Central Line Anatomy
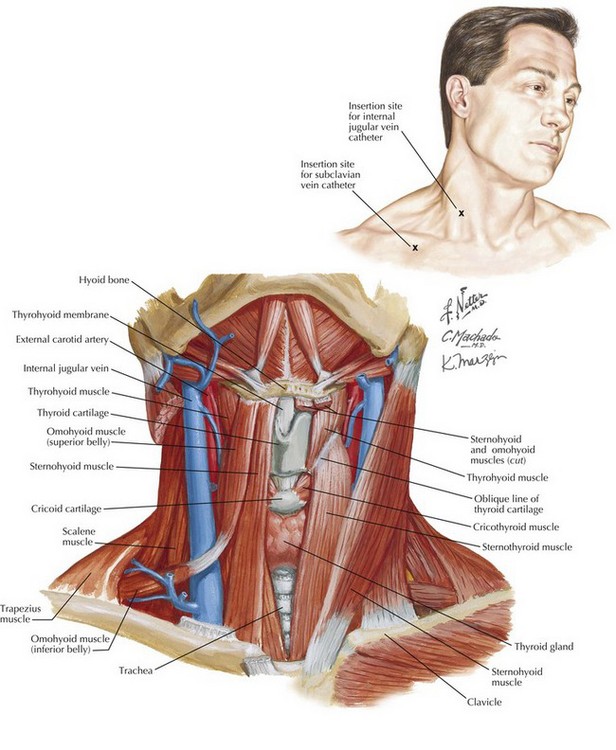
Internal Jugular Vein Catheterization
The internal jugular vein is located in the triangle formed by the two heads of the sternocleidomastoid muscle and clavicle in the anterior neck (Fig. 40-1). Cannulation of the right internal jugular vein is preferred to the left vein because the right provides more direct access to the right atrium, avoids the thoracic duct, and is associated with fewer complications. The ultrasound probe is placed to position the vein in the center of the image. The surgeon differentiates the internal jugular vein from the carotid artery by noting that the vein compresses with gentle pressure.
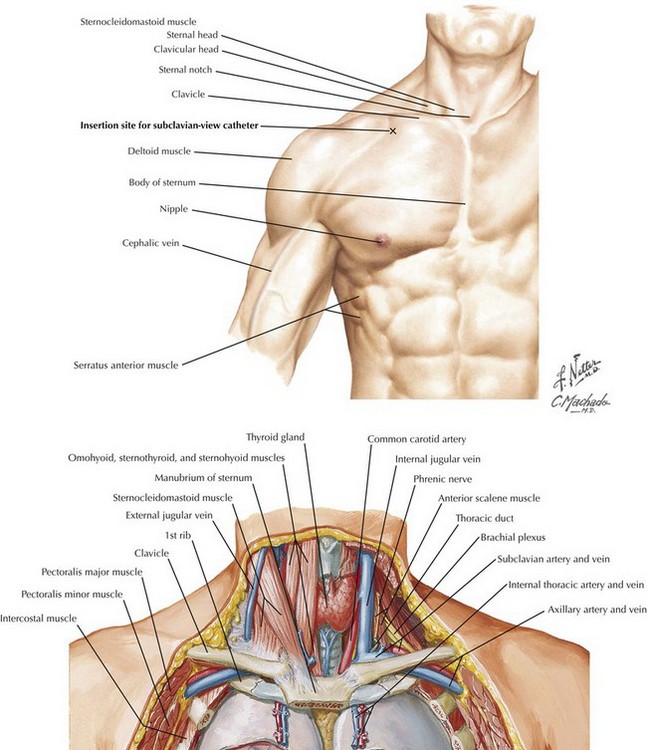
Subclavian Vein Catheterization
The subclavian vein passes just below the point where the clavicle deviates from the 1st and 2nd ribs (Fig. 40-2). Here the vein is anterior and inferior to the subclavian artery. The needle is inserted at a point 2 cm lateral and 2 cm inferior to the junction of the middle and lateral thirds of the clavicle. The needle penetrates the skin at a 15- to 30-degree angle and can be directed toward a point 1 to 2 cm above the sternal notch.
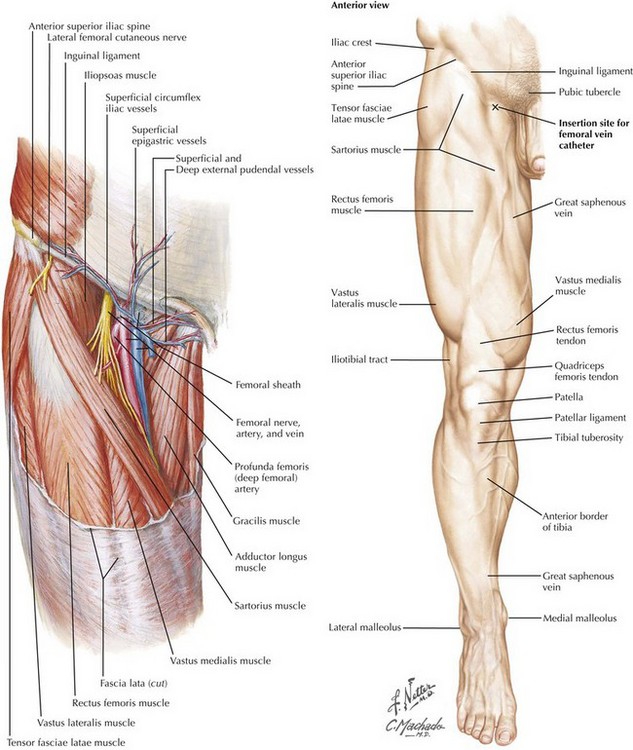
Femoral Vein Catheterization
The femoral vein lies within the femoral triangle in the inguinal-femoral area (Fig. 40-3). The triangle is formed by the inguinal ligament, adductor longus muscle, and sartorius muscle. When the inguinal ligament is not easily seen, its position can be determined as it courses between the pubic tubercle and anterior superior iliac spine. The femoral artery lies at the midpoint along the course of the inguinal ligament, and the femoral vein lies medial to the artery below the inguinal ligament.
Braner, D, Lai, S, Eman, S, Tegtmeyer, K. Central venous catheterization: subclavian vein. N Engl J Med. 2007;357:e26.
Kron, IL, Ailawadi, G. Cardiovascular monitoring and support. In: Fischer JE, ed. Fischer’s mastery of surgery. 6th ed. Philadelphia: Wolters Kluwer/Lippincott, Williams & Wilkins; 2012:65–82.
Ortega, R, Song, M, Hansen, CJ, Barash, P. Ultrasound-guided internal jugular vein cannulation. N Engl J Med. 2010;362:e57.