Cervical Cerclage
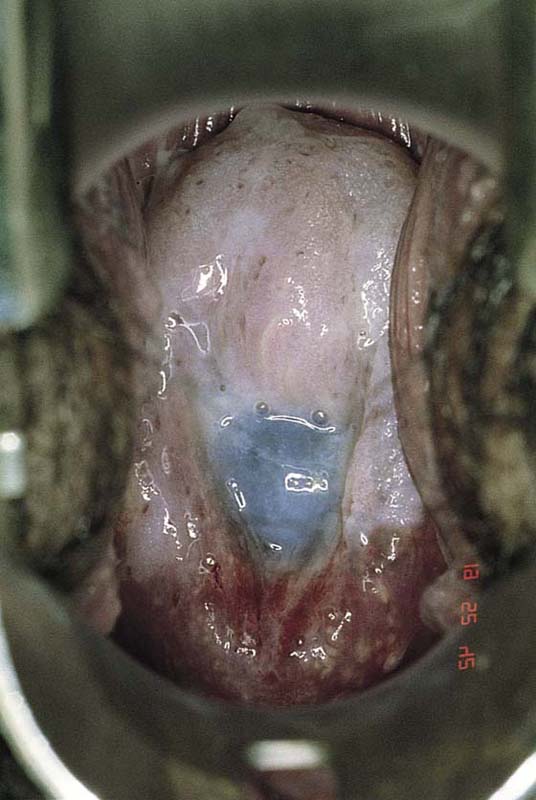
Cervical incompetence (cervical insufficiency) is a nebulous condition characterized by pain-free dilatation and shortening of the cervix in the second or early third trimester of pregnancy (Fig. 49–1). This is followed by prolapse of the membranes through the cervix and, ultimately, by expulsion of the fetus with or without membrane rupture (Fig. 49–2). The diagnosis of cervical insufficiency depends primarily on an obstetric history of one or more pregnancy losses associated with painless labor and dilatation.
Once the diagnosis has been at least presumptively made, a decision must be reached about whether to suture the cervix. Most cerclage operations are performed via the vaginal approach. The technique of abdominal cerclage is described and shown in Unit I.
The Shirodkar surgical procedure is aimed at restoring the cervix to a nondilated state as well as lengthening the cervical canal. Essentially, in this operation a nonresorbable suture is placed at or above the level of the internal os of the cervix. If lengthening is to be achieved, then a portion of the corporal isthmus should be incorporated into the encompassing suture. This will eliminate the funnel effect of the membranes at the top of the cervical canal and will add 1 to 2 cm of length to the canal. Care must be taken to dissect the vagina away from the cervix and to retract it superiorly and anteriorly to avoid injury to the terminal ureter (i.e., at the uterovesical junction). As is noted in Section F Unit II, the ureters cross the vagina at the anterior and anterolateral fornices to gain entry to the bladder base (trigone).
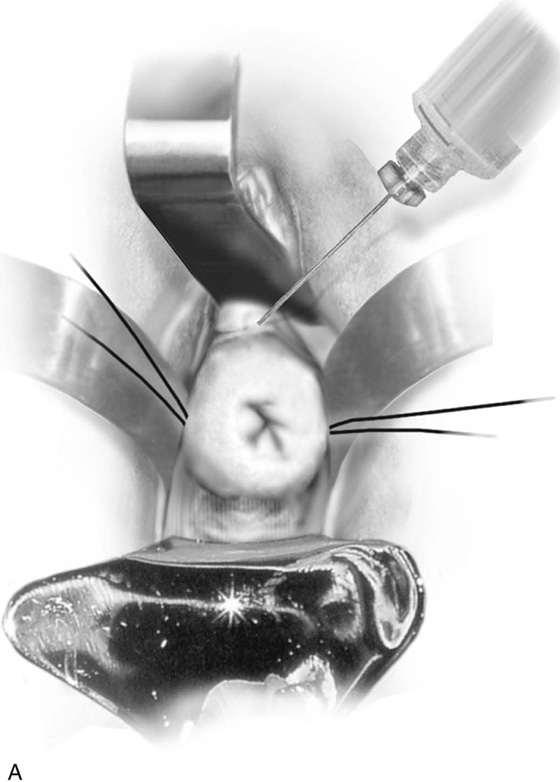
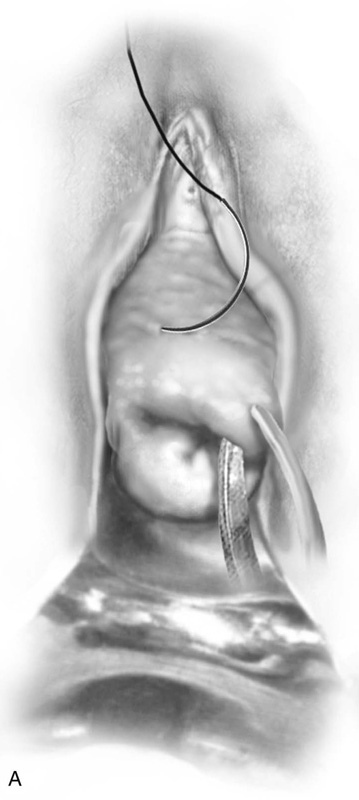
The cervix is exposed by placing a weighted retractor into the posterior fornix. Small Dever retractors are placed in the lateral vaginal fornices, and a finger (small Richardson) retractor is placed in the anterior fornix. Sutures of 0 Vicryl are placed into the cervix at the 3 and 9 o’clock positions in figure-of-8 fashion for traction (Fig. 49–3A). These sutures should not be placed too far back into the lateral fornix because they can occlude the ureter. The sutures must be placed in the cervix forward of the vaginal reflection.
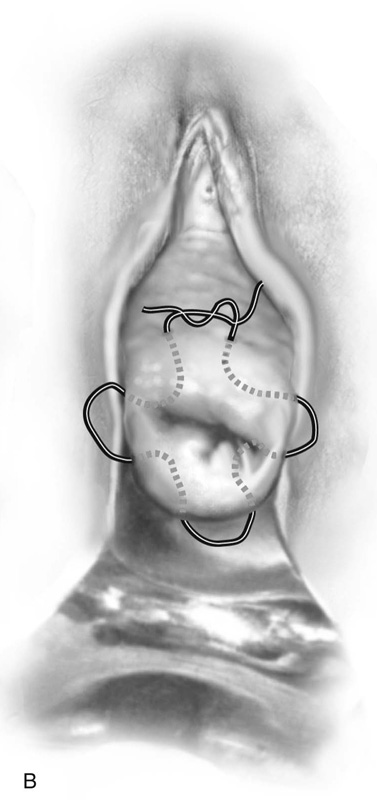
Next, 10 to 20 mL of normal saline is injected into the anterior cervix at the point of the vaginal reflection to create a plane of dissection. A similar injection is made into the posterior aspect of the cervix. A 2-cm incision is made with a scalpel into the vaginal reflection. The vagina is easily separated and dissected from the cervix. A similar procedure is carried out posteriorly. Retractors can now be placed between the cervix and the vagina (Fig. 49–3B, C).
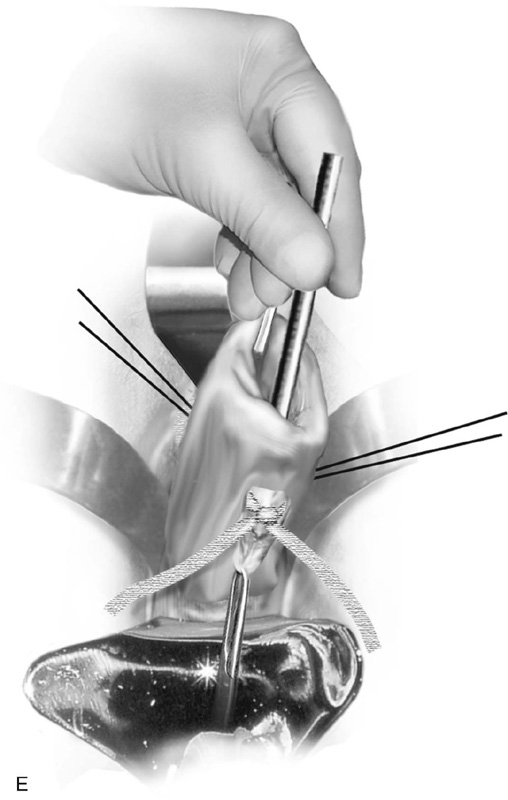
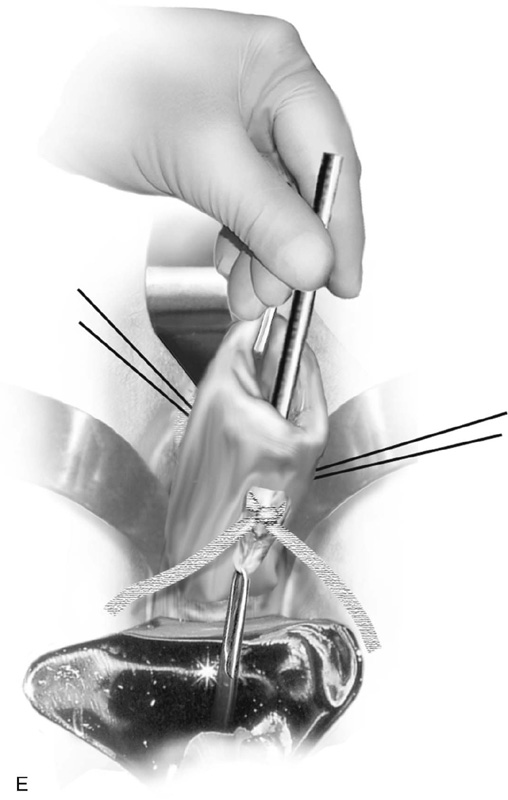
A Mersilene band on a double-armed needle is introduced into the anterior incision at or above the level of the internal os. The needle is slipped between the vagina and the cervix, respectively, on the right and left sides and is brought out at the posterior incision site (Fig. 49–3D). The suture is tied into place posteriorly taking care not to squeeze the cervix so much as to cause the band to cut into the substance of the cervix or, even worse, through the cervix. This can be prevented by inserting a metal catheter or a firm rubber catheter into the cervix and tightening over the catheter (Fig. 49–3E). A 3-0 Prolene stitch should be placed into the cervix and through the band both anteriorly and posteriorly to prevent the band from displacing. The mucosa is closed with simple interrupted 2-0 Vicryl sutures (Fig. 49–3F).
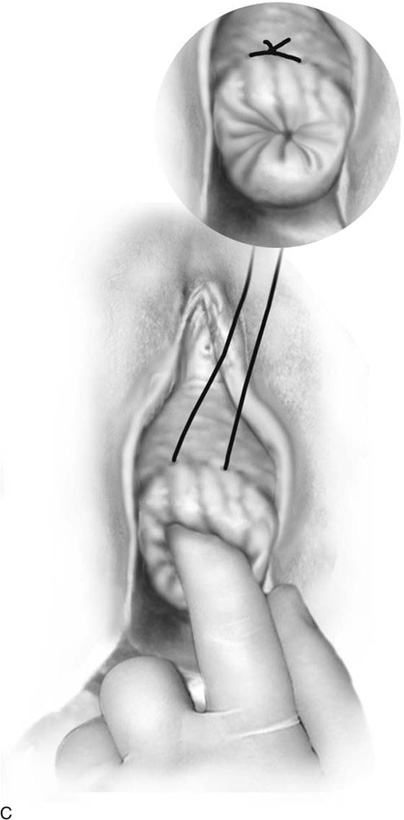
McDonald originally specified that a No. 4 braided silk suture should be placed into the cervix beginning anteriorly (12 o’clock) at the point where the rugose vagina is reflected onto the smooth mucosa of the cervix and is carried clockwise or counterclockwise, taking peripheral bites with the needle around the cervix through the 3, 6, and 9 o’clock positions until arriving back at the 12 o’clock position (Fig. 49–4A, B). At that point, the stitch is tightened over the assistant’s index or little finger inserted into the patient’s cervical canal and is secured with three or four throws of the knot (Fig. 49–4C). Although McDonald thought the cervicovaginal junction corresponded to the internal os, in reality it is below that location (Fig 49–4C, inset). Placing the suture at the internal os would mean suturing into the anterior vagina and possibly injuring the ureters or the urinary bladder. Currently, #2 Prolene and Mersilene are the suture materials most commonly used for this cerclage technique.
FIGURE 49–1 This patient was referred for colposcopy and biopsy because of an abnormal Pap smear. The cervix is agape with the canal dilated and shortened. The blue-tinged membranes are clearly visible.
FIGURE 49–2 This painless labor progressed rapidly. The cervix is 5 cm dilated and completely effaced, and the membranes are bulging into the vagina.
FIGURE 49–3 A. Shirodkar cerclage. The cervix is secured with two 0 Vicryl sutures placed at the 3 and 9 o’clock positions at the vaginal cervical reflections. An injection of 10 to 20 mL of normal saline is made just beneath the cervical mucosa to create a plane of dissection. B. A transverse 2-cm incision is made on the anterior aspect of the cervix at the 12 o’clock position and is carried down to the pubocervical fascia. The bladder is pushed cranially and is freed from the cervix (i.e., the bladder is advanced). C. A similar incision is made on the posterior surface of the cervix. In this case, the cul-de-sac is dissected away from the cervical tissue and is advanced. D. A Mersilene band swagged onto a large, curved needle enters via the anterior incision and exits via the posterior incision on the right and left. The cervix is now completely encircled by the band. E. The needles are cut off, and the band is tied at 6 o’clock over a rubber catheter. F. Anteriorly and posteriorly, 3-0 nylon sutures are placed through the band and into the substance of the cervix to anchor the band and prevent migration. Finally, the incisions are closed with a 2-0 Vicryl running or interrupted suture.
FIGURE 49–4 A. McDonald cerclage. The anterior lip of the cervix is held with a tenaculum. A #2 Prolene suture is placed into the cervix beginning on the anterior surface below the junction of the cervical and vaginal mucosa. B. The suture is vectored counterclockwise around the cervix, while taking multiple, secure bites into the cervical mucosa and stroma throughout the circumnavigation of the cervix. C. The suture is squarely tied down over the finger of the assistant. This prevents excessive cinching down of the stitch and will reduce the chances of the suture cutting completely through the cervix. Inset. The final puckered appearance of the sutured cervix (purse string or tobacco pouch effect).