectomy)
A cervical stump is the remnant of the uterus that remains following a subtotal hysterectomy (Fig. 50–1). Historically, supracervical hysterectomy was performed under adverse circumstances whereby rapid termination of the operation was essential for the well-being of the patient (e.g., in the complicated pregnancy). However, more recently surgeons are electively performing laparoscopic or robotic subtotal hysterectomy. Subsequent removal of the stump, or trachelectomy, may be required for various reasons, including persistent bleeding, prolapse, pain, and abnormal cervical pathology.
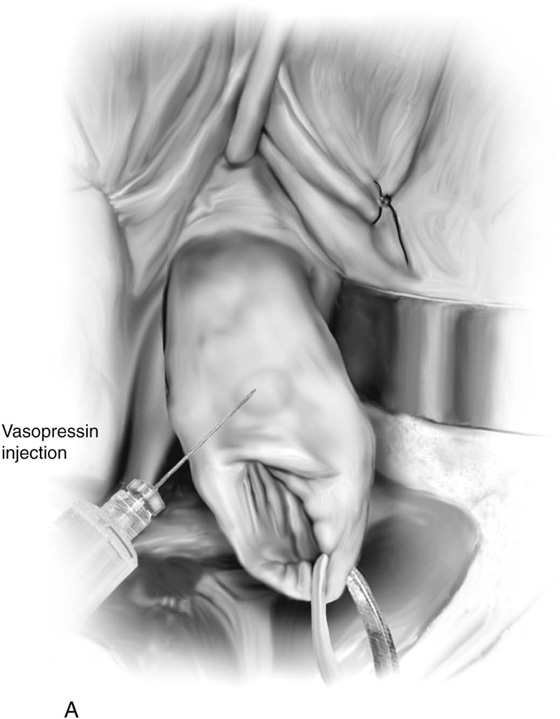
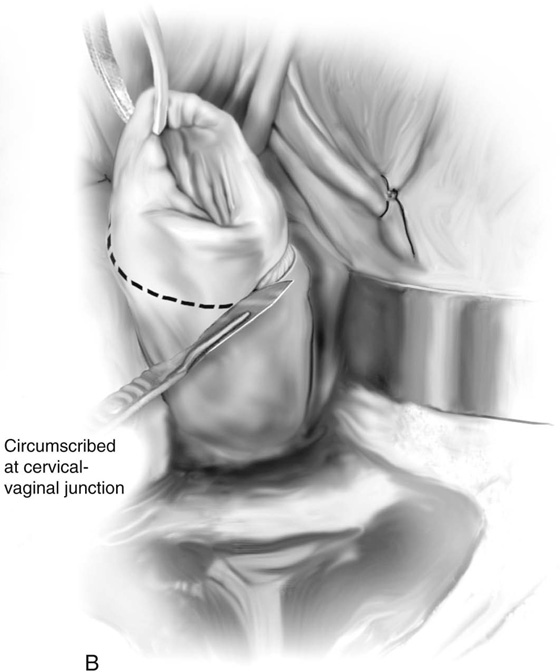
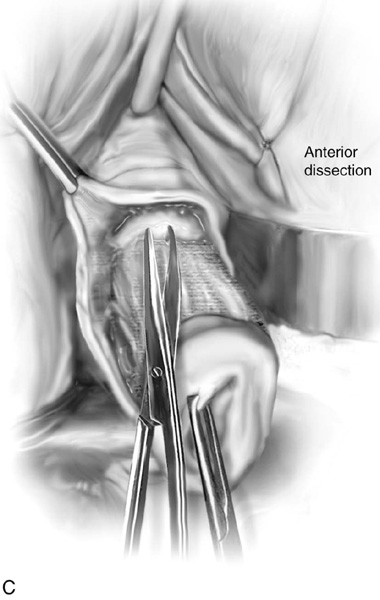
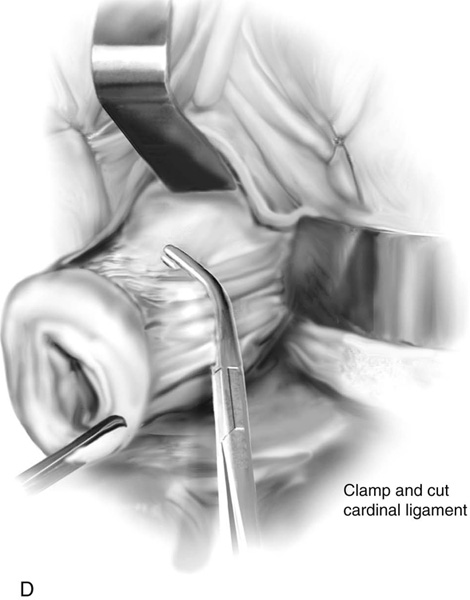
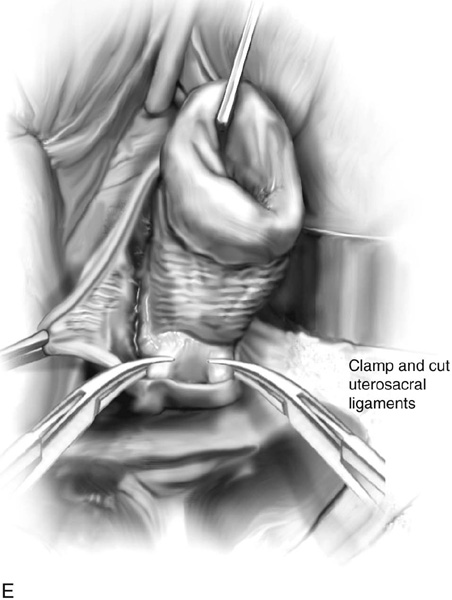
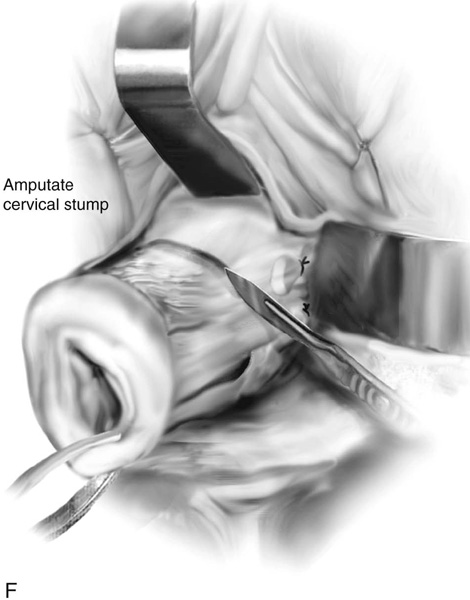
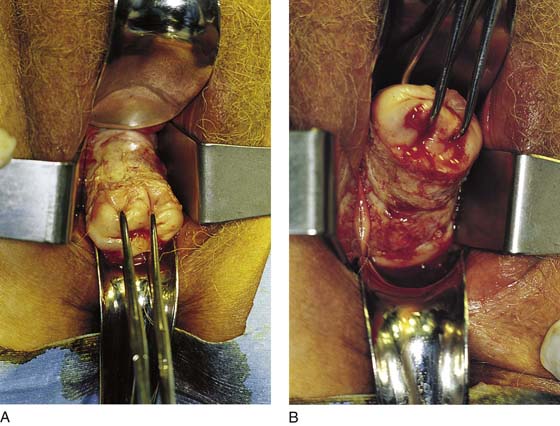
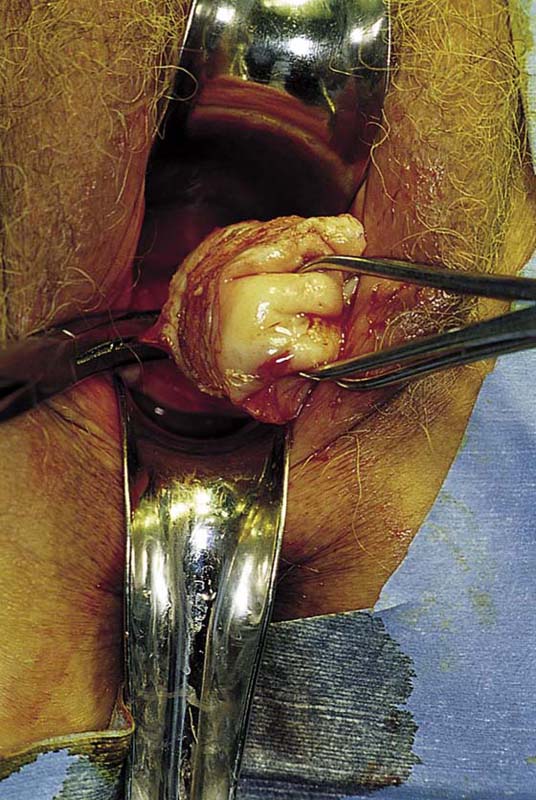
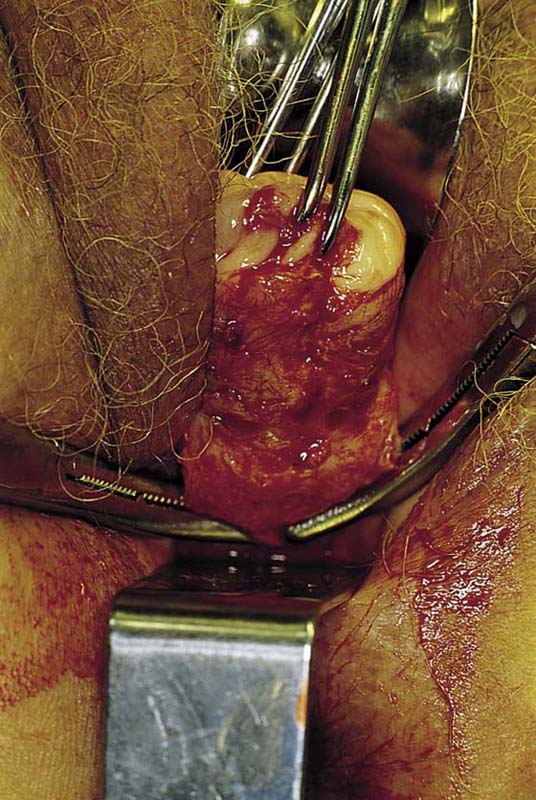
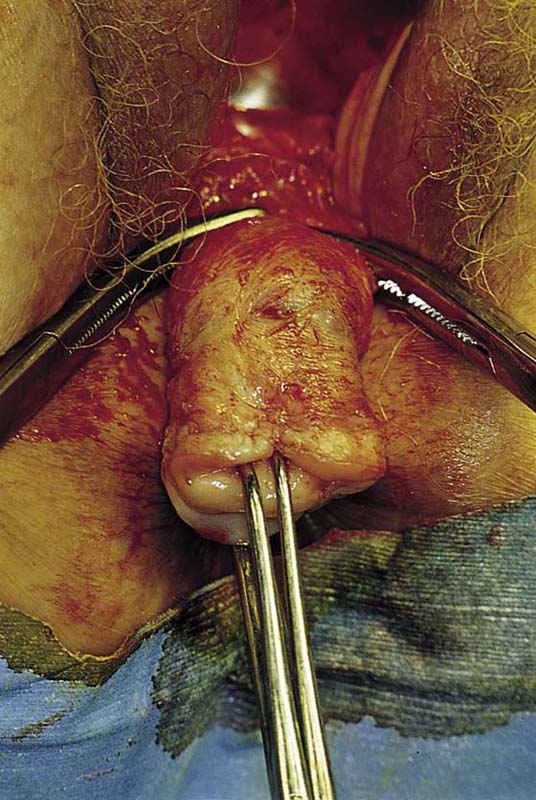
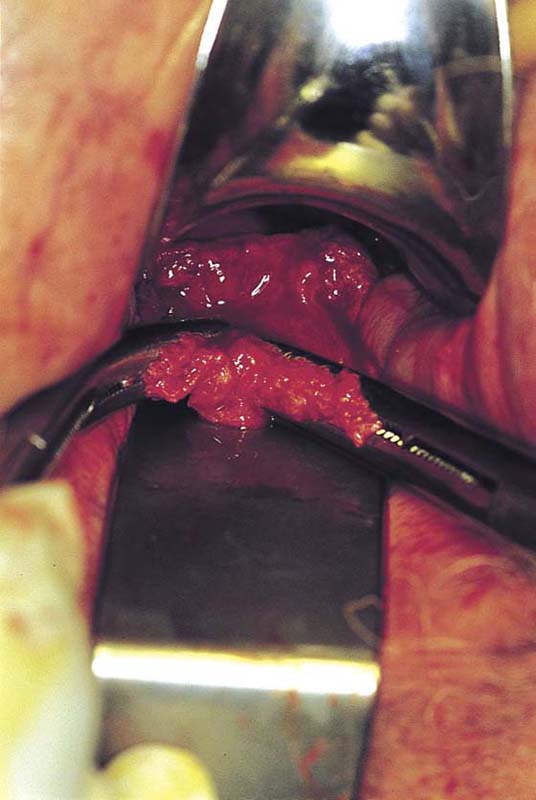
The cervical stump is removed in an identical fashion to the initial steps of a vaginal hysterectomy. Although entering the peritoneal cavity is not mandatory, it is preferred to ensure complete removal of the cervix and to allow for obliteration of the cul-de-sac and suspension of the vagina in cases of prolapse. The stump is grasped with a single-toothed tenaculum and is pulled inferiorly. A 1 : 100 diluted vasopressin solution is injected beneath the cervical and vaginal mucosa with a 25-gauge needle and a triple-ring 10-mL syringe. The solution will help to develop a plane of dissection. The injections are performed circumferentially around the cervix (Fig. 50–2A). With a scalpel, an incision is made into the cervix and is circumscribed below the cervicovaginal junction (Fig. 50–2B). The bladder is dissected from the cervix anteriorly; the vagina, together with the ureters, is pushed upward (craniad) from the lateral aspect of the cervix (Figs. 50–2C and 50–3A). The cul-de-sac and the rectum are dissected free posteriorly (Fig. 50–3B). The lower portion of the cardinal ligaments is clamped with curved Zeppelin clamps (Figs. 50–2D and 50–4). The uterosacral ligaments are identified and clamped (Figs. 50–2E and 50–5). The clamped structures are cut and transfixed with 0 Vicryl sutures. The cervix is kept taut by downward traction of the tenaculum and is completely freed from the rectum posteriorly (i.e., the rectovaginal space is dissected free from the cervix) (Fig. 50–6). The bladder may be adherent to the stump; thus sharp dissection should always be utilized to mobilize the bladder off the cervix (Fig. 50–7). The Metzenbaum scissors are directed away from the bladder and toward the stump in a carefully executed spread-and-cut technique. The stump is cut free and removed (Figs. 50–2F, 50–8, and 50–9). The cardinal and uterosacral stumps are sutured into each vaginal angle, and the vagina is closed transversely with interrupted 0 Vicryl sutures. If prolapse is present, a culdoplasty or a vaginal vault suspension should be performed (see Chapters 53 and 55).
As a cautionary note, it should be understood that during the supracervical hysterectomy, the bladder peritoneum may be advanced over the top of the cervix and sutured down posteriorly as a means of covering and peritonizing the stump. Conversely, the peritoneum of the sigmoid colon may be advanced and sutured anteriorly for the same purpose.
FIGURE 50–1 This cervix remained in situ following a laparoscopic subtotal hysterectomy. The patient subsequently desired removal of the cervix because of a persistent foul discharge and postcoital bleeding.
FIGURE 50–2 A. The cervix is grasped with a tenaculum and is pulled downward. A fine needle is inserted submucosally, and a 1 : 100 vasopressin solution is injected at the 12 o’clock position and is continued circumferentially around the cervix. B. A scalpel is used to make a circumscribing incision into the cervix approximately 5 to 10 mm back from the external os. C. The bladder is sharply dissected from the cervix together with the anterior vagina; similarly, the posterior vagina and the cul-de-sac are dissected free of the cervix. D. The lower portion of the cardinal ligament is clamped. E. The uterosacral ligaments are similarly clamped, cut, and suture-ligated. F. The cervical stump, after having its ligamentous and vascular pedicles secured, is cut free by means of a sharp scalpel or scissors.
FIGURE 50–3 A. The bladder has been dissected free from the anterior aspect of the cervix by means of Metzenbaum scissors. Note the downward tension on the cervix. B. The cul-de-sac and the rectum are freed from the posterior aspect of the cervix. Again, note the upward traction on the cervix, which facilitates the posterior dissection.
FIGURE 50–4 The cardinal ligaments are clamped, cut, and suture-ligated with 0 Vicryl sutures.
FIGURE 50–5 The uterosacral ligaments are clamped, cut, and suture-ligated.
FIGURE 50–6 The top of the cervix is cross-clamped. Note that the rectum has been sufficiently mobilized off the posterior aspect of the cervix.
FIGURE 50–7 The bladder and ureters have been mobilized superiorly and out of the way of these clamps.
FIGURE 50–8 The stump has been excised over the clamps. The upper portions of the cardinal ligaments are suture-ligated with 0 Vicryl or polydioxanone (PDS).
FIGURE 50–9 The 4-cm-long removed stump is sent to pathology for sampling. If intraepithelial neoplasia were present or suspected, the cervix would be cut up analogous to conization and serially sectioned.

 Michael S. Baggish
Michael S. Baggish