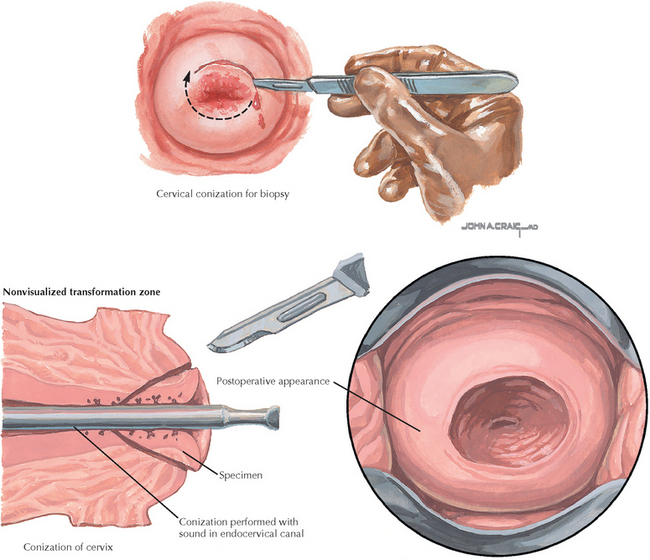
Chapter 234 Cervical Conization (Cold Knife)
REQUIRED EQUIPMENT
CPT CODE(S)
Cullimore JE, Luesley DM, Rollason TP, et al. A prospective study of conization of the cervix in the management of cervical intraepithelial glandular neoplasia (CIGN)—A preliminary report. Br J Obstet Gynaecol. 1992;99:314.
Duggan BD, Felix JC, Muderspach LI, et al. Cold-knife conization versus conization by the loop electrosurgical excision procedure: a randomized, prospective study. Am J Obstet Gynecol. 1999;180:276.
Mathevet P, Dargent D, Roy M, et al. A randomized prospective study comparing three techniques of conization: cold knife, laser, and LEEP. Gynecol Oncol. 1994;54:175.
El-Bastawissi AY, Becker TM, Daling JR. Effect of cervical carcinoma in situ and its management on pregnancy outcome. Obstet Gynecol. 1999;93:207.
Jackobsson M, Gissler M, Sainio S, et al. Preterm delivery after surgical treatment for cervical intraepithelial neoplasia. Obstet Gynecol. 2007;109:309.
Kyrgiou M, Koliopoulos G, Martin-Hirsch P, et al. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;367:489.
Kyrgiou M, Tsoumpou I, Vrekoussis T, et al. The up-to-date evidence on colposcopy practice and treatment of cervical intraepithelial neoplasia: the Cochrane colposcopy and cervical cytopathology collaborative group (C5 group) approach. Cancer Treat Rev. 2006;32:516.
Sadler L, Saftlas A, Wang W, et al. Treatment for cervical intraepithelial neoplasia and risk of preterm delivery. JAMA. 2004;291:2100.
American College of Obstetricians and Gynecologists. Diagnosis and treatment of cervical carcinomas. ACOG Practice Bulletin 35. Obstet Gynecol. 2002;99:855.
American College of Obstetricians and Gynecologists. Management of abnormal cervical cytology and histology. ACOG Practice Bulletin 66. Obstet Gynecol. 2005;106:645.
Montz FJ. Impact of therapy for cervical intraepithelial neoplasia on fertility. Am J Obstet Gynecol. 1996;175:1129.
Morris M, Mitchell MF, Silva EG, et al. Cervical conization as definitive therapy for early invasive squamous carcinoma of the cervix. Gynecol Oncol. 1993;51:193.
Sokol H. A modification of the Sturmdorf suture. Am J Obstet Gynecol. 1964;89:823.