CHAPTER 59 Cervical Radicular Pain: Injection Procedures
INTRODUCTION
This chapter will review the literature pertaining to the use of epidural space steroid injection (ESI) in the treatment of cervical radicular pain. Epidural injections are utilized to introduce corticosteroid and anesthetic to the epidural compartment and the suspected site of neural injury. There is a plethora of literature describing ESI in the treatment of lumbar radicular and axial pain, and this topic will be comprehensively addressed in a dedicated chapter of this text. Injection therapy has found a particular role in the treatment of lumbar radiculopathy, as a growing body of literature has supported a biochemical and inflammatory injury component in the case of lumbar radicular disorders.1–5 Recent prospective uncontrolled6–9 and controlled lumbar studies10–12 have suggested a significant beneficial response when transforaminal epidural steroid injections (TFESI) are utilized in the treatment of radiculopathy.
While the role of inflammation in the injury process of cervical radiculopathy has largely been extrapolated from this lumbar literature base, several studies have similarly highlighted the biochemical processes likely at play in cervical radicular disorders. In a study of cervical disc specimens removed during discectomy for radiculopathy,13 when compared to control disc samples, significant increases in matrix metalloproteinase, nitric oxide, prostaglandin E2, and interleukin-6 were observed. A later study by this same author14 revealed herniated cervical disc specimens to be biologically responsive with resultant increased levels of nitric oxide, interleukin-6, and prostaglandin E2 when exposed to interleukin-1β. A more recent immunohistochemical investigation of herniated cervical intervertebral discs15 has revealed the presence of inflammatory processes and neovascularization, increased levels of matrix metalloproteinase, and a marked increase in nitric oxide production when compared to control samples.
Similar to the lumbar literature, which has revealed abnormal radiographs and compressive lesions in asymptomatic individuals,16–18 studies of the cervical spine also reveal abnormal radiographic findings in patients without cervical pain or symptoms of radiculopathy.17,19,20 In a cervical MRI study of asymptomatic patients,19 20% of subjects over 40 years of age were observed to have foraminal stenosis, and 10% of cases under 40 years of age revealed a herniated disc. In an earlier study of asymptomatic subjects employing cervical myelography,17 21% of cases were observed to have nerve root filling defects. These significant radiographic and potentially compressive findings in asymptomatic individuals suggest that a purely mechanical injury construct is too simplistic.
Also, parallel to the lumbar radiographic literature,21–24 which has revealed regression of symptomatic disc lesions with a tendency for symptoms to improve prior to radiographic regression, cervical studies have demonstrated a regression of symptomatic cervical disc pathology.25–27 Both CT26 and MRI25,27 studies have revealed the largest disc herniations to reduce most in size. In greater than 75% of cases a 35–100% size reduction in disc lesions has been observed, and a greater likelihood of resolution is realized in cases of disc extrusion. In combination, these cervical-specific biochemical and radiographic studies set the stage for a mechanochemical injury construct in cases of cervical radiculopathy. It is the biochemical or inflammatory component of neural injury that is the intended target of ESI therapy. The remainder of this chapter will review the available literature addressing this treatment approach in cervical radicular disorders.
BACKGROUND LITERATURE
Similar to lumbar ESI, injections to the cervical spine can be performed through either an interlaminar or transforaminal approach. During the performance of interlaminar injections, medication is most reliably placed in the epidural space with the use of fluoroscopic guidance. This fact has been established in the lumbar spine injection literature. White28 revealed a 25% miss rate when interlaminar injections were performed by an experienced anesthesiologist without the use of fluoroscopy. The inaccuracy of cervical interlaminar injections performed without guidance has more recently been reported.29 In this multicenter retrospective analysis, a first-attempt miss rate of 53% was observed when the typical loss of resistance technique was utilized. When medication was successfully introduced to the epidural space, ventral spread of medication was observed in only 28%. While interlaminar ESI can be performed with technical success, particularly with the use of fluoroscopic guidance, there are anatomic advantages to performing ESI through a transforaminal approach.30 With interlaminar injections, medication is typically deposited dorsally, posterior to the thecal sac. The spinal pathology that serves as the intended target of ESI is typically located in the ventral spinal canal. TFESI provides the interventionist an opportunity to better control the flow of injectant and target the specific level of segmental pathology. In addition, and of particular importance in the cervical spine, the transforaminal injection approach allows for foraminal and extraforaminal spread of medication. The complexity of the cervical anatomy requires fluoroscopic guidance if TFESI is to be performed.
In addition, and similar to ESI in the lumbar spine, the use of fluoroscopic guidance and contrast enhancement allows the interventionist to avoid vascular uptake, which would prevent the successful placement of medication at the injury site. Indeed, this is a significant issue for two reasons. The general notion is that a local instillation of glucocorticoid provides greater benefit than using an oral or parenteral route. If the medication is infused intravascularly, this proposed benefit will be obviated. A second and potentially more important reason to avoid intravascular uptake is the possibility of inadvertent arterial injection with resultant neural injury. Such complications will be further reviewed in the concluding section of this chapter. Several studies underscore the importance of using fluoroscopy during spinal injection procedures. An 11.2% incidence of venous uptake has been observed by fluoroscopy during lumbar TFESI, necessitating needle repositioning to achieve a satisfactory epidurogram.31 An earlier study of fluoroscopically guided lumbar injections32 revealed a 10.9% and 10.8% incidence of vascular uptake during transforaminal and caudal injections, respectively, compared with a 1.9% incidence when utilizing an interlaminar approach. In a prospective study of 337 cervical TFESI,33 the overall rate of fluoroscopically visualized venous uptake was 19.4%. Observation of blood in the hub of the injection needle was determined to be unreliable in the detection of vascular uptake, with a 97% specificity but only a 45.9% sensitivity observed. These studies highlight the role of fluoroscopic visualization as the only reliable means of observing venous uptake, as the sensitivity of blood observed in the spinal injection needle or tubing is unacceptably poor.
While the majority of background literature addressing cervical ESI describes an interlaminar injection approach, performed with and without fluoroscopic guidance, more recent clinical studies employ fluoroscopically guided TFESI. While there is an apparent trend for more recent cervical literature to describe a transforaminal (TF) approach, there remains a wide discrepancy in cervical injection techniques employed by the interventional spine community. A recent national survey of anesthesia practices found that fluoroscopic guidance is employed during cervical ESI in 73% of private practices but in only 39% of academic institutions.34 Similarly, TFESI was more likely to be employed by 61% of private practices but only 15% of academic centers.
INTERLAMINAR INJECTION LITERATURE
Cervical ESI clinical outcome studies have been published, but the body of literature is not as vast as that addressing lumbar ESI. To date, the overwhelming majority of these studies are uncontrolled and retrospective. The introduction of cervical epidural injections initially arose as a result of the described successes in treating lumbar axial and radicular pain with epidural injections of corticosteroid. The earliest reference to cervical epidural injection therapy was in a 1972 study describing the role of intra- and extradural corticosteroids.35 In the 1980s, several studies reported clinical outcomes following cervical epidural injection therapy.36–40 These studies included patients with a variety of clinical presentations including radiculopathy, cervical pain, reflex sympathetic dystrophy, postherpetic neuralgia, and viral brachial plexitis. Three uncontrolled studies published in 1986 which included a total of 180 patients describe a combined result of greater than 90% pain relief in 20–24% of patients and little to no response in 12–24% of cases.37–40 In these studies, an interlaminar injection approach was performed without fluoroscopic guidance. In one of these studies38 that retrospectively analyzed 25 patients receiving an average of 1.5 injections, patients with superior outcomes were more likely to present with radicular pain and sensorimotor deficits on examination. In a 1988 study41 of 16 patients presenting with suspected cervical radicular symptoms without a radiographic correlate, up to three blind interlaminar ESI were performed. After 1 year and questionnaire follow-up, 12 patients described their pain as improved and 50% of those patients with initial neurological deficits reported improvement in these symptoms. Additional outcome studies published in the 1990s36,40,42 describe approximately 40% of 100 combined patients realizing relief of 70% or greater. In one of these studies,36 which included 58 patients followed for 6 months, 41.4% demonstrated an excellent response, defined as greater than 90% pain relief. An excellent outcome was described to be more likely in those patients with radiographic evidence of spondylosis or subacute cervical strains.
A 1993 retrospective analysis of 100 patients43 receiving cervical interlaminar ESI attempted to identify patient characteristics that would serve as reliable predictors of clinical outcome. In each case, a mean of 2.35 injections were performed in a nonfluoroscopically guided (blind) fashion at the level of suspected segmental pathology. Forty-one percent of the total patient population described greater than 50% pain relief and at least a partial return to normal activities at a mean of 14.7 months follow-up. Symptom duration prior to injection and a history of trauma did not prove reliable in predicting clinical outcomes. Older patients and those with radicular pain were observed to realize more lasting pain relief. In this study, patients with a herniated disc or a motor deficit were observed to do worse. Patients with cervical spondylosis or stenosis demonstrated a superior outcome. The authors concluded that patients with clinical radiculopathy or radicular pain were more likely than patients with axial pain alone to realize relief from cervical ESI. Complications in this study included a 2% incidence of dural puncture and 4% incidence of vasovagal events.
In a 1996 study of 26 patients44 treated nonsurgically for cervical radiculopathy associated with a herniated disc, 20 patients demonstrated a good or excellent outcome. Each of these patients was fully satisfied with the outcome and reported little to no residual pain or activity limitation. Nineteen of these 20 successes initially presented with cervical disc extrusion. The outcomes following injection therapy in this study cannot be presented with any certainty, as only nine of these patients received a single fluoroscopically guided cervical ESI performed in either an interlaminar or transforaminal fashion. Other nonsurgical treatment approaches employed in this study included relative rest, icing, the use of a cervical collar, nonsteroidal anti-inflammatory agents, and in most cases, an oral corticosteroid taper. Similarly, in a frequently referenced 1999 study45 which prospectively studied 246 patients nonrandomly assigned to either conservative or surgical treatment for cervical radiculopathy, cervical injection therapy was employed in the conservative care group. Spinal injections employed were described as nerve blocks, ESI, or facet blocks. The body of the paper suggests that injections were utilized in 13% of patients, and therefore outcomes following injection therapy in this paper are unclear. In this paper, both groups of patients realized significant improvements in pain and functional status.
DIAGNOSTIC SELECTIVE NERVE ROOT INJECTION
While there are many references alluding to the utility of lumbar diagnostic selective nerve root block (SNRB), performed through a fluoroscopically guided transforaminal approach, the role of diagnostic cervical injections remains poorly defined. The specificity and sensitivity of lumbar diagnostic nerve root injections has been estimated at 87–100%46,47 and 99–100%,48,49 respectively, with corroborative surgical lesions observed. In a study of patients treated with anterior cervical decompression and fusion,50 75 patients demonstrated a positive response to a preoperative diagnostic cervical SNRB. Diagnostic injections were performed with fluoroscopic guidance, contrast enhancement, and 1 cc of 1% lidocaine. The study describes 65 of 75 patients realizing immediate postoperative relief during a recovery room assessment. In a more recent report,51 the preoperative diagnostic utility of lumbar and cervical selective nerve root injections has similarly been assessed. In this study, 101 patients were included, but only 18 were cervical patients. Nerve root localization was confirmed with both contrast enhancement and symptom provocation utilizing a nerve root stimulator. Anesthetization was performed utilizing 0.5–0.75 cc of 2% lidocaine. A 90% reduction in symptoms during the postinjection assessment was considered a positive response. Of those patients who underwent surgery with a positive preoperative diagnostic injection, 91% reported a successful surgical outcome. Of the 10 patients who demonstrated a negative response to preoperative injection, 60% reported a successful surgical outcome. This difference in outcomes was statistically significant (p=0.05).
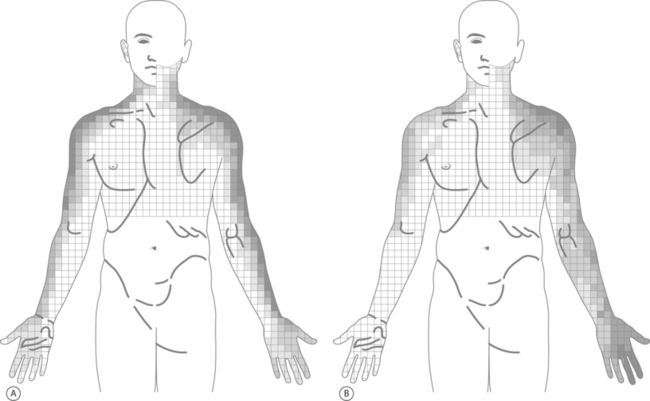
In a novel study,52 the symptoms resulting from cervical nerve root provocation during diagnostic SNRB were recorded and dynatomal maps described. In this study, 87 patients underwent 134 cervical nerve root stimulations. The C4 through C8 nerve roots were studied and symptom distributions recorded utilizing more than 1000 bits of data compiled upon a 793-body-sector bit map containing 43 clinically relevant body regions. The resultant dynatomal maps differed considerably from the classic cervical dermatomes described by Foerster53 and Keegan and Garrett.54 Highlights from the dynatomal maps include C5 root stimulation resulting in symptoms radiating as distal as the forearm in only 14%, C6 symptoms incorporating the ulnar hand and fifth digit in 37% and 30%, respectively, C7 symptoms uniquely referred to the anterior head and to the chest as frequently (17%) as to the middle finger, and C8 symptoms extending to the thumb as often as digit five (Fig. 59.1). As the authors explain, these differences between the dynatomal maps and more classically described dermatomal distributions likely arise in part from limitations in the more classic studies’ methodology, the more frequent existence of cervical intrathecal anastomoses,55,56 and varying nerve root contributions to the brachial plexus.
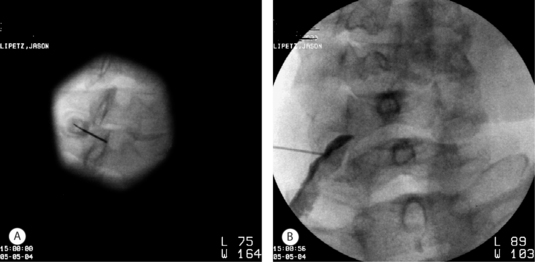
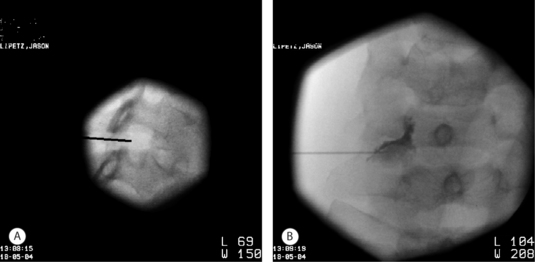
In the author’s practice, diagnostic cervical SNRB are employed when diagnostic uncertainty remains. As described later in this chapter, the level of segmental pathology is often clarified through a review of radiographs and a detailed physical examination. In those cases in which diagnostic uncertainty remains, electrodiagnostic studies can be utilized. When electrodiagnostic studies fail to confirm a level of segmental pathology, SNRB can be utilized in an effort to more definitively identify the pain generator. In the cervical spine in particular, where dynatomal overlap is more frequently observed, the clinician needs to be cautious in assigning a level of radicular involvement when the physical examination and radiographs are not clearly corroborative. In other cases, radicular pain may be clinically suspect, but a radiographic correlate is not appreciated, i.e. following whiplash or in the setting of a chemical radiculitis. In such instances, diagnostic SNRB are employed. It is the author’s goal during diagnostic injections to achieve a contrast pattern which reveals the exiting nerve root and dorsal root ganglion without epidural spread to adjacent levels. This can often best be achieved by positioning the spinal needle adjacent the posteriorly situated superior articular process but with a more inferior and lateral position in the foramen (Fig. 59.2). Anesthetization is performed with 0.8–1.0cc of 2% lidocaine. The patient’s response to diagnostic injection is considered positive if an 80% symptomatic reduction is realized during the postinjection assessment performed approximately 20 minutes after injection. Pain ratings and diagrams are completed before and after injection, and typically provocative maneuvers are performed during the assessment phase.
TRANSFORAMINAL INJECTION LITERATURE AND DIAGNOSTIC SUBSETS
A 1996 prospective uncontrolled study of 68 consecutive cervical radiculopathy patients reported outcomes following injection therapy.57 Each patient described radicular pain that radiated at least as distally as the forearm. All patients except for one presented with an associated neurologic deficit in the form of either reduced strength, sensation, or a diminished reflex. The average duration of symptoms was approximately 2 months. All but one patient demonstrated a radiographic finding which was believed to correlate with symptoms. In 70% of cases a corroborative intervertebral disc protrusion or herniation was described, and in 30% spondylotic foraminal encroachment was observed. The patients in this study were treated with three possible injection techniques. Initially, a cervical or brachial plexus block was performed using anatomic landmarks without image guidance. If this injection technique proved helpful, it was repeated. Otherwise, a fluoroscopically guided contrast enhanced TFESI was performed. Once again, if this approach proved helpful it was repeated. If this failed to offer relief, a fluoroscopically guided interlaminar ESI was performed. Each patient received an average of 2.5 injections, and in 62% of cases a TFESI was employed. Twenty-nine percent improved with the plexus block approach and 16% received interlaminar injections. No complications were reported in this study. The average time to clinical discharge in this study was 7 months. At that time an average VAS of 0.6 was recorded, all patients had returned to work, and partial or full neurologic recovery was described in 47% and 46%, respectively. An additional phone interview was conducted with 93% of patients at an average of 39 months following treatment. By this survey, 76% of patients were pain free and the other 24% reported an average pain score of 2/10. Eighty-six percent reported an absence of parasthesias, and 73% reported no residual weakness. No patient required surgical intervention. In addition to these described clinical outcomes, the authors share an interesting observation in the discussion section of their paper. This same group of investigators performed a study with similar methodology and interventions in the treatment of patients with lumbar radiculopathy.58 In that study, 14% of patients ultimately required surgical intervention, leading the authors to speculate that the prognosis for recovery following injection therapy might be more favorable for the cervical radiculopathy population.
In a 2001 prospective study of 32 patients with cervical radiculopathy,59 fluoroscopically guided TFESI were similarly employed. Inclusion criteria included a persistence of symptoms for at least 2 months, high radicular pain scores on a 10 point scale, and a radiographic correlate such as a focal disc lesion or degenerative foraminal stenosis. In 26 of 32 cases, spondylosis was described rather than a disc herniation. Injections were performed in the seated position and with fluoroscopic guidance but without contrast enhancement. Patients were clinically followed for 6 months. In 27 of the 34 levels treated only one injection was performed, and in the remaining seven, a second injection was administered. At 6-month follow-up, a good or excellent result, defined as at least 50% pain relief and requiring little to no medical treatment, was observed in 56% of patients. No long-term complications were reported. These outcomes are inferior to those described by the previous 68 patient study in which no patients described ongoing debilitating pain. There are several differences between these studies in methodology and patient populations. First, the majority of the patients in this study presented with radiculopathy suspected as arising from corroborative degenerative foraminal stenosis as opposed to a herniated disc. Additionally, contrast enhancement was not utilized during injections, and repeat injections were not employed in the majority of cases.
Transforaminal injections performed with CT guidance have been utilized in a retrospective study of 30 patients presenting with cervical radiculopathy.60 In this study, 16 patients presented with suspected corroborative degenerative foraminal stenosis and 14 with a focal disc protrusion. Patients were excluded if a strength deficit was evident. The average symptom duration prior to injection therapy was 2.7 months. Patients were evaluated at 2 weeks and 6 months after injection therapy and the pain response was assessed. Injection procedures were performed with CT guidance and contrast enhancement. The mean visual analog score prior to injection therapy was 6.5, and this was significantly reduced (p<0.001) to 3.3 at 2 weeks after the injection procedure. An outcome of excellent was assigned to those with greater than 75% pain relief and good for those with at least a 50% pain reduction. Eighteen patients realized a good or excellent outcome 2 weeks after the first injection and this was sustained at 6 months without further injection therapy. Only 3 of 12 patients who realized an initial fair or poor outcome received a second injection. Two of these patients realized excellent outcomes that were sustained at the 6-month follow-up. Initial pain intensity, symptom duration, and radiographic correlates were not found to reliably predict clinical outcomes. No procedural complications were reported.
In an additional study of CT-guided transforaminal injection therapy for radicular pain,61 outcomes of 160 patients were retrospectively analyzed. In 18 of these cases, patients presented with cervical radicular pain. The remainder of the patients were treated for symptoms of thoracic or lumbar origin. Patients presented with variable radiographic correlates in this study, including degenerative foraminal stenosis, disc herniation, postoperative fibrosus, or no visible radiographic abnormalities. The majority of patients, approximately 80%, received only a single injection. Eleven of these 18 patients (61%) realized symptomatic improvement, and it is extrapolated from the data that in 80% of these cases a greater than 50% reduction in radicular pain was realized. It would also appear after a review of this report that approximately 66% of those cases with improvement demonstrated sustained relief by phone interview at a mean of 110 days following treatment. For the study group as a whole, there was no apparent correlation between radiographic findings at the symptomatic level and outcomes. There was a suggestion of greater efficacy of injections for cervical patients, in which 57.9% of injections were categorized as effective, when compared to thoracic and lumbar patients, in which a 50% and 48% efficacy were assigned, respectively.
In an effort to assess outcomes following cervical TFESI in a more diagnosis-specific fashion, the author’s research group retrospectively analyzed the data in three separate studies.62–64 The first of these three studies62 included 20 subjects with cervical radicular pain arising from atraumatic spondylotic foraminal stenosis. Each patient presented with radiographic evidence of foraminal stenosis at the symptomatic level. A diagnosis of level-specific radiculopathy was confirmed either by a corroborative myotomal strength deficit or reflex abnormality, electrodiagnostic evidence of myotomal denervation, or a positive response to a confirmatory diagnostic SNRB. Patients’ average symptom duration prior to treatment was 5.8 months. At initial presentation, the average VAS was 6.9. Follow-up data collection was performed by an independent reviewer by phone interview at an average of 21.2 months. An average of 2.2 injections was performed in each case. At the time of follow-up, six patients (30%) had proceeded with surgical decompression. An overall good or excellent result was described by 12 patients (60%). To be categorized as a good or excellent outcome, patients needed to demonstrate a pain score of four or less on a ten point scale, be working full time, utilizing no more than prescription NSAIDs to control pain, and demonstrate high patient satisfaction scores. The average recorded verbal pain score at the time of follow-up was 2.0. A significant improvement (p=0.001) in the average pain score was observed. A significant reduction (p=0.0005) in medication usage was also observed at the time of follow-up. At follow-up, only one patient was requiring opioid analgesics and nearly 86% were utilizing no medications or over-the-counter agents. An analysis of patient characteristics at initial presentation, including associated weakness and distal extent of radicular pain, did not predict clinical outcomes with statistical significance. A significant relationship was noted between patient age and satisfaction with treatment, with younger patients providing the highest patient satisfaction scores (p=0.0047).
In the second and third published studies, patients with a traumatic symptomatic onset were described. In the second paper,63 the efficacy of cervical TFESI was retrospectively analyzed in 22 patients who presented with radicular pain following a whiplash event and whose imaging did not reveal a radiographic correlate at the symptomatic level. In this study, patients were excluded if their examination revealed a strength or reflex abnormality or if electrodiagnostic studies revealed denervation. Each patient demonstrated an initial positive response to a diagnostic SNRB to confirm the symptomatic level. Patients’ average symptom duration prior to diagnostic injection was 6 months. Follow-up data were collected by phone interview at an average of 33 weeks after the final therapeutic injection. Outcome categorization was based upon a consideration of work status, medication use, and Oswestry scores. An overall 14% good or excellent outcome was observed. To be labeled good or excellent, the patient was required to be working at least full time with modifications, utilizing no more than prescription NSAIDs for pain control, and demonstrate an Oswestry score of 21–40, suggestive of more ‘moderate’ disability. When considering patient stratification before and following treatment, a significant change was not observed. In patients with initial higher levels of function, a more pronounced pain reduction was reported at the time of follow-up.
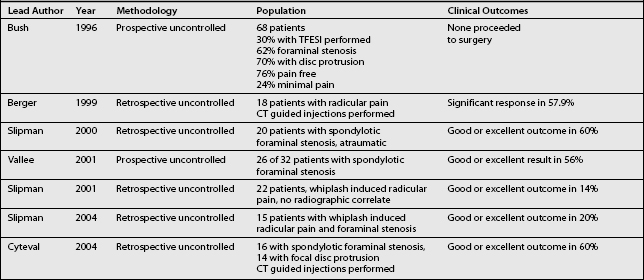
The third64 of these three studies similarly investigated patients with a traumatic symptomatic onset but with radiographs revealing degenerative foraminal stenosis at the symptomatic level. This study included 15 patients presenting with a median symptom duration of 13 months. The symptomatic level was determined by the presence of a corroborative strength deficit or reflex abnormality, electrodiagnostic evidence of myotomal denervation, or a positive response to a diagnostic SNRB. An average of 3.7 injections was performed at each symptomatic level, and follow-up data were collected by phone interview at an average of 20.7 months following treatment. Similar to the first of these three studies, outcomes were determined through a consideration of work status, pain scores, medication use, and patient satisfaction. While a significant reduction (p=0.0313) in pain scores was observed, an overall good or excellent outcome was observed in only 20%. Six patients underwent surgery, and only one of these realized a good or excellent postoperative outcome. The outcomes from these three studies as well as the previous cervical TFESI studies described in this chapter are summarized in Table 59.1.
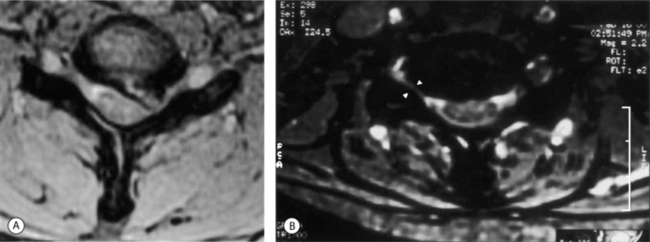
In this author’s practice, transforaminal injections are employed for patients with cervical radicular pain and radiculopathy. Often, prior to injection therapy, patients have failed trials of nonsteroidal anti-inflammatory agents and analgesics, physical therapy, oral corticosteroids, and interlaminar epidural injections performed with or without fluoroscopic guidance. In other cases in which the patient presents with a more painful or pronounced radiculopathy, transforaminal injections are introduced earlier in the treatment algorithm. The algorithmic approach to the patient with cervical radicular pain is comprehensively addressed in Chapter 57 by Dr. Zacharia Isaac and Curtis Slipman and will only be touched upon here. An important guiding principle is that prior to performing a therapeutic transforaminal injection, the level of segmental pathology is confirmed. Intuitively, this is an appealing notion as the purpose of the injection is to deliver the therapeutic substance as close to the site of pathology as possible. Devoting the time required and employing the appropriate diagnostic modalities to the identification of the proper target is a necessary component of providing the best possible treatment. The level of nerve root involvement is typically confirmed in one of three ways. The patient can present with radiographs revealing of a focal compressive lesion, i.e. disc protrusion or degenerative foraminal stenosis (Fig. 59.3), and a corroborative myotomal strength deficit or reflex abnormality. In cases in which radicular pain is suspect, but the exam remains intact and imaging less conclusive, i.e. multilevel foraminal compromise, electrodiagnostic studies can be employed to confirm the level of pathology. If such testing also does not prove to be diagnostic, diagnostic SNRB offers a third means of confirming the level of involvement. In those cases in which the patient presents with a history and examination consistent with cervical radicular pain, a normal neurologic exam, and a highly corroborative radiograph, i.e. single-level disc extrusion with pronounced foraminal compromise and nerve root compression, the level of pathology is also appropriately assigned. Therapeutic injections are typically performed 2 weeks apart with a reevaluation scheduled 2 weeks after the second injection. In those cases in which patients present with more debilitating pain, the first two injections can be performed at 1-week intervals. If progress is realized after the initial two injections, a third is scheduled. If pain relief is complete after one or two injections, no further injections are performed. A fourth and final injection is reserved for those patients with sustained and incremental, but incomplete, relief after the initial three. Patients with successful therapeutic outcomes typically receive between two and three injections. This is in agreement with the lumbar6,10 and cervical57,62 injection literature describing superior clinical outcomes. While observed clinically, it is atypical for the cervical radiculopathy patient to realize complete lasting relief after the first injection. The author questions whether recently published cervical59,60 and lumbar65 TFESI studies describing inferior outcomes have done so, in part, as a result of terminating treatment after a single injection rather than offering a series of injections in accordance with the patient’s clinical response. Injections are typically performed in conjunction with a diagnosis-specific physical therapy regimen coordinated by an experienced mechanical therapist. During therapy, an emphasis is placed upon symptom centralization and strengthening of the myotomal strength deficit.
The author’s experience is in agreement with the cervical injection literature in that patients with radicular pain arising from degenerative foraminal stenosis are often successfully treated with injection therapy, but are more likely to have persistent or recurrent symptoms than the patient with an acute discogenic radiculopathy. This contradicts findings of interlaminar ESI papers36,43 that suggest superior outcomes in the setting of degenerative spondylosis. The 60% success rate described for patients with spondylotic radicular pain is essentially in agreement with the author’s clinical experience. In those patients with persistent spondylotic radicular pain, it would appear that the stenosis serves as an ongoing mechanical stressor less likely to be ameliorated through chemical therapies. Those patients with radicular pain following trauma, i.e. whiplash, without a radiographic correlate may present with the worst prognosis due to an intrinsic and less reversible neural injury following a transient but potentially profound compressive or traction type insult.66 Outcomes in the author’s practice for this challenging population have been poor and have mirrored the data from the author’s whiplash studies.63,64 While one report41 has described more positive outcomes following ESI for patients with cervical radicular pain without a radiographic correlate, these ‘radiculitis’ patients were not described as post-traumatic.
The author would also agree with the observations of other authors suggesting that outcomes following TFESI for patients with acute discogenic cervical radiculopathy are superior to those observed for patients with lumbar radiculopathy.57,61 Controlled studies of lumbar transforaminal injection therapy for mixed patient populations with stenotic and discogenic radiculopathy suggests a 71–84% success rate.10,12 The author’s experience with patients presenting with discogenic cervical radiculopathy is consistent with a long-term success rate at the higher end of this range. This also holds true for patients presenting with more severe radicular pain, even when a more pronounced myotomal strength deficit is initially evident. In contrast to43 and in agreement with38 previous interlaminar ESI studies, the author has not found a sensorimotor deficit at initial presentation to portend a worse nonsurgical outcome. In those cases where the extent of weakness presents a greater clinical concern, patients are concurrently evaluated by a surgical associate and their progress more closely followed.
Finally, it will be interesting to see if newer injectable medications are introduced over the coming years. While the current cocktail of corticosteroid and local anesthetic would appear to be effective in treating patients with radicular pain syndromes, basic scientific research has uncovered other potential targets in both the inflammatory cascade67 and the pain generating cycle.68 It will require well-designed and controlled clinical trials to determine if in fact newer agents can offer a more potent and cost-effective means of treating the biochemical injury component of cervical and lumbosacral radiculopathies.
COMPLICATIONS
More minor complications following interlaminar cervical ESI including nausea, vomiting, dizziness, facial flushing, hypotension, and increased cervical pain have been reported.69–71 Complications arising from fluoroscopically guided interlaminar ESI have been described in a retrospective study of 345 injections in 157 consecutive patients.72 Injections were performed at the C6–7 or C7–T1 level utilizing 2 cc of 1% lidocaine and 80 mg of triamcinolone acetonide. Patients were surveyed by telephone 24 hours after injection procedures and asked to complete a standardized questionnaire. Clinical chart notes were also reviewed for the 3-week period following injections. A transient increase in neck pain was described in 6.7%, nonpositional headaches which resolved in 24 hours in 4.6%, insomnia the night of the injection in 1.7%, vasovagal reactions in 1.7%, facial flushing in 1.5%, fever the night of the procedure in 0.3%, and dural puncture in 0.3%. The authors concluded that interlaminar ESI appear to be a safe treatment approach for patients with cervical radiculopathy.
Before proceeding with a discussion focusing on more injection site-specific complications arising from ESI, it should be highlighted that many of the more minor ‘complications’ described actually represent symptoms arising from a transient systemic corticosteroid effect. Insomnia, facial flushing, and nausea69–72 are fairly commonly described in the author’s practice and more notably when less particulate corticosteroid compounds, i.e. betamethasone as opposed to methylprednisolone, are administered. Resultant elevations in blood glucose levels remain a particular concern in diabetics receiving injection therapy. Similarly, and as reported in the literature, persistent hiccups73 and dysphonia74 have been observed on more limited occasion following epidural injection of corticosteroid. The systemic corticosteroid effect which frequently arises after epidural injection by any route raises the possibility that a component of the therapeutic effect realized might similarly arise from a more systemic as opposed to a local process. While this is an issue for further study and consideration, in the author’s experience many patients realize relief through ESI after failing one or two oral corticosteroid tapers. While limited in methodology, a small placebo-controlled study75 comparing oral dexamethasone to placebo in the treatment of lumbosacral radicular pain did not demonstrate a significant therapeutic effect. In this author’s opinion, while the possibility remains that a systemic corticosteroid effect contributes in small part to the therapeutic response following ESI, it can be stated with much greater certainty that these systemic effects contribute to the profile of minor ‘complications’ often observed.
Additional and more serious complications following interlaminar ESI have also been reported. Cases of severe pain suggestive of neural injury following an interlaminar ESI have been described.76,77 In three of these cases, a blind C6–7 approach was complicated by a complex regional pain syndrome (CRPS) affecting the upper extremity contralateral to the symptomatic side in two cases. In these cases, symptoms resolved over a 3-week to 3-month period and were presumed to arise from either spinal cord or nerve root trauma. A 1998 paper69 reports two cases of intrinsic spinal cord damage following interlaminar injection. In each of these cases, intravenous sedation was utilized and the injection was performed with fluoroscopic guidance. In each case the initial injection attempt resulted in suspected subarachnoid placement without a response from the sedated patient. Postprocedural imaging did reveal an abnormal signal within the spinal cord in both cases. In the first case, the patient was left with symptoms consistent with an iatrogenic right C7 radiculopathy and paresthesias affecting the bilateral lower extremities. In the second case, the patient suffered from a severe left upper extremity CRPS and paresthesias affecting the right thigh. Epidural abscess,78 epidural hematoma,30,79–81 and subdural hematoma82 have similarly been described as complications arising from interlaminar cervical ESI. In several of these cases, the patients required emergent cervical laminectomy and decompression for progressive neurologic deterioration. In two of these cases, a postoperative return to neurologic baseline is reported,78,79 and in another82 the patient succumbed to cardiac arrest following an acute meningitis.
Complications following cervical TFESI have been highlighted in the more recent literature. Complications associated with both cervical and lumbar TFESI have been reported in a prospective, nonrandomized, controlled study.83 In this paper, 151 patients received 306 transforaminal injections. Concurrently, 60 patients who were evaluated, but who did not receive injection therapy served as the control group. Side effects and complications were recorded by an independent reviewer through patient questionnaires completed immediately following, at 1 week, and 3 months following each injection. The control group also completed the same questionnaire on one occasion. In this study, 37 patients received 89 cervical TFESI. Ninety-one percent of the study group as a whole described no complications or side effects during the injection procedure. Light headedness was reported by 2.2% of patients, nausea by 1.1%, and dural puncture was also suspected in 1.1%. Immediately following cervical injection procedures, 22.7% reported increased pain at the injection site, 18.2% described increased radicular pain, 13.6% light headedness, 9.1% increased axial pain, 4.5 % non-specific headache, and 3.4% nausea. At the 1-week interview there was no difference in reporting between the cervical injection patients and the control group except for increased pain at the injection site which was reported in 30.3% of injection patients. At 3 months, two patients reported increased neck pain and one reported heartburn and fluid retention. Of the two patients with increased neck pain, one stated that he or she would not repeat the injection when considering the outcome. No patients in the study group reported more serious complications.
Complications associated with fluoroscopically guided cervical TFESI have also been reported in a retrospective fashion.84 In this study, a total of 357 injections were performed. Fluoroscopically guided contrast-enhanced injections were performed utilizing 1–2 cc of 1% lidocaine and 6–12 mg of betamethasone. Charts were reviewed from the time of injection for as long as 3 years following treatment to identify complications. Two complications were reported. In one case, a patient lost consciousness for 2 minutes, followed by 2 hours of nausea and vomiting which then resolved. In the second case, the patient reported a headache and cervical stiffness that persisted for 3 months following the injection with a subsequent complete resolution. These authors concluded that cervical TFESI are a relatively safe treatment option. As this study was retrospective in nature, the possibility remains that additional complications, and in particular those of a short-term nature, were experienced but not recorded through a more comprehensive and ongoing process of patient inquiry.
A more recent retrospective review85 describes the complications associated with 1036 cervical TFESI performed over a 4-year period. In this report, no catastrophic neurologic events are described. Seventeen minor complications (1.64%) including dizziness, numbness, pain, transient weakness, and one case of transient global amnesia were described. Of particular interest in this study is the authors’ efforts to correlate complications with needle tip placement as observed in the frontal and lateral fluoroscopy images. Their data suggest that deeper needle placement, i.e. more medial in the frontal plane, did not correlate with the incidence of minor complications. A significant relationship (p=0.04) is described between minor complications observed and improper needle positioning in the lateral plane. More anterior or ventral placement of the needle tip within the neural foramen appeared to correlate with the incidence of transient complications.
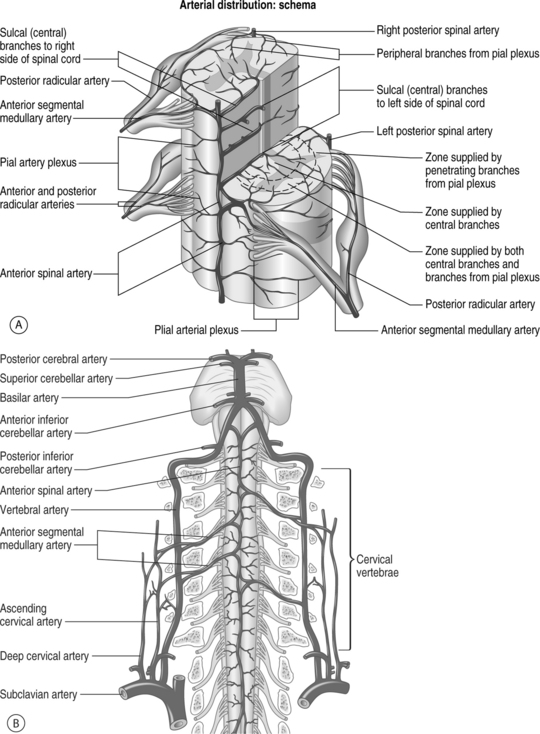
Severe neurological complications following cervical TFESI have also been reported and the pathophysiology behind these events has been the focus of recent discussion and debate.86–91 The complex vasculature of the cervical spine is illustrated in Figure 59.4. Three cases of fatalities arising from either spinal cord or brain injury following TFESI have been reported in the literature.88,91,92 In the first of these cases,91 an anterior spinal artery syndrome following a C6 injection is described. In this case, a 22-gauge spinal needle was reportedly successfully passed into the right C5–6 foramen. A satisfactory contrast pattern is described, and the injection was performed utilizing 0.5 cc of 0.5% bupivacaine and 0.5 cc of triamcinolone. Within 2 minutes the patient developed a flaccid four-extremity paralysis and respiratory compromise. An MRI of the cervical spine revealed increased signal within the spinal cord from C2 to T1. The patient ultimately recovered sensation without improvement in his motor exam, and within 1 month the patient expired from medical complications.
In the second reported case,88 a 48-year-old female was treated with a C6 transforaminal injection utilizing contrast enhancement and a satisfactory epidurogram is similarly described. A 25-gauge, 2” spinal needle was utilized to inject 2 mL of 0.25% bupivacaine and 80 mg of triamcinolone. Upon transfer from the procedure table, the patient became unresponsive. Within 1 hour she regained consciousness but remained with pronounced bilateral lower and right upper extremity weakness. The patient underwent surgical brainstem decompression in the setting of an apparent massive cerebellar infarct. She expired the following day. Intraoperative findings were significant for an anomalous tortuous vertebral artery. Pathology revealed bilateral cerebellar and left occipital cortex infarction with thromboembolism within a leptomeningeal artery adjacent to the left occipital cortex, consistent with an injury to the vertebral artery or an associated branch. In a third fatality case,92 a left C7 TFESI was performed utilizing a 25-gauge, 31–2 spinal needle. Following needle placement in the foramen, initial aspiration was ‘heme positive’ and the needle was therefore repositioned. A satisfactory epidurogram of the C7 nerve root was then appreciated after the injection of contrast, and a 3 cc solution of 80 mg methylprednisolone and 0.75% bupivacaine was injected. The patient immediately became unresponsive. CT imaging revealed a large brainstem hemorrhage, obstructive hydrocephalus, and extensive bleeding throughout the pons and midbrain. The patient expired the following day. Postmortem examination revealed dissection and thrombosis of the left vertebral artery suspected to have resulted from vertebral artery puncture during the injection procedure.
In addition to these three reported fatalities, it has been reported that 15 other cases of death or severe neurologic sequelae have followed cervical TFESI.86,87 The details of cases have yet to be presented or published as they remain sub judice. In one reported case of a marked adverse neurologic complication, a patient suffered from cortical blindness, a partial right homonymous hemianopsia, following TFESI at the C5–6 level.93 In this case, vertebral artery puncture was also suspected, based upon an initial aspirate, and 1 cc of air was intentionally introduced by the authors in an effort to confirm needle placement within the epidural space. Contrast agent was then injected and an unsatisfactory epidurogram was observed. Within seconds, the patient developed nystagmus and, within 45 minutes, total bilateral blindness which ultimately improved. An initial MRI of the brain revealed widespread occipital lobe enhancement, and follow-up imaging on day 4 revealed edema within the left occipital cortex. The authors of this case speculate that complications arose from either direct vertebral artery injury, radiocontrast agent toxicity following intra-arterial injection, or air embolization.82,94
Inadvertent injection of a crystalloid corticosteroid solution into a radicular artery has been theorized as a likely mechanism of injury in those cases where an acute vascular insult to the spinal cord is suspected.86,87,89,90 In these cases it is speculated that a larger-caliber radicular or segmental medullary artery which more critically reinforces the anterior spinal artery becomes compromised during the TFESI. These more critical radicular arteries are located within the neural foramen and can arise variably at the C3 to C8 levels.95,96 Potential mechanisms of radicular artery insult include direct intra-arterial injection, transient vasospasm, arterial compression from a foraminal fluid bolus, or iatrogenic dissection.86–89,91 Contrast flow patterns consistent with inadvertent arterial penetration have been published in which the radicular artery either terminates in multiple spinal cord branches or joins with the anterior spinal artery.86,87 In these cases where such contrast flow was observed, the procedure was terminated secondary to vascular penetration concerns.86,87 In another case, while such arterial flow was not visualized after the injection of contrast, radicular artery injection was suspected, based upon the patient’s response to an initial injection of anesthetic.89 In this case, a satisfactory epidurogram was depicted with the needle placed within the right C6–7 foramen. Injection of 0.8 cc of 2% lidocaine was then performed with a suspected resultant venous flow pattern contralaterally as the ipsilateral periradicular dye was blushed. Over the subsequent 3 minutes, the patient lost motor control of all four extremities as well as sharp sensation, while fine touch sensation and proprioception were preserved. All symptoms, consistent with those arising from an anterior spinal artery syndrome, resolved without sequelae within 20 minutes. The transient nature of these pronounced deficits was likely related to the half-life of the anesthetic agent. Corticosteroid was not subsequently injected. Concurrent injection of corticosteroid in this case may have resulted in a less reversible injury.
The authors in the second fatality case above88 further investigated the potential relationship between corticosteroid particle size and neurologic injury resulting from intra-arterial injection. The authors theorized that injection of the corticosteroid preparation might have contributed to arterial thrombus formation and vascular occlusion. Five commonly utilized corticosteroid preparations were subjected to microscopic study. Following manual agitation, the particles in dexa- and betamethasone tended to be lucent and rod-like, whereas those in the triamcinolone and methylprednisolone samples were amorphous and opaque. Additionally, over time, the particles in the samples of methylprednisolone and triamcinolone tended to form large aggregates in excess of 100 micrometers. The authors speculate that such aggregate formation might be a factor contributing to occlusion of the microvasculature. Direct intraneural spread of injectate along the spinal nerve to the spinal cord has also been suggested as a potential mechanism of spinal cord injury during injection.87,97
Fortunately, after hundreds of cervical TFESI performed in the author’s practice, there have been no significant complications. Candidates for cervical TFESI are carefully selected. Cervical TFESI are utilized predominantly for patients with true radicular pain. Unlike lumbar TFESI, which are often utilized for patients with axial pain, cervical TFESI are less frequently employed for patients without a radicular component. Patients are fully conscious during injections and are repeatedly questioned regarding symptoms during the procedure. Injection needles utilized can range from 22-gauge to 25-gauge, and all agents are injected through microbore tubing to eliminate needle movement during syringe changes. To assure proper and posterior foraminal entry, the desired oblique view is sequentially created from the lateral plane. Once achieved, magnification and columnation are utilized (Fig. 59.5). A dedicated chapter of this text will more completely address cervical TFESI technique. Contrast injection is observed in real time to confirm satisfactory flow and to rule out vascular uptake. Prior to the introduction of corticosteroid and following observation of a satisfactory dye flow pattern, a test dose of local anesthetic, approximately 1 cc of 1% lidocaine, is injected. The patient is then briefly monitored and questioned for any adverse response including an exacerbation of pain complaints in the affected limb, headache, lightheadedness, or other sensorimotor symptoms affecting the upper or lower extremities. While there has been a national shortage of betamethasone suspensions, this agent has been available in limited quantities in the author’s practice and, when available, remains the corticosteroid of choice for cervical injections. The corticosteroid and anesthetic solution is manually agitated prior to injection. By administering all medications through tubing, a lower-pressure injection is performed, likely minimizing transient increases in foraminal pressures and maximizing patient comfort during injection. The use of tubing throughout the injection procedure obviates the need for syringe changes at the interface with the spinal needle and minimizes the likelihood of needle position change during the procedure.
The recent apparent increase in reports describing complications associated with cervical TFESI is likely multifactorial in origin. In part, this increase might parallel an overall increase in the numbers of TFESI performed as this technique is embraced by greater numbers in the interventional spine community. Any interventionist performing cervical TFESI should either first complete dedicated fellowship training or reach a level of greater lumbar procedural experience prior to including this injection approach in the treatment armamentarium. With further standardization of injection technique and training for cervical TFESI, complication rates might be further reduced. The complications reported to date have in large part been vascular in nature. The available case reports reveal devastating incidents resulting from either direct trauma to or injection of the vertebral artery. Other cases are highly suggestive of disruption of a critical penetrating radicular artery, through direct intra-arterial injection, needle trauma, or vasospasm following injection. In the setting of the betamethasone shortage, the possibility remains that the use of corticosteroid solutions containing larger and aggregate-forming particles has contributed to vascular occlusion in some cases. It should be noted that betamethasone has similarly been implicated in a case of suspected vascular insult resulting in a lower thoracic spinal cord injury and paraplegia following a midlumbar TFESI.98 The details of other adverse event cases remain unavailable, but the possibility also exists that some neurologic complications have resulted from more grossly misplaced needles or ill-advised procedural technique.
1 Rydevik B, Brown M, Lundborg G. Pathoanatomy and pathophysiology of nerve root compression. Spine. 1984;9:7-15.
2 Saal JS, Franson RC, Dobrow R, et al. High levels of phospholipase A-2 activity in lumbar disc herniations. Spine. 1990;15:674-678.
3 Olmarker K, Rydevik B, Nordborg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equine nerve roots. Spine. 1993;18:1425-1432.
4 Kayama S, Konno S, Olmarker K, et al. Incision of the anulus fibrosus induces nerve root morphologic, vascular, and function changes: an experimental study. Spine. 1996;21:2539-2543.
5 Lee HM, Weinstein JN, Meller ST, et al. The role of steroids and their effects on phospholipase A2: an animal model of radiculopathy. Spine. 1998;23:1191-1196.
6 Weiner BK, Fraser RD. Foraminal injection for lateral lumbar disc herniation. J Bone Joint Surg [Br]. 1997;79:804-807.
7 Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic transforaminal lumbar epidural steroids: an outcome study. Arch Phys Med Rehab. 1998;79:1362-1366.
8 Botwin KP, Gruber RD, Bouchlas CJ, et al. Fluoroscopically guided lumbar transforaminal steroid injections in degenerative lumbar stenosis: an outcome study. Amer J Phys Med Rehab. 2002;81:898-905.
9 Narozny M, Zanetti M, Boos N. Therapeutic efficacy of selective nerve root blocks in the treatment of lumbar radicular leg pain. Swiss Med Wk. 2001;131:75-80.
10 Riew KD, Yin Y, Gilula L, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, controlled, randomized, double-blind study. J Bone Joint Surg. 2000;82:1589-1593.
11 Butterman GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg. 2004;86:670-679.
12 Vad VB, Bhat AL, Lutz GE, et al. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002;27:11-16.
13 Kang JD, Georgescu HI, McIntyre-Larkin L, et al. Herniated cervical intervertebral discs spontaneously produce matrix metalloproteinases, nitric oxide, interleukin-6, and prostaglandin E2. Spine. 1995;20:2373-2378.
14 Kang JD, Stefanovic-Racic M, McIntyre-Larkin L, et al. Toward a biochemic understanding of human intervertebral disc degeneration. Contributions of nitric oxide, interleukins, prostaglandin E2, and matrix metalloproteinases. Spine. 1997;22:1065-1073.
15 Furusawa N, Baba H, Miyoshi N, et al. Herniation of cervical intervertebral disc: immunohistochemical examination and measurement of nitric oxide production. Spine. 2001;26:1110-1116.
16 Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. J Bone Joint Surg [Am]. 1990;72:403-408.
17 Hitselberger WE, Witten RM. Abnormal myelograms in asymptomatic patients. J Neurosurg. 1968;28:204-206.
18 Wiesel SW, Tsourmas N, Feffer HL, et al. A study of computer-assisted tomography. I. The incidence of positive CAT scans in an asymptomatic group of patients. Spine. 1984;9:549-551.
19 Boden SD, McCowin PR, Davis DO, et al. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. J Bone Joint Surg [Am]. 1990;72:1178-1184.
20 Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine. 1986;11:521-524.
21 Maigne JY, Rime B, Deligne B. Computed tomographic follow-up study of forty-eight cases of nonoperatively treated lumbar intervertebral disc herniation. Spine. 1992;17:1071-1074.
22 Bozzao A, Gallucci M, Masciocci C, et al. Lumbar disc herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology. 1992;185:135-141.
23 Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine. 1990;15:683-686.
24 Komori H, Owaka A, Muneta T, et al. Contrast-enhanced magnetic resonance imaging in conservative management of lumbar intervertebral disc herniation. Spine. 1998;23:67-73.
25 Mochida K, Komori H, Owaka A, et al. Regression of cervical disc herniation observed on magnetic resonance images. Spine. 1998;23:990-995.
26 Maigne JY, Guedj S, Straus C. Computed tomographic follow-up study of 21 cases of nonoperatively treated cervical intervertebral soft disc herniation. Spine. 1994;19:189-191.
27 Bush K, Chaudhuri R, Hillier S, et al. The pathomorphologic changes that accompany the resolution of cervical radiculopathy. A prospective study with repeat magnetic resonance imaging. Spine. 1997;22:183-187.
28 White AH. Injection techniques for the diagnosis and treatment of low back pain. Ortho Clin N Am. 1983;14:553-567.
29 Stojanovic MP, Vu TN, Caneris O, et al. The role of fluoroscopy in cervical epidural steroid injections: an analysis of contrast dispersal patterns. Spine. 2002;27:509-514.
30 Bogduk N, Christophidis N, Cherry D, et al. Epidural steroids in the management of back pain and sciatica of spinal origin. Report of the Working Party on Epidural Use of Steroids in the Management of Back Pain. Canberra: National Health and Medical Research Council, 1993.
31 Furman MB, O’Brien EM, Zgleszewski TM. Incidence of intravascular penetration in lumbosacral epidural steroid injections. Spine. 2000;20:2628-2632.
32 Sullivan WJ, Willick SE, Chira-Adisai W, et al. Incidence of intravascular uptake in lumbar spinal injection procedures. Spine. 2000;25:481-486.
33 Furman MB, Giovanniello MT, O’Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine. 2003;28:21-25.
34 Cluff R, Mehio AK, Cohen SP, et al. The technical aspects of epidural steroid injections: a national survey. Anesth Analg. 2002;95:403-408.
35 Winnie AP, Hartman JT, Myers HL, et al. Pain clinic II: Intradural and extradural corticosteroids for sciatica. Anesth Analg. 1972;51:991-1003.
36 Cicala RS, Westbrook L, Angel JJ. Side effects and complications of cervical epidural steroid injections. J Pain Sympt Manag. 1989;4:64-66.
37 Purkis IE. Cervical epidural steroids. Pain Clin. 1986;1:3-7.
38 Rowlingson JC, Kirschenbaum LP. Epidural analgesic techniques in the management of cervical pain. Anesth Analg. 1986;65:938-942.
39 Shulman M. Treatment of neck pain with cervical epidural injection. Reg Anesth. 1986;11:92-94.
40 Woodward JL, Weinstein SM. Epidural injections for the diagnosis and management of axial and radicular pain syndromes. Phys Med Rehab Clin N Am. 1995;6:691-714.
41 Warfield CA, Biber MP, Crews DA, et al. Epidural steroid injection as a treatment for cervical radiculitis. Clin J Pain. 1988;4:201-204.
42 Mangar D, Thomas PB. Epidural steroid injections in the treatment of cervical and lumbar pain syndromes. Reg Anesth. 1991;16:246.
43 Ferrante FM, Wilson SP, Iacobo C, et al. Clinical classification as a predictor of therapeutic outcome after cervical epidural steroid injection. Spine. 1993;18:730-736.
44 Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine. 1996;21:1877-1883.
45 Samapth P, Bendebba M, Davis JD, et al. Outcome in patients with cervical radiculopathy. Spine. 1999;24:591-597.
46 Schutz H, Lougheed WM, Wortzman G, et al. Intervertebral nerve-root in the investigation of chronic lumbar disc disease. Can J Surg. 1973;16:217-221.
47 Krempen JF, Smith BS. Nerve root injection: a method for evaluating the etiology of sciatica. J Bone Joint Surg. 1974;56:1435-1444.
48 Haueisen DC, Smith BS, Myers SR, et al. The diagnostic accuracy of spinal nerve injection studies: their role in the evaluation of recurrent sciatica. Clin Orthop Rel Res. 1985;198:179-183.
49 Van Akkerveeken PF. The diagnostic value of nerve root sheath infiltration. Acta Orthop Scand. 1993;251:62-63.
50 Kikuchi S, Macnab I, et al. Localisation of the level of symptomatic cervical disc degeneration. J Bone Joint Surg [Br]. 1981;63:272-277.
51 Nordmann DK, Macadaeg K, Sasso RC. Selective nerve root injections can predict surgical outcome for lumbar and cervical radiculopathy: a retrospective review with comparison to magnetic resonance imaging. Spine J. 2002;2:29S.
52 Slipman CW, Plastaras CT, Palmitier RA, et al. Symptom provocation of fluoroscopically guided cervical nerve root stimulation. Are dynatomal maps identical to dermatomal maps? Spine. 1998;23:2235-2242.
53 Foerster O. The dermatomes in man. Brain. 1933;102:1-39.
54 Keegan JJ, Garrett FD. The segmental distribution of the cutaneous nerves in the limbs of man. Anat Rec. 1948;102:409-437.
55 Moriishi J, Otani K, Tanaka K, et al. The intersegmental anastomoses between spinal nerve roots. Anat Rec. 1989;224:110-116.
56 Tanaka N, Fujimoto Y, An HS, et al. The anatomic relation between the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine. 2000;25:286-291.
57 Bush K, Hillier S. Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections: a prospective study with independent clinical review. Eur Spine J. 1996;5:319-325.
58 Bush K, Cowan N, Katz DE, et al. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiographic follow up. Spine. 1992;17:1205-1212.
59 Vallee JN, Feydey A, Carlier RY, et al. Chronic cervical radiculopathy: lateral-approach periradicular corticosteroid injection. Radiology. 2001;218:886-892.
60 Cyteval C, Thoma E, Decoux E, et al. Cervical radiculopathy: open study on percutaneous periradicular foraminal steroid infiltration performed under CT control in 30 patients. Am J Neuroradiol. 2004;25:441-445.
61 Berger O, Dousset V, Delmer O, et al. Evaluation of CT-guided periganglionic foraminal steroid injections for treatment of radicular pain in patients with foraminal stenosis. J Radiol. 1999;80:917-925.
62 Slipman CW, Lipetz JS, Jackson HB, et al. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehab. 2000;81:741-746.
63 Slipman CW, Lipetz JS, Jackson HB, et al. Outcomes of therapeutic selective nerve root blocks for whiplash induced cervical radicular pain. Pain Physician. 2001;4:167-174.
64 Slipman CW, Lipetz JS, Depalma MJ, et al. Therapeutic selective nerve root block in the nonsurgical treatment traumatically induced cervical spondylotic radicular pain. Am J Phys Med Rehabil. 2004;83:446-454.
65 Karppinen J, Malmivaara A, Kurunlahti M, et al. Periradicular infiltration for sciatica: a randomized controlled trial. Spine. 2001;26:1059-1067.
66 Olmarker K, Rydevik B, Holm S. Edema formation in spinal nerve roots induced by experimental graded compression. Spine. 1989;14:569-573.
67 Igarashi T, Kikuchi S, Shubayev V, et al. 2000 Volvo Award winner in basic science studies. Exogenous tumor necrosis factor-alpha mimics nucleus pulposus induced neuropathology. Molecular, histologic, and behavioral comparisons in rats. Spine. 2000;25:2975-2980.
68 Harrington JF, Messier AA, Bereiter D, et al. Herniated lumbar disc material as a source of free glutamate available to affect pain signals through the dorsal root ganglion. Spine. 2000;25:929-936.
69 Hodges SD, Castleberg RL, Miller T, et al. Cervical epidural steroid injection with intrinsic cord damage. Two case reports. Spine. 1998;23:2137-2142.
70 Cicala RS, Westbrook A, Angel JJ. Side effects and complications of cervical epidural injections. J Pain Sympt Manag. 1989;4:64-66.
71 Nelson DA. Dangers from methylprednisolone acetate (Depo-Medrol) therapy by intraspinal injection. Arch Neurol. 1988;45:804-806.
72 Botwin KP, Castellanos R, Rao S, et al. Complications of fluoroscopically guided interlaminar cervical epidural injections. Arch Phys Med Rehab. 2000;81:1045-1050.
73 Slipman CW, Shin CH, Patel RK. Persistent hiccup associated with thoracic epidural injection. Am J Phys Med Rehab. 2001;80:618-621.
74 Slipman CW, Chow DW, Lenrow DA. Dysphonia associated with epidural steroid injection: a case report. Am J Phys Med Rehab. 2002;83:1309-1310.
75 Haimovic IC, Beresford HR. Dexamethasone is not superior to placebo for treating lumbosacral radicular pain. Neurology. 1986;36:1593-1594.
76 Field J, Rathmell JP, Stephenson JH, et al. Neuropathic pain following cervical epidural injection. Anesthesiology. 2000;93:885-888.
77 Siegfried RN. Development of complex regional pain syndrome after cervical epidural steroid injection. Anesthesiology. 1997;86:1394-1396.
78 Huang RC, Shapiro GS, Lim M, et al. Cervical epidural abscess after cervical epidural steroid injection. Spine. 2004;29:E7-E9.
79 Stoll A, Sanchez M. Epidural hematoma after epidural block: implications for its use in pain management. Surg Neurol. 2002;57:235-240.
80 Tuel SM, Meythaler JM, Cross LL. Cushing’s syndrome from epidural methylprednisolone. Pain. 1990;40:81-84.
81 Catchlove RFH, Braha R. Clinical reports: the use of cervical blocks in the management of chronic head and neck pain. Can Anaesth Soc J. 1984;31:188-191.
82 Reitman CA, Watters W. Subdural hematoma after cervical epidural steroid injection. Spine. 2002;27:E174-E176.
83 Huston CW, Slipman CW, Garvan CW. Complications and side effects of cervical and lumbosacral selective nerve root injections. Arch Phys Med Rehab. 2005;86:277-283.
84 Brady RD. Complications of transforaminal cervical epidural steroid injections. Proceedings of the North American Spine Society. 14th Annual Meeting. 1999:142-143.
85 Ma D, Gilula L, Riew D. Complication of fluoroscopically guided extraforaminal cervical nerve blocks – an analysis of 1036 injections. Spine J. 2004;4:5S-21S.
86 Baker R, Drefuss P, Mercer S, et al. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003;103:211-215.
87 Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004;100:1595-1600.
88 Tiso RL, Cutler T, Catania JA, et al. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004;4:468-474.
89 Karasek M, Bogduk N. Temporary neurologic deficit after cervical transforaminal injection of local anesthetic. Pain Med. 2004;5:202-205.
90 Kloth DS. Risk of cervical transforaminal epidural injections by anterior approach. Pain Phys. 2003;6:392-393.
91 Brouwers PJAM, Kottink EJBL, Simon MAM, et al. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001;91:397-399.
92 Rozin L, Roman R, Koehler SA, et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Foren Med Path. 2003;24:351-355.
93 McMillan MR, Crumpton CR. Cortical blindness and neurologic injury complicating cervical transforaminal injection for cervical radiculopathy. Anesthesiology. 2003;99:509-511.
94 De Cordoba JL, Bernal J. Cervical transforaminal blocks should not be attempted by anyone without extensive documented experience in fluoroscopically guided injections. Anesthesiology. 2004;100:1323-1324.
95 Chakravorty BG. Arterial supply of the cervical spinal cord (with special reference to the radicular arteries). Anat Rec. 1971;170:311-330.
96 Turnbull IM, Brieg A, Hassler O. Blood supply of the cervical spinal cord in man. A microangiographic study. J Neurosurg. 1966;21:951-965.
97 Selander D, Sjostrand. Longitudinal spread of intraneurally injected local anesthetics. Acta Anaesth Scand. 1978;22:622-634.
98 Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: a report of three cases. Spine J. 2002;2:70-75.