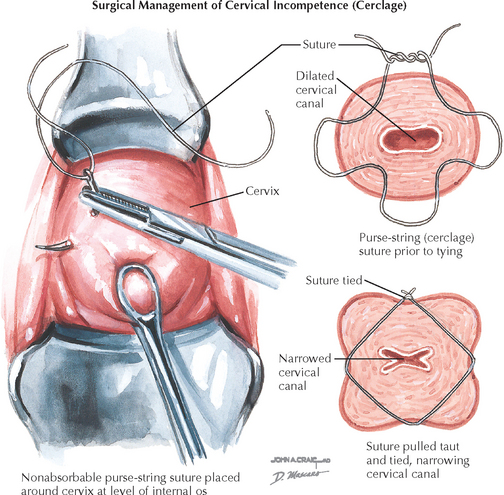
Chapter 233 Cervical Cerclage
REQUIRED EQUIPMENT
Althuisius SM, Dekker GA, Hummel P, et al. Final results of the Cervical Incompetence Prevention Randomized Cerclage Trial (CIPRACT): Therapeutic cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol. 2001;185:1106.
Althuisius SM, Dekker GA, Hummel P, van Geijn HP, Cervical Incompetence Prevention Randomized Cerclage Trial. Cervical Incompetence Prevention Randomized Cerclage Trial: Emergency cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol. 2003;189:907.
Berghella V, Odibo AO, Tolosa JE. Cerclage for prevention of preterm birth in women with a short cervix found on transvaginal ultrasound examination: a randomized trial. Am J Obstet Gynecol. 2004;191:1311.
Lazar P, Gueguen S, Dreyfus J, et al. Multicentred controlled trial of cervical cerclage in women at moderate risk of preterm delivery. Br J Obstet Gynaecol. 1984;91:731.
Rush RW, Isaacs S, McPherson K, et al. A randomized controlled trial of cervical cerclage in women at high risk of spontaneous preterm delivery. Br J Obstet Gynaecol. 1984;91:724.
Secher NJ, McCormack CD, Weber T, et al. Cervical occlusion in women with cervical insufficiency: protocol for a randomised, controlled trial with cerclage, with and without cervical occlusion. BJOG. 2007;114:649. e1.
To MS, Alfirevic Z, Heath VC, et alFetal Medicine Foundation Second Trimester Screening Group. Cervical cerclage for prevention of preterm delivery in women with short cervix: randomized controlled trial. Lancet. 2004;363:1849.
Belej-Rak T, Okun N, Windrim R, et al. Effectiveness of cervical cerclage for a sonographically shortened cervix: a systematic review and meta-analysis. Am J Obstet Gynecol. 2003;189:1679.
Berghella V, Odibo AO, To MS, et al. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106:181.
Drakeley AJ, Roberts D, Alfirevic Z. Cervical cerclage for prevention of preterm delivery: meta-analysis of randomized trials. Obstet Gynecol. 2003;102:621.
Harger JH. Cerclage and cervical insufficiency: an evidence-based analysis. Obstet Gynecol. 2002;100:1313.
Rust OA, Atlas RO, Meyn J, et al. Does cerclage location influence perinatal outcome? Am J Obstet Gynecol. 2003;189:1688.
Zaveri V, Aghajafari F, Amankwah K, Hannah M. Abdominal versus vaginal cerclage after a failed transvaginal cerclage: a systematic review. Am J Obstet Gynecol. 2002;187:868.
Althuisius SM, van Geijn HP. Strategies for prevention—Cervical cerclage. BJOG. 2005;112:51.
American College of Obstetricians and Gynecologists. Cervical insufficiency. ACOG Practice Bulletin 48. Obstet Gynecol. 2003;102:1091.
American College of Obstetricians and Gynecologists. Ultrasonography in pregnancy. ACOG Practice Bulletin 58. Obstet Gynecol. 2004;104:1449.
Cunningham FG, Gant NF, Leveno KJ, et al, editors Williams Obstetrics 21st ed. 2001 McGraw-Hill New York 862
McDonald IA. Suture of the cervix for inevitable abortion. J Obstet Gynaecol Br Emp. 1957;64:346.
McDonald IA. Incompetence of the cervix. Aust N Z J Obstet Gynaecol. 1978;18:34.
McNamara HM. Problems and challenges in the management of preterm labour. BJOG. 2003;110:79.
Noori M, Helmig RB, Hein M, Steer PJ. Could a cervical occlusion suture be effective at improving perinatal outcome? BJOG. 2007;114:532.
Romero R, Espinoza J, Erez O, Hassan S. The role of cervical cerclage in obstetric practice: can the patient who could benefit from this procedure be identified? Am J Obstet Gynecol. 2006;194:1.