Central Retinal Vein Occlusion
Clinical Features:
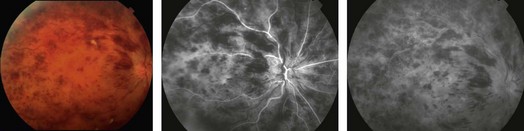
Dilated, tortuous retinal veins and intraretinal hemorrhages are noted in all four quadrants (Fig. 14.2.1). Cotton wool spots, disc edema and macular edema may also be seen. CRVO may be subdivided into ischemic or non-ischemic based on the degree of peripheral retinal non-perfusion seen on fluorescein angiography. Ischemic CRVO tend to have worse visual acuity (<20/200) and more confluent hemorrhage and cotton wool spots. Non-ischemic CRVO usually presents with better visual acuity and the relative paucity of cotton wool spots. Non-ischemic CRVO will convert to ischemic CRVO over weeks to months in about 20–30% of cases. Although the diagnosis of CRVO can be made by the characteristic fundus appearance, perfusion and the presence of ischemia is best assessed by a fluorescein angiogram.
OCT Features:
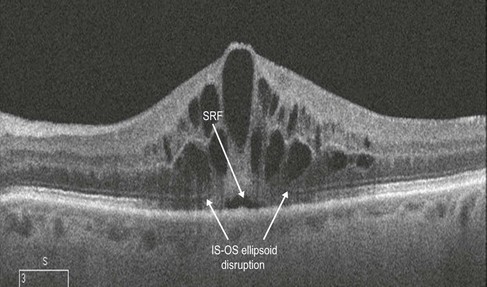
Macular edema, a critical feature of CRVO, is best evaluated by an OCT scan (Figs 14.2.2 and 14.2.3). A line scan through the macula shows diffuse thickening with hyporeflective spaces within the outer retinal layers consistent with cystoid macular edema. Some subretinal fluid may also be noted, which most likely is secondary to excess intraretinal fluid ‘overflowing’ into the subretinal space.
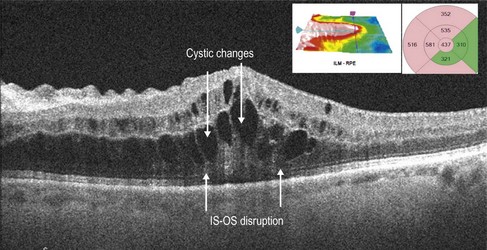
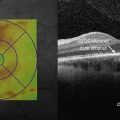
Figure 14.2.2 Intraretinal thickening is noted. Cystic changes are seen in the outer retina that span multiple retinal layers. There is some subretinal fluid. The thickening does not respect the horizontal raphe as seen on the thickness map (inset). There is ellipsoid IS-OS disruption seen.