CHAPTER THREE CERVICAL SPINE
AXIOMS IN ASSESSING THE CERVICAL SPINE
INTRODUCTION
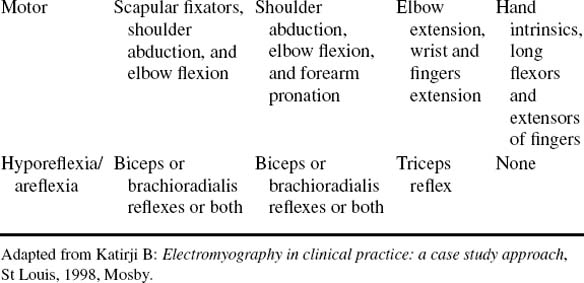
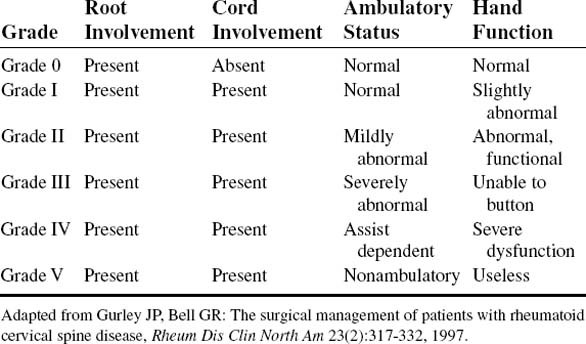
The nerve roots in the neck are particularly vulnerable to injury because of their relatively horizontal position in comparison with those of the lumbar spine. Stretching of the spinal cord itself is greatest at the cervical spine, which also predisposes the cord and nerve roots to trauma (Tables 3-1 and 3-2).
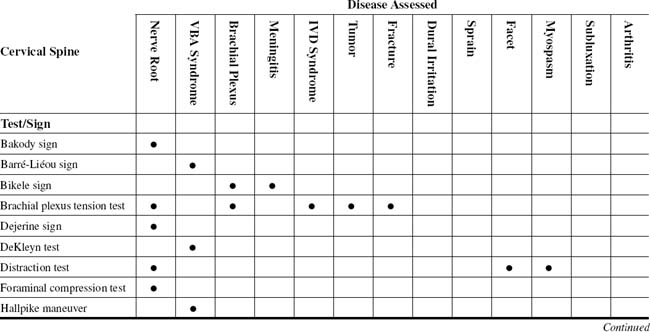
TABLE 3-2 CERVICAL SPINE CROSS-REFERENCE TABLE BY SYNDROME OR TISSUE
| Arthritis |
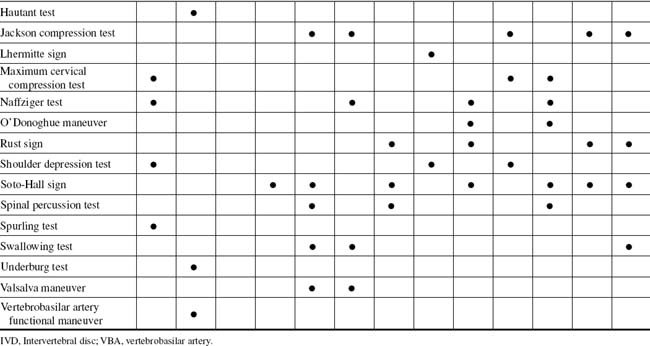
Many provocative tests can be used for the cervical spine. The anatomic structures commonly tested are dural tension, foraminal and vertebral canal patency, and muscle, tendon, or ligamentous injuries (Table 3-3). During investigation of the upper extremity, the examiner must differentiate between canal or nerve root lesions by physical examination and, if necessary, electrodiagnostic studies. Cervical spine canal stenosis, whether of bony or soft-tissue origins, can cause lower-extremity signs and symptoms. Most notable is long tract pain, or rhizalgia, appearing in an ipsilateral leg with a cervical nerve root lesion (Table 3-4).
TABLE 3-3 COMMON PROVOCATIVE TESTS TO EVALUATE THE SPINE
| Provocative Test | Anatomic Structures Being Tested | Positive Finding(s) |
|---|---|---|
| Cervical Spine | ||
| Jackson compression test | Dural sheath, nerve root, spinal nerve | Radicular pain |
| Spurling compression test | Dural sheath, nerve root, spinal nerve | Radicular pain |
| Maximal foraminal compression test | Dural sheath, nerve root, spinal nerve | Radicular pain |
| Distraction test | Dural sheath, nerve root, spinal nerve | Relief of radicular pain |
| Shoulder depression test | Dural sheath, nerve root, spinal nerve, brachial plexus | Radicular pain to one or more dermatomes |
| E.A.S.T. test | Subclavian artery | Vascular compromise |
| Eden test | Scalene musculature | Radiculopathy to multiple dermatomes or vascular compromise |
| Thoracic Spine | ||
| Wright hyperabduction test | Pectoralis minor | Vascular compromise, subclavian artery, TOS |
| Tests for anterior thoracic wall | Peripheral nerve, muscles | Radicular pain, dull ache |
| Lumbar Spine | ||
| Straight leg raise | Dural sheath, nerve root, spinal nerve | Radiculopathy to one dermatome usually |
| Braggard test | Dural sheath, nerve root, spinal nerve | Radiculopathy to one dermatome usually |
| Bekhterev (Bechterew) test | Dural sheath, nerve root, spinal nerve | Radiculopathy to one dermatome usually |
| Neri bow string test | Dural sheath, nerve root, spinal nerve | Radiculopathy to one dermatome usually |
E.A.S.T., Elevated arm stress test; TOS, thoracic outlet syndrome.
From Greenstein GM: Clinical assessment of neuromusculoskeletal disorders, St Louis, 1997, Mosby.
TABLE 3-4 CLASSIFICATION OF POST–SPINAL CORD INJURY PAIN STATES
| Acute Phase Pains | Chronic Phase Pains |
|---|---|
Adapted from Beric A: Post-Spinal Cord Injury Pain States, Anesthesiol Clin North Am 15(2):445-463, 1997.
ORTHOPEDIC GAMUT 3-1 CERVICAL SPINE PAIN
Differential diagnostic possibilities of cervical spine pain include:
ESSENTIAL CLINICAL ANATOMY
ORTHOPEDIC GAMUT 3-3 CATEGORIES OF INTRACTABLE SPINAL CORD INJURY PAIN
ORTHOPEDIC GAMUT 3-4 NEURAL RESPONSES
Pathologic neural responses to cervical injury can be grouped into four categories:
The intervertebral discs are fibrocartilaginous flattened structures interposed between adjacent vertebral bodies. Each disc consists of a gelatinous inner region (i.e., the nucleus pulposus), surrounded by a solid ring of stiffer material (i.e., the annulus fibrosus).
ESSENTIAL MOTION ASSESSMENT
ORTHOPEDIC GAMUT 3-5 VERTEBRAL MUSCLES
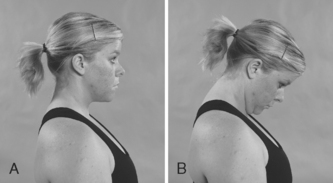
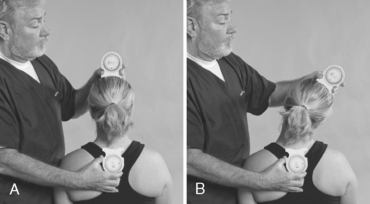
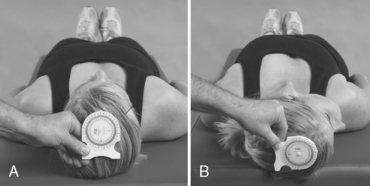
During a cervical spine range-of-motion assessment, the examiner should examine active then passive movements. For flexion, the patient brings the chin onto the chest; for extension, the patient bends the head backward as far as possible. For lateral flexion, the patient brings an ear toward the shoulder, first on one side and then on the other. For rotation, the patient looks over one shoulder and then the other. Repeating the movements while applying gentle pressure over the vertex of the skull may trigger pain or paresthesia in the arm if a critical degree of narrowing exists at an intervertebral foramen. In evaluating cervical spine range of motion, the examiner observes not only the total range of movement, but also the smoothness and comfort with which the patient accomplishes the motions (Figs. 3-1 to 3-8).
ESSENTIAL MUSCLE FUNCTION ASSESSMENT
ORTHOPEDIC GAMUT 3-6 CERVICAL SPINE MUSCLE STRENGTH
To evaluate cervical spine muscle strength, the patient takes the following actions:
The intrinsic longitudinal vertebral muscles, placed more superficially, are collectively called the erector spinae. The cervical region contains elongated muscles originating from the spinous process (the splenius muscles) and others from the transverse processes (the semispinalis muscles). The suboccipital muscles are a special group of muscles linking the atlas, the axis, and the base of the skull.
ESSENTIAL IMAGING
Plain-Film Imaging
ORTHOPEDIC GAMUT 3-8 CERVICAL SPINE PLAIN FILM SERIES
The typical cervical spine plain-film series consists of the following:
Specific views are used to evaluate complex regions of anatomy or spinal placement at extremes of motion (Box 3-1).
BOX 3-1 ACCEPTED ADDITIONAL CERVICAL SPINE PLAIN-FILM IMAGING
Data from Greenstein GM: Clinical assessment of neuromusculoskeletal disorders, St Louis, 1997, Mosby.
In assessing the sagittal diameter of the spinal canal, on a lateral view, the shortest distance from the posterior aspect of the vertebral body to the spinolaminar line is measured. The distance between the posterior aspect of the dens and the posterior cervical line is measured at C1. The ranges for diameter by level are listed in Table 3-5.
TABLE 3-5 ACCEPTED SAGITTAL CANAL DIAMETER OF THE CERVICAL SPINE
| Level | Diameter (mm) Minimum | Maximum |
|---|---|---|
| C1 | 16 | 31 |
| C2 | 14 | 27 |
| C3 | 13 | 23 |
| C4 to C7 | 12 | 22 |
Adapted from Greenstein GM: Clinical assessment of neuromusculoskeletal disorders, St Louis, 1997, Mosby.
BAKODY SIGN
SHOULDER ABDUCTION RELIEF SIGN/TEST—CERVICAL FORAMINAL COMPRESSION TEST
Assessment for Cervical Nerve Root Compression
Comment
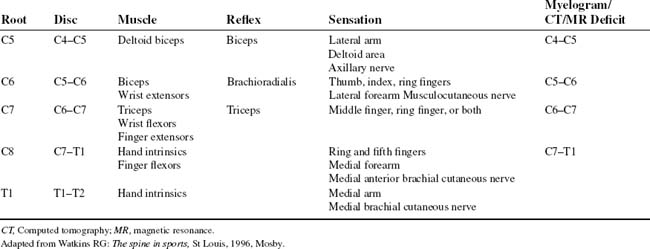
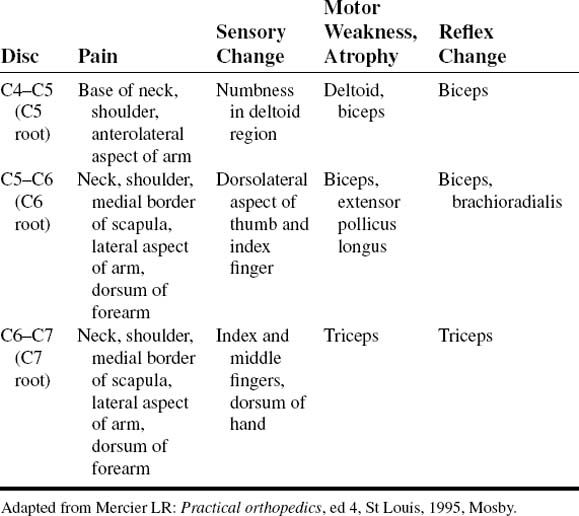
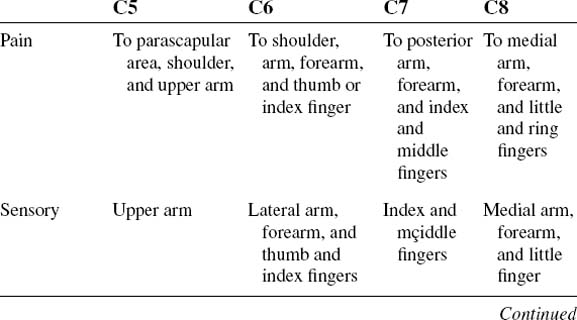
Cervical radiculopathy is more common than cervical myelopathy. Cervical radiculopathy consists of pain and neurologic dysfunction produced by irritation or injury to a spinal nerve. The injury may be caused by a herniated cervical disc, cervical foraminal stenosis, tumors, fractures, or dislocations. The pathognomic characteristic of cervical radiculopathy is pain in the distribution of nerve (Table 3-6).
PROCEDURE
BARRÉ-LIÉOU SIGN
Assessment for Vertebral Artery Syndrome
ORTHOPEDIC GAMUT 3-11 TRAUMA TO THE VERTEBRAL ARTERY
Three areas in which the vertebral artery is most susceptible to trauma:
ORTHOPEDIC GAMUT 3-12 CLASSIFICATION OF LOCKED-IN SYNDROME
Locked-in syndrome is subdivided based on the extent of motor impairment:
ORTHOEPDIC GAMUT 3-13 THE AMERICAN CONGRESS OF REHABILITATION MEDICINE (1995) DEFINITION OF LOCKED-IN SYNDROME
PROCEDURE
PROCEDURE
BRACHIAL PLEXUS TENSION TEST
PROCEDURE
PROCEDURE
DEKLEYN TEST
Assessment for Vertebral Artery Syndrome
ORTHOPEDIC GAMUT 3-16 VERTEBRAL ARTERY PATENCY TESTS
Several variations of the vertebral artery patency tests include:
ORTHOPEDIC GAMUT 3-17 POTENTIAL SITES OF COMPRESSION OR INJURY DURING SPINAL MOVEMENT
PROCEDURE
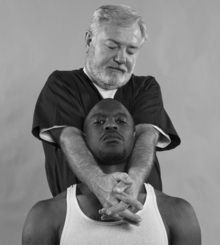
DISTRACTION TEST
Assessment for Cervical Nerve Root Compression, Intervertebral Foraminal Encroachment, and Facet Capsulitis
ORTHOPEDIC GAMUT 3-18 ZYGAPOPHYSEAL JOINT MENISCI
Four distinct types of cervical zygapophyseal joint (Z-joint) menisci exist:
Pain and stiffness may result from weather changes or unexplained causes. Radiculopathy is not always present. Hyporeflexia, motor weakness, and sensory disturbance (especially paresthesia) are common (Table 3-7).
ORTHOPEDIC GAMUT 3-19 INDIRECT SIGNS OF CERVICAL TRAUMA OR INJURY
PROCEDURE
FORAMINAL COMPRESSION TEST
PROCEDURE
HALLPIKE MANEUVER
Assessment for Vertebrobasilar Artery Insufficiency
PROCEDURE
HAUTANT TEST
Assessment for Vertebral Artery Syndrome
ORTHOPEDIC GAMUT 3-22 WALLENBERG SYNDROME
Wallenberg syndrome characteristics:
PROCEDURE
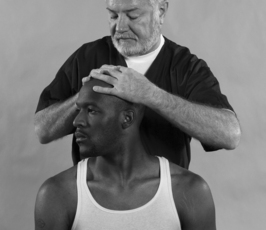
JACKSON COMPRESSION TEST
Assessment for Cervical Nerve Root Compression Resulting from a Space-Occupying Lesion, Subluxation, Inflammatory Edema, Exostosis of Degenerative Joint Disease, Tumor, or Intervertebral Disc Herniation
ORTHOPEDIC GAMUT 3-23 CERVICAL NERVE ROOT COMPRESSION SYNDROME
Clinical axioms regarding cervical nerve root compression syndrome:
Comment
Despite the variability in sensory and motor presentations of cervical radiculopathies, certain classic symptoms and signs exist and are extremely helpful in localizing the compressed root (Table 3-9).
TABLE 3-9 MODIFIED QUEBEC TASK FORCE CLASSIFICATION SYSTEM FOR ACUTE WHIPLASH ASSOCIATED DISORDERS (WAD)
| Proposed Grade | Classification | Physical and Psychological Impairments Present |
|---|---|---|
| WAD 0 |
BPPT, Brachial plexus provocation test; CCFT, cranio-cervical flexion test; GHQ, general health questionnaire; IES, impact of events scale; JPE, joint positioning error; TAMPA, Tampa scale of kinesophobia.
Adapted from Sterling M. A proposed new classification system for whiplash associated disorders—implications for assessment and management, Man Ther 9(2):60-70, 2004.
PROCEDURE
LHERMITTE SIGN
Assessment for Myelopathy of the Cervical Spine
Comment
Peripheral neuropathy is a disorder that affects the peripheral motor, sensory, or autonomic nerves to a variable degree. If only one nerve is affected, mononeuropathy is indicated. If several nerves are involved in a distal symmetric or asymmetric fashion, polyneuropathy is indicated. A patter with multiple, single-peripheral nerves or their branches are involved is considered mononeuritis multiplex (Table 3-10).
TABLE 3-10 CLINICAL SIGNS OF CERVICAL RADICULOPATHY AND MYELOPATHY*
| Cervical Radiculopathy | Myelopathy | |
|---|---|---|
| Muscle wasting | Path, unilateral | Path, bilateral |
| Sensory deficit radicular | Path | Norm |
| Vibratory sense diminished | Norm | Path, lower extremities |
| Muscle stretch reflexes | Path (weak) | Path (hyper) |
| Abdominal reflexes | Norm | Path (absent) |
| Spurling | Path | Norm |
| Babinski sign | Norm | Path |
| Hypertonicity | Norm | Path |
| Gait | Norm | Path |
Norm, Normal; Path, pathologic.
* Classic findings include limitations in cervical range of motion, spasticity (with increased muscle tendon reflexes below the level of canal compromise), a positive Babinski sign, absent abdominal reflexes, decreased joint position and vibratory sensation, and an abnormal gait.
Adapted from Salvi FJ, Jones JC, Weigert BJ: The assessment of cervical myelopathy, Spine J 6(6, suppl 1):S182-S189, 2006.
PROCEDURE
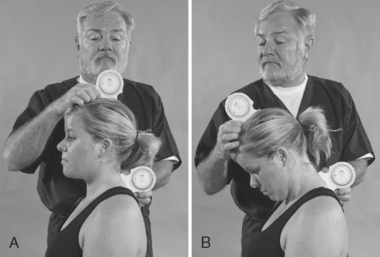
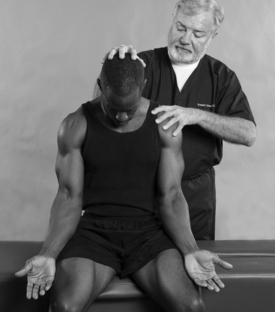
MAXIMUM CERVICAL COMPRESSION TEST
ASSESSMENT FOR CERVICAL NERVE ROOT SYNDROME OR FACET SYNDROME (CONCAVE TESTING) AND CERVICAL MUSCULAR STRAIN (CONVEX TESTING)
Comment
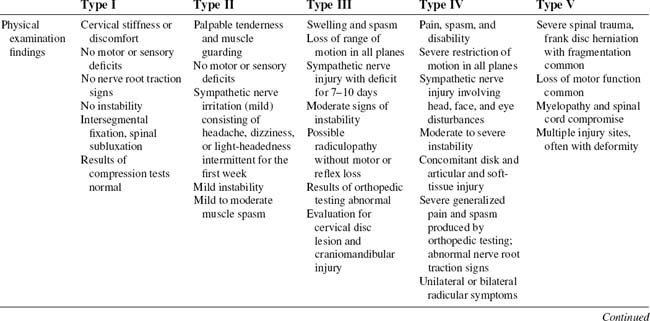
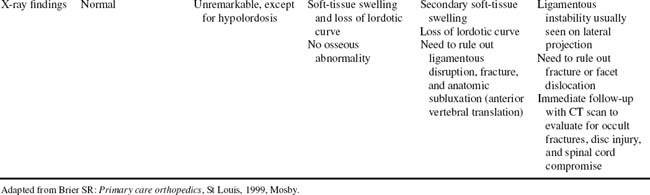
The vulnerability to injury of the cervical region is so great that even low- to moderate-intensity trauma can compromise a multitude of systems. As a result, a variety of signs and symptoms may develop. As is known, the secondary effects of whiplash are sometimes as disabling, if not more so, than the soreness and muscular stiffness of the initial symptoms (Table 3-11).
TABLE 3-11 SYMPTOMS EXPERIENCED WITH CERVICAL ACCELERATION-DECELERATION SYNDROMES
| Symptom | Lesion Site |
|---|---|
| Headache | Suboccipital muscles, greater occipital nerve, myofascial trigger points, facet point irritation |
| Disorientation, irritability | Brain |
| Visual disturbances | Vertebrobasilar artery network, brainstem, cervical spinal cord |
| Memory and concentration disturbances | Brain |
| Vertigo | Cervical sympathetic nerves, vertebral artery, inner ear |
| Arm and hand numbness | Brachial plexus, scalenes |
| Thumb, index finger, middle finger numbness; weakness; temperature changes | Median nerve, carpal tunnel |
| Difficulty swallowing | Pharynx |
| Ringing in ears | Temporomandibular joint, vertebral and basilar arteries, cervical sympathetic chain, inner ear |
| Dizziness, light-headedness | Cervical sympathetic nerves, brain, inner ear |
| Neck and shoulder pain | Paravertebral muscles, apophyseal joints, cervical nerve roots, cervical disc |
| Poor balance, proprioception, and posture | Inner ear |
Adapted from Brier SR: Primary care orthopedics, St Louis, 1999, Mosby.
ORTHOPEDIC GAMUT 3-27 MYOFASCIAL INVOLVEMENT
Two common areas of myofascial involvement of the cervical spine are:
ORTHOPEDIC GAMUT 3-28 TESTS OF DIFFERENTIATION
PROCEDURE
PROCEDURE
O’DONOGHUE MANEUVER
Assessment for Cervical Muscular Strain (Isometric) and Cervical Ligamentous Sprain (Passive Range of Motion)
Comment
Most patients with cervical strain complain of paraspinal muscular aches and stiffness that may extend as far cephalad as the suboccipital region (Table 3-12). Chronic muscular strain of the cervical spine can affect distant organ systems. Pain may be referred to the head, orbits, or scapula.
| Physical examination findings |
Adapted from Brier SR: Primary care orthopedics, St Louis, 1999, Mosby.
ORTHOPEDIC GAMUT 3-29 CERVICAL SPINE MUSCULAR INJURY
The mechanism of cervical spine muscular injury is usually one of the following:
ORTHOPEDIC GAMUT 3-30 STRAINS
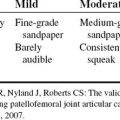
Strains are divided into three categories according to the degree of muscle tissue damage:
ORTHOPEDIC GAMUT 3-31 SPRAINS
Sprains are divided into four categories according to the severity of the ligamentous injury:
ORTHOPEDIC GAMUT 3-32 CERVICAL ACCELERATION-DECELERATION INJURY
Five types of cervical acceleration-deceleration injury:
Separating various grades of cervical whiplash injury is possible according to the degree of external trauma, orthopedic, and neurologic findings, as well as patient disability (Table 3-13).
PROCEDURE
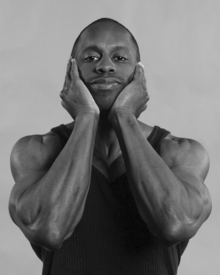
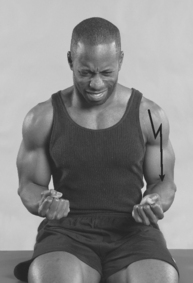
RUST SIGN
Assessment for Severe Cervical Spine Sprain, Upper Cervical Rheumatoid Arthritis, Upper Cervical Spine Fracture, and Severe Upper Cervical Spine Subluxation
ORTHOPEDIC GAMUT 3-33 ODONTOID PROCESS FRACTURES
The Anderson/D’Alonzo classification of odontoid process fractures:
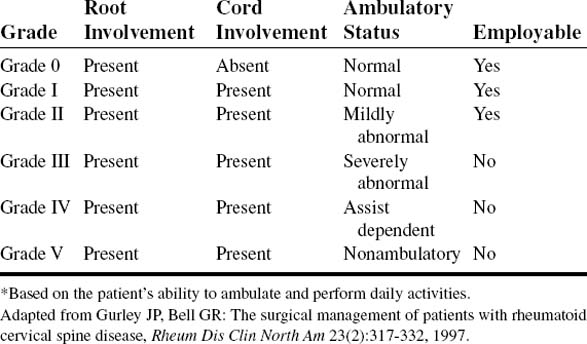
Comment
Atlantoaxial subluxation is the most common and significant manifestation of rheumatoid involvement of the cervical spine. Long duration of disease, advanced patient age, and peripheral joint erosive instability are associated with more common and severe C1–C2 instabilities, affecting the activities of daily living (Tables 3-14 and 3-15).
PROCEDURE
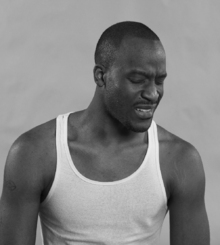
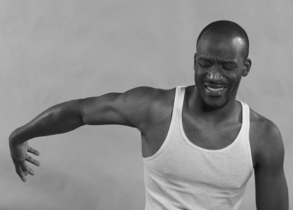
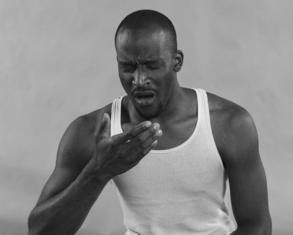
If the patient spontaneously grasps the head with both hands when lying down or when arising from a recumbent position, this action is a positive sign that indicates severe sprain, rheumatoid arthritis, fracture, or severe cervical subluxation (Figs. 3-29 and 3-30).
SHOULDER DEPRESSION TEST
PROCEDURE
SOTO-HALL SIGN
PROCEDURE
SPINAL PERCUSSION TEST
Assessment for Osseous or Soft-Tissue Injury
ORTHOPEDIC GAMUT 3-39 ATLANTOAXIAL INJURIES
The radiographic signs of atlantoaxial injuries are often subtle:
ORTHOPEDIC GAMUT 3-40 CERVICAL SPINE FLEXION-EXTENSION RADIOGRAPHS
The following are prerequisites for cervical spine flexion-extension radiographs:
Comment
Pain or discomfort that is nonarticular may be myofascial in origin. The patient with myofascial pain typically has multiple sites of trigger points that refer pain to a distant site (Table 3-16).
TABLE 3-16 REFERRAL ZONES ASSOCIATED WITH TRIGGER POINTS IN MYOFASCIAL PAIN SYNDROME
| Localized Trigger Points | Referral Zone |
|---|---|
| Suboccipital muscles |
From Brier SR: Primary care orthopedics, St Louis, 1999, Mosby.
PROCEDURE
SPURLING TEST
Assessment for Cervical Nerve Root Compression Syndrome
Comment
All patients who sustain sufficient injury to the cervical spine to make the examiner suspect cervical disc compromise should have a standard three-view, plain-film X-ray film series (Table 3-17).
| Type | Acute Herniated Cervical Disc | Chronic Degenerative Disc Disease |
|---|---|---|
| Physical examination findings |
Adapted from Brier SR: Primary care orthopedics, St Louis, 1999, Mosby.
PROCEDURE
PROCEDURE
UNDERBURG TEST
Assessment for Vertebrobasilar Artery Syndrome
ORTHOPEDIC GAMUT 3-42 BRAINSTEM ISCHEMIA
In vertebrobasilar artery insufficiency, brainstem ischemia is the result of:
ORTHOPEDIC GAMUT 3-43 ARTERIAL WALL (INTIMAL) DAMAGE
In vertebrobasilar syndrome, damage to the artery wall is the result of:
ORTHOPEDIC GAMUT 3-44 VASOSPASM
Arterial wall intimal trauma producing vasospasm follows Virchow triad:
PROCEDURE
VALSALVA MANEUVER—NEURO-ORTHOPEDIC APPLICATION
Assessment for Space-Occupying Lesion, Tumor, Intervertebral Disc Herniation, or Osteophytes
ORTHOPEDIC GAMUT 3-45 CERVICAL SPINE SPONDYLOSIS
Assessment of cervical spine spondylosis includes the following:
PROCEDURE
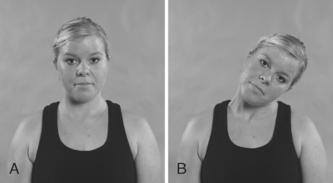
VERTEBROBASILAR ARTERY FUNCTIONAL MANEUVER
Assessment for Vertebral, Basilar, or Carotid Artery Stenosis or Compression
ORTHOPEDIC GAMUT 3-47 VERTEBROBASILAR INSUFFICIENCY
The major signs and symptoms of vertebrobasilar insufficiency are as follows:
ORTHOPEDIC GAMUT 3-48 DIFFERENTIAL DIAGNOSES OF FACIAL PURPURA
ORTHOPEDIC GAMUT 3-49 VERTEBROBASILAR ISCHEMIA
Three types of vertebrobasilar ischemia are: