60 Cervical Plexus Block
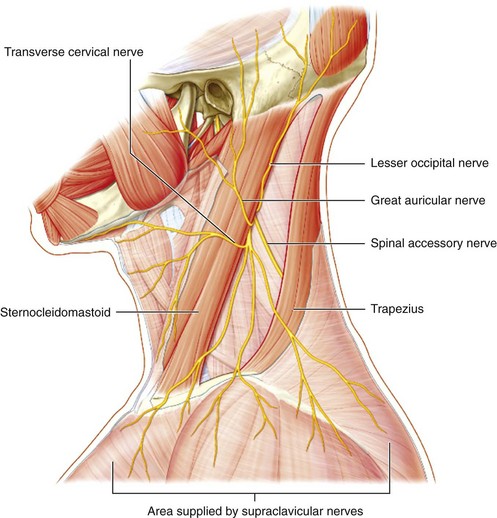
The cervical plexus derives from the ventral rami of C2, C3, and C4. Its superficial branches primarily consist of the lesser occipital, great auricular, transverse cervical, and supraclavicular nerves. These nerves innervate the skin of the neck and shoulder. The nerves converge at the posterolateral border of the sternocleidomastoid muscle, where cervical plexus block can be performed. Common indications for cervical plexus block include carotid endarterectomy, thyroid and parathyroid surgery, and surgery on the clavicle.1
Ultrasound imaging is useful for guiding blocks of the cervical plexus. Sonographic landmarks can be identified and in some cases direct nerve imaging is possible. Optimal needle tip placement with in-plane approach can be used to target injections and potentially avoid complications.2 Cervical plexus blocks are sometimes classified as superficial or deep according to whether or not the nerves have pierced the prevertebral fascia at the site of injection. Intermediate cervical plexus blocks target the cervical plexus where its nerves lie underneath the sternocleidomastoid muscle.3 This technique is highly amenable to ultrasound guidance and is described here.
Suggested Technique
Several sonographic landmarks more precisely determine the level for cervical plexus block injections (Table 60-1):
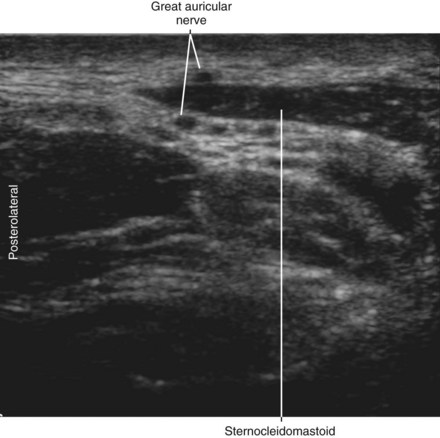
1. The great auricular nerve is the largest branch of the cervical plexus and is often visible as it lies over the sternocleidomastoid muscle. Cervical plexus block can be performed just caudal to the point at which the great auricular nerve wraps around the posterolateral edge of the sternocleidomastoid muscle to join the remainder of the cervical plexus.
2. The external jugular vein crosses the posterolateral edge of the sternocleidomastoid muscle. The cervical plexus emerges at the muscle edge to lie underneath the external jugular vein. This vein can serve as a tubular conduit to promote distribution of the injection to the underlying cervical plexus.
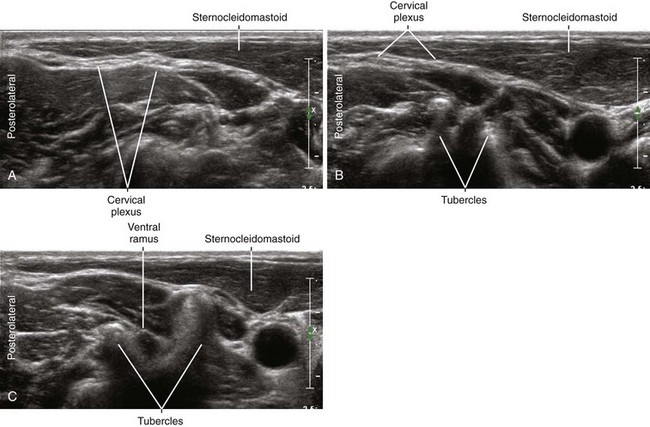
3. Cervical levels can be estimated by cervical vertebral morphology on ultrasound imaging scans.4,5 The anterior tubercle of the seventh cervical transverse process is rudimentary. In contrast, the anterior tubercle of the sixth cervical transverse process (sometimes referred to as Chassaignac’s tubercle) is prominent compared with its posterior tubercle. This bony morphology can be used to identify higher cervical levels when performing cervical plexus blocks. In addition, the first segment of the vertebral artery lies anterior to the seventh cervical transverse process before it enters the cervical spinal canal. The intervening space (sulcus) between the anterior and posterior tubercles becomes progressively smaller as one slides the transducer cephalad. This is because the exiting ventral rami are smaller at the higher cervical vertebrae. The cervical plexus can be blocked just deep to the sternocleidomastoid muscle at the level of the C4 foramina as assessed in a transverse plane of imaging.
4. At the level for cervical plexus block, the ventral rami of the brachial plexus are not visible and the scalene muscles taper off to small diameter. At this level the longus capitis and levator scapulae muscles are more prominent.
Table 60-1 Sonographic Landmarks for Intermediate Cervical Plexus Block*
| Location for Intermediate Cervical Plexus Block | Comment on the Sonographic Landmarks |
|---|---|
| Where the EJ crosses the posterolateral edge of the SCM | The cervical plexus emerges to lie underneath the EJ. |
| Where the GAN rounds the posterolateral edge of the SCM | The GAN is the largest branch of the cervical plexus and therefore relatively easy to identify. |
| At the level of the C4 transverse process |
EJ, External jugular vein; GAN, great auricular nerve; SCM, sternocleidomastoid muscle.
* This block is performed with a transverse view of the posterolateral edge of the sternocleidomastoid to guide injection underneath this muscle where the cervical plexus organizes. The level of block is chosen to help complete distribution of the injection to the entire cervical plexus. The transducer slides in a cephalocaudad fashion to identify these landmarks for intermediate cervical plexus block. Although the quality of these sonographic landmarks can vary from patient to patient, all four locations are very close to each other
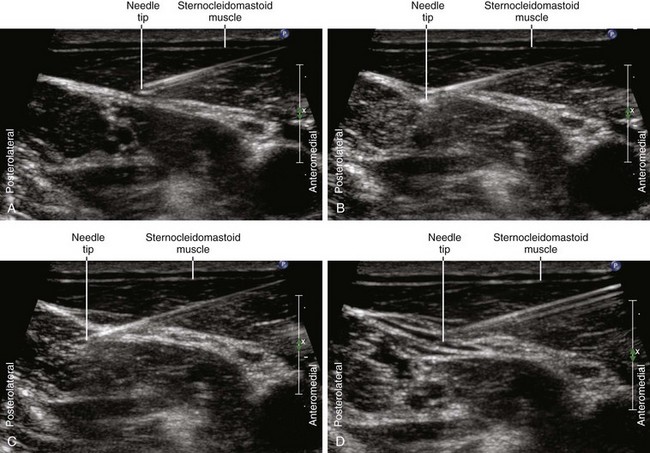
A transverse view with in-plane approach (medial to lateral or lateral to medial) can be used to place the needle tip through the posterolateral edge of the sternocleidomastoid muscle. A 25-gauge, 1.5-inch hypodermic needle on extension tubing or control syringe can be used to administer 10 mL of local anesthetic for the block. The ulnar aspect of the hand controlling the needle should rest on the neck to stabilize and retract the mobile skin. The injection should have a crescent-shaped distribution as it layers along the undersurface of the sternocleidomastoid muscle for cervical plexus block.6 The extent of cervical plexus block can be clinically measured by testing the skin over the clavicle (supraclavicular nerve territory), behind the ear (lesser occipital nerve territory), and posterior ear (great auricular nerve territory).
Key Points
| Cervial Plexus Block | The Essentials |
|---|---|
| Anatomy | The cervical plexus lies under the SCM. |
| The cervical plexus contributions lie in the cervical interscalene groove (between AS and MS caudally, or between LC and LS cephalad). | |
| Cutaneous branches of the cervical plexus emerge at posterolateral edge of the SCM. | |
| The cervical plexus lies under the EJ at the SCM border. | |
| The C4 ventral ramus and foramina are smaller than at lower levels. | |
| Image orientation | The SCM has a tapering posterolateral edge. |
| Positioning | Supine with arms at side, head turned to opposite side |
| Support the head position with gel donut. | |
| Operator | Standing at the side of the patient |
| Display | Across the table |
| Transducer | High-frequency linear, 23- to 38-mm footprint |
| Initial depth setting | 20 to 25 mm |
| Needle | 25 gauge, 38 mm in length |
| Anatomic location | Begin by scanning to identify the posterolateral edge of the SCM. |
| Cervical plexus block is usually performed at the C4 level, where BP is not visible. | |
| Approach | Transverse view of SCM, in-plane from medial to lateral |
| Place the needle tip through the SCM near its posterolateral edge. | |
| The needle may cross into the MS or LS muscle. | |
| Inject as the needle is slowly withdrawn. | |
| Sonographic assessment | The injection should layer underneath the SCM. |
| Anatomic variation | Contributions to the cervical plexus vary. |
Key Points
| Cervical Plexus Block | The Essential Points |
|---|---|
| Superficial | Infiltrate local anesthetic deep to the platysma and EJ along the posterolateral border of the SCM. |
| Intermediate | Inject local anesthetic deep to the SCM near its posterolateral border at the midpoint of this muscle. |
| Deep | Inject local anesthetic around the cervical ventral rami near their exit from the respective cervical foramina. |
Key Points
| Cervical Plexus Territory | Cutaneous Assessment |
|---|---|
| Lesser occipital nerve (LON) | Behind the upper part of the external ear |
| Great auricular nerve (GAN) | Along the posterior aspect of the helix near the lobule |
| Transverse cervical nerve (TCN) | Under the body of the mandible |
| Supraclavicular nerve (SCN) | Over the clavicle |
Clinical Pearls
• For some surgeries (such as shoulder surgery) an interscalene block can be performed with a high volume of local anesthetic when it is desirable to anesthetize both the cervical and brachial plexus. With this technique some local anesthetic is injected as the needle is withdrawn to anesthetize branches of the superficial cervical plexus.
• It is important to inject within the fascial layer underneath the sternocleidomastoid muscle. This is best accomplished by placing the needle tip through the posterolateral corner of the sternocleidomastoid muscle and then slowly withdrawing the needle as local anesthetic is injected using low pressure and a fine 25- or 27-gauge needle. Do not advance the block needle into the anterior scalene muscle because the phrenic nerve is located on the surface of this muscle.7 The phrenic nerve does not course lateral to the interscalene groove.
• The great auricular nerve and external jugular vein have a parallel course over the surface of the sternocleidomastoid muscle, with the great auricular nerve lying on the cephalad side of the vein. The great auricular nerve can be traced to help localize the other smaller nerves of the cervical plexus. Because the great auricular nerve loops down around the edge of the sternocleidomastoid muscle it can be seen both superficial and deep to this muscle in one field of transverse view.
• Because the middle scalene muscle inserts on higher cervical transverse processes than the anterior scalene muscle, the middle scalene muscle can be followed farther cephalad on ultrasound scans.
• Unlike the brachial plexus, the nerves of the cervical plexus are directed both cephalad and caudad from their spinal origin, so they do not stack up in a compact organized fashion but rather consist of loops and divergent branches. The innervation of the neck has contributions from descending branches of cranial nerves and ascending branches that run with sympathetic nerves. Therefore, cervical plexus blocks usually do not serve as definitive anesthetics and the need for airway control is an important consideration.
1 Roessel T, Wiessner D, Heller AR, et al. High-resolution ultrasound-guided high interscalene plexus block for carotid endarterectomy. Reg Anesth Pain Med. 2007;32(3):247–253.
2 Fredrickson MJ. Superficial cervical plexus neuropathy with chronic pain after superficial cervical plexus block and interscalene catheter placement. Reg Anesth Pain Med. 2011;36(2):206.
3 Choquet O, Dadure C, Capdevila X. Ultrasound-guided deep or intermediate cervical plexus block: the target should be the posterior cervical space. Anesth Analg. 2010;111(6):1563–1564.
4 Martinoli C, Bianchi S, Santacroce E, et al. Brachial plexus sonography: a technique for assessing the root level. AJR Am J Roentgenol. 2002;179(3):699–702.
5 Soeding P, Eizenberg N. Review article: anatomical considerations for ultrasound guidance for regional anesthesia of the neck and upper limb. Can J Anaesth. 2009;56(7):518–533. Epub 2009, May 28. Review
6 Tran de QH, Dugani S, Finlayson RJ. A randomized comparison between ultrasound-guided and landmark-based superficial cervical plexus block. Reg Anesth Pain Med. 2010;35(6):539–543.
7 Kessler J, Schafhalter-Zoppoth I, Gray AT. An ultrasound study of the phrenic nerve in the posterior cervical triangle: implications for the interscalene brachial plexus block. Reg Anesth Pain Med. 2008;33(6):545–550.