Chapter 11 Causes of Nontraumatic Hemorrhagic Stroke in Children
Pediatric Moyamoya Syndrome
• Ischemic stroke is relatively rare in children (approximately 2 to 3 per 100,000 children) compared to the adult population. In adults, 80% to 85% of strokes are ischemic, whereas the remaining 15% to 20% are hemorrhagic. In children, 55% of strokes are believed to be ischemic, and the remainder hemorrhagic.
• Early diagnosis of this condition is of paramount importance to minimize sequelae of potential strokes. The etiology of stroke in children covers a wide spectrum to include congenital heart disease, anemia, genetic causes, and moyamoya syndrome.
• The clinical status of the patient at the time of treatment is the most important predictor of long-term outcome. As such, any child with a stroke should have moyamoya syndrome considered in the differential diagnosis to minimize the risk of missing the presence of the disease. There is no medical treatment for moyamoya syndrome that can stop the progressive nature of this condition. Furthermore, the natural history of this condition is that of progressive narrowing of the cerebral vessels; therefore, referral of children with diagnosed moyamoya syndrome to a center experienced with the care of these complex patients is critical to providing optimal care.
• Optimal treatment of moyamoya syndrome appears to be operative, although class I data such as a randomized controlled trial between medical and surgical treatment does not exist. The surgical management of this condition is often successful in experienced centers and consists of cerebral revascularization through a variety of indirect means, such as pial synangiosis in which an extracranial vessel is laid on the cerebral cortex for vascular ingrowth or direct means in which an extracranial vessel is anastomosed to an intracranial vessel. Although direct methods afford immediate revascularization, it is not often technically possible in young children and indirect methods also offer success with revascularization in months.
Ischemic stroke in children is a relatively rare entity relative to the adult population. The World Health Organization’s MONICA Project defines stroke as “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, with symptoms lasting 24 hours or longer or leading to death with no apparent cause other than of vascular origin.”1 The definition includes ischemic and hemorrhagic infarction and intracerebral and subarachnoid hemorrhage. In adults, 80% to 85% of strokes are ischemic, whereas the remaining 15% to 20% are hemorrhagic. In children, 55% are believed to be ischemic, and the remainder hemorrhagic.2,3
Pediatric Ischemic Stroke
In this chapter, the major causes of ischemic stroke in children are reviewed with an emphasis on diseases with neurosurgical relevance, particularly moyamoya syndrome. Reference will be made to the recent American Heart Association (AHA) Scientific Statement on the Management of Stroke in Infants and Children as a resource for current management guidelines.4 Causes of hemorrhagic stroke, including aneurysms and arteriovenous malformations (AVMs) are presented in other chapters in this text.
Incidence
It is difficult to ascertain the general incidence of ischemic stroke in children as there is limited information regarding pediatric stroke epidemiology. A population study from Rochester, Minnesota, of children under 15 years of age detected an incidence of cerebrovascular disease (including both ischemic and hemorrhagic stroke) of 2.5 per 100,000 population. In general, retrospective studies have reported stroke incidence of approximately 2.5 to 3.1 cases per 100,000 children per year.5,6 In Japan, a series looking at ischemic cerebrovascular disease in children under 16 years of age (excluding moyamoya syndrome) identified a rate of 0.2 cases per 100,000 children. This reported rate may be low not only because of the exclusion of strokes caused by moyamoya disease (a leading cause of stroke in Japan) but also because of low rates of congenital heart disease.6 The higher rate of approximately 13 cases of stroke per 100,000 children per year, in a prospective European study, probably reflects the increased availability of better imaging modalities, such as computed tomography (CT).7 Hemorrhagic strokes account for approximately half of all strokes in the pediatric population. In a hospital autopsy series, 8.7% of patients died of complications related to cerebrovascular disease, but the most common cause of death was hemorrhage from an AVM, not ischemic stroke. The rate of recurrence is estimated to be 20% in these children.8
Causes
Strokes in adults are often caused by atherosclerosis; in contrast, the etiology of stroke in children can be diverse and determining the cause can be challenging. Although many different causes and potential risk factors for childhood stroke have been described, ischemic stroke in children frequently results from cardiac embolism, prothrombotic states, or vasculopathies, including the syndrome of moyamoya.4
Genetic Disorders
Several heritable conditions have been implicated in pediatric ischemic stroke. These genetic conditions may be known from family history or may be newly diagnosed in a given patient.9 Congenital metabolic derangements can contribute to premature arteriosclerosis and resultant ischemic stroke.
Dyslipoproteinemias, inborn errors in the metabolism of lipids and cholesterol, have been associated with increased stroke in children. Deficiencies of proteins C and S, antithrombin III deficiency, prothrombin G20210A mutant genotype, sickle cell disease, and activated protein C resistance are examples of inherited hematological abnormalities associated with ischemic stroke.4,10,11 Homocystinuria is a genetic disorder in which endothelial cell injury occurs, with ensuing thrombotic and embolic infarcts. Other inherited metabolic disorders such as the syndrome of mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS), Fabry disease, Menkes disease, and Tangier disease may also be associated with strokes. Although direct correction of the underlying genetic defects of the aforementioned diseases is not yet available, treatment currently focuses on normalizing the metabolic abnormalities. Early knowledge of the predisposing condition can result in heightened vigilance in monitoring for neurological sequelae, and in some cases, stroke burden can be minimized through preventive measures.
Embolic Stroke: Congenital Heart Disease
Strokes may occur in children with either congenital or acquired heart disease. Congenital heart disease is reported to occur in approximately 5 to 10 per 1000 live births and has been implicated in up to one third of all ischemic strokes via embolic phenomena.12,13 Emboli can result from a right-to-left shunt, valvular disease (including mitral valve prolapse), endocardial disease, thrombus/tumor in the left side of the heart, pulmonary arteriovenous fistula, or after cardiac surgery when bypass has been employed. Children with emboli from bacterial endocarditis are also at risk for mycotic aneurysms. The risk for stroke in patients with endocarditis is higher if the disease involves the left side of the heart.
Special note is made of the Fontan operation: essentially an anastomosis of the right atrium to the pulmonary artery. It is one of the most common cardiac operations for children over 1 year of age with congenital heart disease and the surgery is associated with a 2.6% risk of stroke. The risk period for stroke extends from the first postoperative day to 32 months following the Fontan procedure.14
Thrombotic Stroke: Sickle Cell Disease and Hypercoagulable Conditions
Thrombotic stroke is a phenomenon described in children, often in association with polycythemia, dehydration, and infection. One of the most common entities associated with thrombotic stroke in children is sickle cell disease.4
Sickle cell disease affects nearly 1 in 400 African Americans, with a nearly 10% lifetime risk of stroke.15 Many strokes occur in children, with most strokes occurring before 10 years of age.16 Cerebral infarction is often caused by progressive occlusion of the distal internal carotid artery, usually involving the anterior cerebral and middle cerebral artery distributions. Treatment includes hydration, transfusion, and in some cases bone marrow transplant to correct the underlying genetic disorder. Of particular note, recent literature—from our group and others—has highlighted the finding that a substantial number of children with sickle cell disease will fail medical therapy and develop moyamoya syndrome.17,18 Importantly, there is evidence supporting the premise that this subset of children respond well to surgical treatment of their moyamoya disease and should thus be considered for referral to a neurosurgical center experienced in the management of this condition.4,17,18
Other conditions are also associated with prothrombotic disorders. In children who present with ischemic strokes, between 10% and 50% have been reported to have some type of prothrombotic state.19–21 These prothrombotic processes can be genetic, such as factor V Leiden mutation, antiphospholipid antibodies, hyperhomocysteinemia, and elevated lipoprotein(a), or acquired, such as deficiencies in clotting pathways resulting from infection, medications, hepatic disease, or renal disease. Protein C, protein S, and antithrombin III deficiency may be either inherited or acquired. In all children who present with ischemic stroke, laboratory investigation of these hypercoagulable states should be undertaken.
Extracranial Arterial Dissection
Dissection of the carotid or vertebral arteries can occur in children spontaneously or may be secondary to trauma. Stroke can result from emboli from the site of dissection or from reduced blood flow from the narrowed vessel caliber. Of all patients (adult and pediatric) with dissections of these vessels, 6.8% were under the age of 18.22 Presenting symptoms are usually pain (either headache or neck pain) and neurological signs referable to the site of injury. With carotid dissections, Horner syndrome may be present due to injury of the sympathetic plexus surrounding the artery, in addition to neurological deficits referable to the regions of the brain supplied by the carotid. In the posterior circulation, Horner syndrome can also be caused as a result of lateral medullary infarction.
The history may be notable for no injury or seemingly insignificant trauma and there may be an interval of several days between the presumed causative event and the presenting symptoms. Although the gold standard remains conventional six-vessel angiography, the diagnosis of craniocervical dissection is increasingly being made with noninvasive imaging modalities, such as computed tomographic angiography (CTA) and magnetic resonance angiography (MRA).23 Because of technique constraints, MRA and CTA may miss some dissections, particularly those involving the posterior circulation. Particular attention should be paid to the C1-C2 region, as that is the most common site of vertebral artery dissection.24
Treatment is predicated on minimizing embolic events and allowing the injured vessel wall to heal. The risk for recurrent dissection is 12% and seems to be particularly high in the first several months immediately following presentation.22 Optimal treatment remains controversial. At Children’s Hospital Boston, we favor the use of anticoagulation, using heparin initially, followed by conversion to warfarin (Coumadin) for 6 months. Follow-up angiography often discloses healing of the dissection, after which anticoagulation is discontinued. If recurrent symptoms or radiographic progression occurs, endovascular therapy is considered.
Cerebral Vasculitis
Cerebral vasculitis is an uncommon cause of stroke in children. The vasculitis may be infectious or noninfectious. Infectious cases include sepsis of any type (particularly meningitis), varicella, human immunodeficiency virus (HIV), and mycoplasma.25–30 Noninfectious causes include a wide variety of autoimmune disorders, including Behçet disease, sarcoidosis, Sjögren syndrome, ulcerative colitis, Kawasaki disease, and Schönlein-Henoch purpura (SHP), among others.4,31,32
Previous work has demonstrated that only 4% of strokes in children were attributable to vasculitis.33 Further study did not find any cause of vasculitis in children younger than 14 years of age with cerebrovascular disease.5 Taken together, these findings suggest that the incidence of vasculitis, even in at-risk populations, is very low. These data are important, as the neurosurgeon will often be consulted for consideration of brain biopsy in an attempt to make the diagnosis of cerebral vasculitis.
Miscellaneous Causes
One increasingly common cause for stroke in children is the use of illicit drugs. Strokes have been reported in association with the use of amphetamines, cocaine, and phencyclidine (PCP) among others. Suggested mechanisms include transient cerebral vasoconstriction, unmasking of a preexisting cardiovascular disease, toxic vasculitis, and prothrombotic tendencies.34
Migraines are usually benign in children; however, there are reports of infarcts, usually in the vertebrobasilar distribution, associated with this disorder. Presumably these permanent deficits are the result of decreased vessel caliber during the migraine, leading to ischemia and infarction.4
Radiation-induced vasculopathy is a cause of stroke in patients involving either large or small vessels. Most commonly seen in patients treated for tumors, it may present in a delayed fashion. A recent study found that approximately 6% of children with central nervous system tumors treated with radiation had radiographic evidence of stroke.35 One of the most important stroke syndromes associated with radiotherapy is moyamoya syndrome (see following section).36,37
Moyamoya Syndrome
Moyamoya syndrome, a vasculopathy characterized by chronic progressive stenosis at the apices of the intracranial internal carotid arteries, is an increasingly recognized entity associated with cerebral ischemia.38 This progressive stenosis occurs simultaneously as characteristic arterial collateral vessels develop at the base of the brain. These collateral vessels, when visualized on angiography, have been likened to the appearance of haze, a cloud, or a puff of smoke, which translates to “moyamoya” in Japanese.
This arteriopathy results in diminished blood supply to the brain, with resultant transient ischemic attacks (TIAs), seizures, headaches, hemorrhage, and strokes (Table 11.1). It has been associated with approximately 6% of childhood strokes.39,40 There are few to no class I or II data on the treatment of pediatric moyamoya syndrome, and the evidence that serves as a basis for guidelines is aggregated class III data.4 A recent meta-analysis of the literature of surgical treatment of pediatric moyamoya syndrome and a review article in the New England Journal of Medicine offer two sources for more comprehensive summaries of the literature.38,41
TABLE 11.1 Frequency of Presenting Signs and Symptoms in Patients with Moyamoya Syndrome
| Sign/Symptom | No. of Patients Affected (N = 143)∗ |
|---|---|
| Stroke | 97 (67.8%) |
| TIAs (including drop attacks) | 62 (43.4%) |
| Seizures | 9 (6.3%) |
| Headache | 9 (6.3%) |
| Choreiform movements | 6 (4.2%) |
| Incidental finding | 6 (4.2%) |
| Intraventricular or intracerebral bleed | 4 (2.8%) |
TIAs, transient ischemic attacks.
∗ Symptom totals are greater than patient total because some patients had multiple symptoms at presentation.
Epidemiology
First described in Japan, moyamoya syndrome has now been observed throughout the world and affects individuals of many ethnic backgrounds, with increasing detection of this disease in American and European populations.42,43 In Japan, it is the most common pediatric cerebrovascular disease; affecting females almost twice as much as males with a prevalence of approximately 3 per 100,000.39,44 In Europe, a recent study cited an incidence of 0.3 patients per center per year, which is approximately one tenth of the incidence in Japan.45 A 2005 U.S. study suggests an incidence that was 0.086 per 100,000 persons. The ethnicity-specific incidence rate ratios compared to whites were 4.6 (95% confidence interval [CI]: 3.4 to 6.3) for Asian Americans, 2.2 (95% CI: 1.3 to 2.4) for African Americans, and 0.5 (95% CI: 0.3 to 0.8) for Hispanics.46
In the United States and Korea, reports corroborated historical claims of a bimodal age distribution of moyamoya syndrome, one group in the pediatric age range (around the first decade of life) and a second group of adults in the 30- to 40-year-old range. Adults—who still predominantly present with stroke—have a sevenfold increased likelihood of presenting with hemorrhage as compared to children.38,47,48 In contrast, children usually present with TIAs or strokes, which may prove more difficult to diagnose because of the patient’s age, leading to delayed recognition of the underlying moyamoya.38,49
Associated Conditions
A number of clinical conditions or predisposing factors have been associated with moyamoya syndrome.18,50–52 Table 11.2 summarizes the clinical associations noted in a recently published series.51
TABLE 11.2 Comorbid Conditions, Risk Factors, and Syndromes Associated with Moyamoya Syndrome
| Condition/Risk Factor/Syndrome | No. of Patients Affected |
|---|---|
| No associated conditions (idiopathic) | 66 |
| Neurofibromatosis type I (NF 1) | 16 |
| Asian ethnicity | 16 |
| Cranial therapeutic irradiation for neoplasia | 15 |
| Hypothalamic-optic system glioma: 8 | |
| Craniopharyngioma: 4 | |
| Medulloblastoma, with Gorlin syndrome: 1 | |
| Acute lymphocytic leukemia, intrathecal chemotherapy: 2 | |
| Down syndrome | 10 |
| Congenital cardiac anomaly, previously operated | 7 |
| Renal artery stenosis | 4 |
| Hemoglobinopathy: 2 sickle cell, 1 Bryn Mawr (four African-American patients, two of whom were the individuals with sickel cell disears [see above]) | 3 |
| Other hematological syndromes: 1 spherocytosis, 1 ITP | 2 |
| Giant cervicofacial hemangiomas | 3 |
| Shunted hydrocephalus | 3 |
| Idiopathic hypertension requiring medication | 3 |
| Hyperthyroidism (1 with Graves’ disease) | 2 |
| Other conditions/syndromes | 10 |
| Reye (remote), Williams, Alagille syndromes; cloacal exstrophy; renal artery fibromuscular dysplasia; congenital cytomegalic inclusion virus infection (remote): 1 each | |
| Unclassified syndromic presentations: 2 | |
| Among 4 African-American patients: 2 with sickle cell disease |
ITP, idiopathic thrombocytopenic purpura.
Natural History and Prognosis
The prognosis of moyamoya syndrome is difficult to predict because the natural history of this disorder is not well known. The clinical progression of disease can be slow with rare, intermittent events or can be fulminant with rapid neurological decline.50,51 However, regardless of the course, it seems clear that moyamoya syndrome, both in terms of arteriopathy and clinical symptoms, inevitably progresses in untreated patients.53 It has been estimated that 50% to 66% of patients with moyamoya syndrome have progression of the neurological deficits with poor outcomes if left untreated.54,55 This number contrasts strikingly to an estimated rate of only 2.6% of worsened neurological status in a recent meta-analysis of 1156 surgically treated pediatric patients.41 Overall prognosis of patients with moyamoya syndrome depends heavily on the neurological status of the child at time of treatment, adding an imperative to early diagnosis and referral to an experienced center.51,56
Screening
There are no data to support indiscriminate screening for moyamoya syndrome and there is little evidence to justify screening first-degree relatives of patients with moyamoya syndrome when only a single family member is affected. However, a 2008 paper concerning patients with unilateral moyamoya syndrome documents decreased stroke burden and better clinical outcome when this specific population was imaged at intervals, providing evidence in support of selective screening.57 Although widespread screening for moyamoya syndrome is not yet standard for any specific group, the diagnosis should be considered when patients with certain high-risk disorders such as neurofibromatosis type 1, Down syndrome, and sickle cell disease are undergoing routine examinations in order to uncover symptomatic patients and refer them for imaging.58–61
Diagnostic Investigations
Computed Tomography
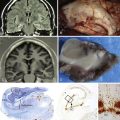
The CT scan in a patient with moyamoya disease may demonstrate small areas of hypodensity suggestive of stroke in cortical watershed zones, basal ganglia, deep white matter, periventricular regions, or hemorrhage.51 However, the CT scan can be normal, particularly in patients presenting solely with TIAs. The intracranial stenoses seen in moyamoya disease may be demonstrated by CTA. Thus, CTA should be considered when MRI is not readily available and a diagnosis of cerebral occlusive vasculopathy is being considered.
Magnetic Resonance Imaging
Widespread availability of MRI and MRA has led to increasing use of these modalities for primary imaging in patients experiencing symptoms suggestive of moyamoya syndrome.62–64 An acute infarct is best seen using diffusion-weighted imaging (DWI), while a chronic infarct is better demonstrated with T1 and T2 imaging. Diminished cortical blood flow secondary to moyamoya syndrome can be inferred from so-called FLAIR (fluid attenuated inversion recovery) sequences, which demonstrate linear high signals that follow a sulcal pattern, which is called the ivy sign.65 The finding most suggestive of moyamoya syndrome on MRI is reduced flow voids in the internal, middle, and anterior cerebral arteries coupled with prominent flow voids through the basal ganglia and thalamus from moyamoya collateral vessels. These imaging findings are virtually diagnostic of moyamoya syndrome.66
Angiography
Formal angiography should consist of a full six-vessel study that includes both external carotid arteries, both internal carotid arteries, and one or both vertebral arteries, depending on the collateral patterns visualized. In a study of 190 angiograms, complication rates in moyamoya patients were no higher than those in non-moyamoya patients with other forms of cerebrovascular disease.67
Definitive diagnosis is based on a distinct arteriographic appearance characterized by bilateral stenosis of the distal intracranial internal carotid artery extending to the proximal anterior and middle arteries. Disease severity is frequently classified into one of six progressive stages, originally defined by Suzuki.53 Development of an extensive collateral network at the base of the brain along with the classic “puff of smoke” appearance on angiography is seen in the intermediate stages of the Suzuki grading system. External carotid imaging is essential to identify preexisting collateral vessels so that surgery, if performed, will not disrupt them. Aneurysms, and the rare arteriovenous malformation known to be associated with certain cases of moyamoya syndrome, can also be best detected by conventional angiography.
Other Diagnostic Techniques
Other diagnostic evaluations that may be useful in evaluating patients with moyamoya syndrome include electroencephalography (EEG) and cerebral blood flow studies. Specific alterations of EEG recordings are usually observed only in pediatric patients and include posterior or centrotemporal slowing, a hyperventilation-induced diffuse pattern of monophasic slow waves (called build-up), and a characteristic rebuild-up phenomenon,68 which looks identical to the build-up slow waves seen in non-moyamoya patients, but differs in the timing of its presentation. Build-up occurs during hyperventilation while rebuild-up occurs after the hyperventilation is completed and indicates a diminished cerebral perfusion reserve.
Treatment Considerations
The majority of data available supports the use of surgical revascularization as a first-line therapy for the treatment of moyamoya syndrome, particularly for patients with recurrent or progressive symptoms.4,41 Abundant type III data, including two relatively large studies with long-term follow-up, have demonstrated a good safety profile for surgical treatment of moyamoya (4% risk of stroke within 30 days of surgery per hemisphere) with a 96% probability of remaining stroke-free over a 5-year follow-up period.51,54 These type III data suggest that surgical therapy of moyamoya syndrome confers an effective, durable treatment for the disease and these findings are concordant with the recent AHA guidelines.4
Historically, there has been a paucity of data comparing the efficacy of medical versus surgical therapy for moyamoya syndrome. A large survey in 1994 from Japan noted that among 821 registered patients with moyamoya syndrome, there were no significant differences in outcome between medically and surgically treated patients.69 However, a recent study indicated that 38.4% of 651 moyamoya patients who were not initially treated with surgery eventually came to surgery as a result of progressive symptoms.70 Medical therapy is often used as treatment for moyamoya syndrome, particularly when the patient is a poor operative risk (severe cardiac disease, advanced debilitation from stroke burden, or other severe comorbid conditions) or has relatively mild moyamoya disease. Aspirin is a standard maintenance therapy for the syndrome without any published series demonstrating its long-term efficacy. A recent meta-analysis noted that medical therapy should not be employed for the treatment of patients with progressive neurological symptoms, stating that medical treatments (e.g., vasodilators, low-molecular-weight dextrans, and steroids) are ineffective.41
Indications for Surgery
Currently, there are no class I or II data to support specific determinants of indications for medical versus surgical therapy. The quality of evidence compiled in a recent meta-analysis of 1448 patients from 57 studies in the English language led to recommendations that were graded D (on a scale from A to D), meaning that they are based completely on class III data (nonanalytic studies) and expert opinions.41 Indications for surgery were noted in less than 15% of studies and varied between centers.41 General indications and timing of surgery remain controversial.71,72 Guidelines from Japan’s Ministry of Health and Welfare regarding indications for surgical treatment of moyamoya syndrome state: “In the cases with (1) repeated clinical symptoms due to apparent cerebral ischemia, or (2) a decreased regional cerebral blood flow, vascular response and perfusion reserve, based on the findings of a cerebral circulation and metabolism study, surgery is indicated.”69 The 2008 AHA guidelines (Box 11.1) are concordant with those from Japan, stating, “Indications for revascularization surgery include progressive ischemic symptoms or evidence of inadequate blood flow or cerebral perfusion reserve in an individual without a contraindication to surgery.”4
BOX 11.1 AHA Guidelines for the Management of Children with Moyamoya Disease∗
Class I Recommendations
1. Different revascularization techniques are useful to effectively reduce the risk of stroke resulting from moyamoya disease (Class I, Level of Evidence B).
2. Indirect revascularization techniques are generally preferable and should be used in younger children whose small-caliber vessels make direct anastomosis difficult, whereas direct bypass techniques are preferable in older individuals (Class I, Level of Evidence C).
3. Revascularization surgery is useful for moyamoya disease (Class I, Level of Evidence B). Indications for revascularization surgery include progressive ischemic symptoms or evidence of inadequate blood flow or cerebral perfusion reserve in an individual without a contraindication to surgery (Class I, Level of Evidence B).
Class II Recommendations
1. Transcranial Doppler may be useful in the evaluation and follow-up of individuals with moyamoya disease (Class IIb, Level of Evidence C).
2. Techniques to minimize anxiety and pain during hospitalizations may reduce the likelihood of stroke caused by hyperventilation-induced vasoconstriction in individuals with moyamoya disease (Class IIb, Level of Evidence C).
3. Management of systemic hypotension, hypovolemia, hyperthermia, and hypocarbia during the intraoperative and perioperative periods may reduce the risk of perioperative stroke in individuals with moyamoya disease (Class IIb, Level of Evidence C).
4. Aspirin may be considered in individuals with moyamoya disease after revascularization surgery or in asymptomatic individuals for whom surgery is not anticipated (Class IIb, Level of Evidence C).
5. Techniques to measure cerebral perfusion and blood flow reserve may assist in the evaluation and follow-up of individuals with moyamoya disease (Class IIb, Level of Evidence C).
Class III Recommendations
1. Except in selected individuals with frequent transient ischemic attacks or multiple infarctions despite antiplatelet therapy and surgery, anticoagulants are not recommended for most individuals with moyamoya disease because of the risk of hemorrhage and the difficulty of maintaining therapeutic levels in children (Class III, Level of Evidence C).
2. In the absence of a strong family history of moyamoya disease or medical conditions that predispose to moyamoya syndrome, there is insufficient evidence to justify screening studies for moyamoya disease in asymptomatic individuals or in relatives of patients with moyamoya syndrome (Class III, Level of Evidence C).
Medical Treatment
There is no known medical treatment capable of reversing the progression of moyamoya syndrome. However, there is support for the use of two classes of medications to slow the progression of the disease: anticoagulants/antiplatelet agents and vasodilators.
The antiplatelet effect of aspirin is useful in moyamoya syndrome because some ischemic symptoms appear to occur as a consequence of emboli from microthrombus formation at sites of arterial stenoses.50,51,72,73 Children with moyamoya syndrome typically receive lifelong aspirin therapy, with those younger than 6 years of age receiving 81 mg/day and older children receiving a variable dose depending on the presence or absence of symptoms.51 Although anticoagulants such as warfarin are rarely used owing to the difficulty of maintaining therapeutic levels in children and the risk of hemorrhage from inadvertent trauma, low-dose low-molecular-weight heparin (Lovenox) has been used, at 0.5 mg/kg twice a day, particularly for those children who are neurologically unstable and need rapidly reversible anticoagulation prior to procedures such as surgery or angiography when ongoing aspirin therapy might be contraindicated.74
The other medication class that has been useful in the treatment of certain symptoms in moyamoya syndrome is calcium channel blockers.73 These drugs may be particularly useful in ameliorating symptoms of intractable headaches or migraines, commonly seen in moyamoya patients, and may be effective in reducing both the frequency and severity of refractory TIA in certain patients.
Surgical Treatment
There are a number of studies in the literature that support a role for surgical management of moyamoya disease, and surgery is generally recommended for the treatment of patients with recurrent or progressive cerebral ischemic events and associated reduced cerebral perfusion reserve. Many different operative techniques have been described, all with the main goal of preventing further ischemic injury by increasing collateral blood flow to hypoperfused areas of cortex, using the external carotid circulation as a donor supply.50,51
The surgical procedures can generally be divided into direct and indirect revascularization techniques. Direct anastomosis procedures, most commonly superficial temporal artery (STA) to middle cerebral artery (MCA) anastomosis (STA-MCA bypass), may achieve instant improvement in focal cerebral perfusion, but these procedures are often technically difficult to perform because of small size of scalp donor vessels or middle cerebral artery recipient vessels. The small vessels limit the amount of additional collateral blood flow supplied to the brain by the procedure, and the basal moyamoya process itself tends to limit the amount of blood flow redistribution because of the proximal basal occlusive process. A variety of indirect revascularization procedures have been described: encephaloduroarteriosynangiosis (EDAS) whereby the STA is dissected free over a course of several inches and then sutured to the cut edges of the opened dura; encephalomyosynangiosis (EMS) in which the temporalis muscle is dissected and placed onto the surface of the brain to encourage collateral vessel development; and the combination of both, encephalomyoarteriosynangiosis (EMAS).75–77 There are multiple variations of these procedures, including solely drilling burr holes, without vessel synangiosis,78,79 and craniotomy with inversion of the dura in hopes of enhancing new dural revascularization of the brain.80 Cervical sympathectomy and omental transposition or omental pedicle grafting have also been described, although sympathectomy has largely been abandoned due to its ineffectiveness.75,81–90 Finally, a number of groups have reported improved results in the use of combined direct and indirect anastomoses.70,75,83,91 A modification of the EDAS procedure, termed pial synangiosis, employs a donor superficial temporal artery as the source of new collateral, a wide opening of the dura and arachnoid, and an attachment of the donor vessel directly to the brain surface by fine sutures.51 The long-term efficacy of this variant of indirect revascularization has been validated by the largest surgical series of pediatric moyamoya patients reported in North America.51
One major consideration is the decision of which surgical technique to employ. In the United States, the AHA guidelines state that indirect procedures, such as pial synangiosis, are best suited to younger patients4 (see Box 11.1).
Once the decision for surgical therapy has been made, several perioperative considerations need to be addressed. In addition to the general issues regarding surgery in children, moyamoya patients are at particular risk of ischemic events in the perioperative period. Crying and hyperventilation, common occurrences in children at times during hospitalization, can lower PCO2 and induce ischemia secondary to cerebral vasoconstriction. Any techniques to reduce pain—including the use of perioperative sedation, painless wound dressing techniques, and absorbable wound suture closures—appear to reduce the incidence of strokes, TIAs, and length of hospital stay.92 A further perioperative consideration is the use of specialized monitoring during surgery, such as EEG, which might identify and help prevent cerebral ischemia detected while the patient is under general anesthesia.
Perioperative and Intraoperative Considerations
The administration of general anesthesia can result in transient physiological changes that can affect cerebral blood flow. Blood pressure, blood volume, and PaCO2 require careful monitoring because moyamoya patients have a diminished cerebral perfusion reserve and deviation from normal levels can result in stroke.92 To reduce the risk of intraoperative and perioperative neurological morbidity, therefore, meticulous management of the patient is required to avoid hypotension, hypovolemia, hyperthermia, and hypocarbia both intraoperatively and perioperatively.51 As noted previously, intraoperative EEG monitoring with a full array of scalp electrodes can be helpful in the neurological assessment of patients under general anesthesia. To help prevent hypovolemia during surgery, patients are often admitted the evening prior to surgery for aggressive intravenous hydration. Postoperatively, the patients are hydrated with intravenous fluids at 1.5 times the normal maintenance rate based on weight for 48 to 72 hours. Aspirin is given on the first postoperative day.
Follow-up Considerations
Careful follow-up of patients with moyamoya syndrome is warranted.41,69 Of patients treated conservatively or with medical management, 38.3% of unoperated patients required surgery eventually.70 A study of patients initially diagnosed with unilateral moyamoya found that 27% (17 of 64) of those with unilateral disease progressed to bilateral involvement, with younger patients being most commonly affected, often within 1 to 5 years.93 Other data further support the premise that younger children with unilateral disease commonly progress to bilateral involvement.94 Of those patients who were treated operatively (for either bilateral or unilateral disease), the need for reoperation due to refractory disease ranged from 1.8% to 18%.69 These data suggest that periodic clinical and radiographic examinations of patients with moyamoya disease, even if treated, should be performed on a regular basis.
Postoperative angiograms or MRI/MRA studies are usually obtained 12 months after surgery and typically demonstrate MCA collateralization from both the donor STA and the meningeal arteries.51,70 A review of 143 children with moyamoya syndrome treated with pial synangiosis demonstrated marked reductions in their stroke frequency after surgery, especially after 1 month postoperatively: 67% had strokes preoperatively, 7.7% had strokes in the perioperative period, and only 3.2% had strokes after at least 1 year of follow-up. The long-term results are excellent, with a stroke rate of 4.3% (2 patients in a group of 46) in patients with a minimum of 5 years of follow-up.51 This work supports the premise that surgical treatment of moyamoya syndrome provides a significant protective effect against new strokes in this patient population and is further supported by a recent meta-analysis of children treated surgically for moyamoya syndrome, which found that out of 1156 patients, 1003 (87%) derived symptomatic benefit from surgical revascularization (complete disappearance or reduction in symptomatic cerebral ischemia).41
Fung L.W., Thompson D., Ganesan V. Revascularisation surgery for paediatric moyamoya: a review of the literature. Childs Nerv Syst. 2005;21:358-364.
Roach E.S., Golomb M.R., Adams R., et al. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke. 2008;39:2644-2691.
Scott R.M., Smith E.R. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360:1226-1237.
Scott R.M., Smith J.L., Robertson R.L., et al. Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg Spine. 2004;100:142-149.
Suzuki J., Takaku A. Cerebrovascular “moyamoya” disease: disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20:288-299.
Please go to expertconsult.com to view a complete list of references.
1. Thorvaldsen P., Asplund K., Kuulasmaa K., et al. Stroke incidence, case fatality, and mortality in the WHO MONICA project. World Health Organization Monitoring Trends and Determinants in Cardiovascular Disease. Stroke. 1995;26:361-367.
2. Daniels S.R., Bates S., Lukin R.R., et al. Cerebrovascular arteriopathy (arteriosclerosis) and ischemic childhood stroke. Stroke. 1982;13:360-365.
3. Nencini P., Inzitari D., Baruffi M.C., et al. Incidence of stroke in young adults in Florence, Italy. Stroke. 1988;19:977-981.
4. Roach E.S., Golomb M.R., Adams R., et al. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke. 2008;39:2644-2691.
5. Schoenberg B.S., Mellinger J.F., Schoenberg D.G. Cerebrovascular disease in infants and children: a study of incidence, clinical features, and survival. Neurology. 1978;28:763-768.
6. Satoh S., Shirane R., Yoshimoto T. Clinical survey of ischemic cerebrovascular disease in children in a district of Japan. Stroke. 1991;22:586-589.
7. Giroud M., Lemesle M., Gouyon J.B., et al. Cerebrovascular disease in children under 16 years of age in the city of Dijon, France: a study of incidence and clinical features from 1985 to 1993. J Clin Epidemiol. 1995;48:1343-1348.
8. Isler W. Stroke in childhood and adolescence. Eur Neurol. 1984;23:421-424.
9. Pullicino P., Greenberg S., Trevisan M. Genetic stroke risk factors. Curr Opin Neurol. 1997;10:58-63.
10. Chaturvedi S., Dzieczkowski J. Multiple hemostatic abnormalities in young adults with activated protein C resistance and cerebral ischemia. J Neurol Sci. 1998;159:209-212.
11. De Stefano V., Chiusolo P., Paciaroni K., et al. Prothrombin G20210A mutant genotype is a risk factor for cerebrovascular ischemic disease in young patients. Blood. 1998;91:3562-3565.
12. Riela A.R., Roach E.S. Etiology of stroke in children. J Child Neurol. 1993;8:201-220.
13. Mitchell S.C., Korones S.B., Berendes H.W. Congenital heart disease in 56,109 births. Incidence and natural history. Circulation. 1971;43:323-332.
14. du Plessis A.J., Chang A.C., Wessel D.L., et al. Cerebrovascular accidents following the Fontan operation. Pediatr Neurol. 1995;12:230-236.
15. Balkaran B., Char G., Morris J.S., et al. Stroke in a cohort of patients with homozygous sickle cell disease. J Pediatr. 1992;120:360-366.
16. Ohene-Frempong K. Stroke in sickle cell disease: demographic, clinical, and therapeutic considerations. Semin Hematol. 1991;28:213-219.
17. Hankinson T.C., Bohman L.E., Heyer G., et al. Surgical treatment of moyamoya syndrome in patients with sickle cell anemia: outcome following encephaloduroarteriosynangiosis. J Neurosurg Pediatr. 2008;1:211-216.
18. Smith E.R., McClain C.D., Heeney M., et al. Pial synangiosis in patients with moyamoya syndrome and sickle cell anemia: perioperative management and surgical outcome. Neurosurg Focus. 2009;26:E10.
19. deVeber G., Monagle P., Chan A., et al. Prothrombotic disorders in infants and children with cerebral thromboembolism. Arch Neurol. 1998;55:1539-1543.
20. Nowak-Gottl U., Strater R., Heinecke A., et al. Lipoprotein (a) and genetic polymorphisms of clotting factor V, prothrombin, and methylenetetrahydrofolate reductase are risk factors of spontaneous ischemic stroke in childhood. Blood. 1999;94:3678-3682.
21. Ganesan V., McShane M.A., Liesner R., et al. Inherited prothrombotic states and ischaemic stroke in childhood. J Neurol Neurosurg Psychiatry. 1998;65:508-511.
22. Schievink W.I., Mokri B., Piepgras D.G. Spontaneous dissections of cervicocephalic arteries in childhood and adolescence. Neurology. 1994;44:1607-1612.
23. Ganesan V., Savvy L., Chong W.K., et al. Conventional cerebral angiography in children with ischemic stroke. Pediatr Neurol. 1999;20:38-42.
24. Garg B.P., Ottinger C.J., Smith R.R., et al. Strokes in children due to vertebral artery trauma. Neurology. 1993;43:2555-2558.
25. Berkefeld J., Enzensberger W., Lanfermann H. MRI in human immunodeficiency virus-associated cerebral vasculitis. Neuroradiology. 2000;42:526-528.
26. Ganesan V., Kirkham F.J. Mechanisms of ischaemic stroke after chickenpox. Arch Dis Child. 1997;76:522-525.
27. Hayman M., Hendson G., Poskitt K.J., et al. Postvaricella angiopathy: report of a case with pathologic correlation. Pediatr Neurol. 2001;24:387-389.
28. Park Y.D., Belman A.L., Kim T.S., et al. Stroke in pediatric acquired immunodeficiency syndrome. Ann Neurol. 1990;28:303-311.
29. Snyder R.D., Stovring J., Cushing A.H., et al. Cerebral infarction in childhood bacterial meningitis. J Neurol Neurosurg Psychiatry. 1981;44:581-585.
30. Fugate S., Roos K.L. Stroke associated with infections including immunizations. Semin Cerebrovasc Dis Stroke. 2001;1:240-248.
31. Sokol D.K., McIntyre J.A., Short R.A., et al. Henoch-Schonlein purpura and stroke: antiphosphatidylethanolamine antibody in CSF and serum. Neurology. 2000;55:1379-1381.
32. Lopez-Yunez A.M., Garg B.P. Non-infectious cerebral vasculitis in children. Sem Cerebrovasc Dis Stroke. 2001;1:249-263.
33. Williams L.S., Garg B.P., Cohen M., et al. Subtypes of ischemic stroke in children and young adults. Neurology. 1997;49:1541-1545.
34. Sloan M.A., Kittner S.J., Feeser B.R., et al. Illicit drug-associated ischemic stroke in the Baltimore-Washington Young Stroke Study. Neurology. 1998;50:1688-1693.
35. Fouladi M., Langston J., Mulhern R., et al. Silent lacunar lesions detected by magnetic resonance imaging of children with brain tumors: a late sequela of therapy. J Clin Oncol. 2000;18:824-831.
36. Serdaroglu A., Simsek F., Gucuyener K., et al. Moyamoya syndrome after radiation therapy for optic pathway glioma: case report. J Child Neurol. 2000;15:765-767.
37. Ullrich N.J., Robertson R., Kinnamon D.D., et al. Moyamoya following cranial irradiation for primary brain tumors in children. Neurology. 2007;68:932-938.
38. Scott R.M., Smith E.R. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360:1226-1237.
39. Nagaraja D., Verma A., Taly A.B., et al. Cerebrovascular disease in children. Acta Neurol Scand. 1994;90:251-255.
40. Soriano S.G., Sethna N.F., Scott R.M. Anesthetic management of children with moyamoya syndrome. Anesth Analg. 1993;77:1066-1070.
41. Fung L.W., Thompson D., Ganesan V. Revascularisation surgery for paediatric moyamoya: a review of the literature. Childs Nerv Syst. 2005;21:358-364.
42. Suzuki J., Kodama N. Moyamoya disease—a review. Stroke. 1983;14:104-109.
43. Caldarelli M., Di Rocco C., Gaglini P. Surgical treatment of moyamoya disease in pediatric age. J Neurosurg Sci. 2001;45:83-91.
44. Wakai K., Tamakoshi A., Ikezaki K., et al. Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey. Clin Neurol Neurosurg. 1997;99(Suppl 2):S1-S5.
45. Yonekawa Y., Ogata N., Kaku Y., et al. Moyamoya disease in Europe, past and present status. Clin Neurol Neurosurg. 1997;99(Suppl 2):S58-S60.
46. Uchino K., Johnston S.C., Becker K.J., et al. Moyamoya disease in Washington State and California. Neurology. 2005;65:956-958.
47. Han D.H., Kwon O.K., Byun B.J., et al. A co-operative study: clinical characteristics of 334 Korean patients with moyamoya disease treated at neurosurgical institutes (1976-1994). The Korean Society for Cerebrovascular Disease. Acta Neurochir (Wien). 2000;142:1263-1273. discussion 1273–1274
48. Yilmaz E.Y., Pritz M.B., Bruno A., et al. Moyamoya: Indiana University Medical Center experience. Arch Neurol. 2001;58:1274-1278.
49. Nishimoto A., Ueta K., Onbe H. Cooperative study on moyamoya disease in Japan, in Abstracts of the 10th Meeting on Surgery for. Stroke. Tokyo: Nyuuron-sha. 1981:53-58.
50. Ohaegbulam C.M.S., Scott R.M. Moyamoya syndrome. In: McLone D., editor. Pediatric Neurosurgery. Philadelphia: WB Saunders; 2001:1077-1092.
51. Scott R.M., Smith J.L., Robertson R.L., et al. Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg Spine. 2004;100:142-149.
52. Qaiser R., Scott R.M., Smith E.R. Identification of an association between Robinow syndrome and moyamoya. Pediatr Neurosurg. 2009;45:69-72.
53. Suzuki J., Takaku A. Cerebrovascular “moyamoya” disease: Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20:288-299.
54. Choi J.U., Kim D.S., Kim E.Y., et al. Natural history of moyamoya disease: comparison of activity of daily living in surgery and non surgery groups. Clin Neurol Neurosurg. 1997;99(Suppl 2):S11-S18.
55. Kurokawa T., Chen Y.J., Tomita S., et al. Cerebrovascular occlusive disease with and without the moyamoya vascular network in children. Neuropediatrics. 1985;16:29-32.
56. Fukuyama Y., Umezu R. Clinical and cerebral angiographic evolutions of idiopathic progressive occlusive disease of the circle of Willis (“moyamoya” disease) in children. Brain Dev. 1985;7:21-37.
57. Smith E.R., Scott R.M. Progression of disease in unilateral moyamoya syndrome. Neurosurg Focus. 2008;24:E17.
58. Kirkham F.J., DeBaun M.R. Stroke in children with sickle cell disease. Curr Treat Options Neurol. 2004;6:357-375.
59. Roach E.S. Etiology of stroke in children. Semin Pediatr Neurol. 2000;7:244-260.
60. Rosser T.L., Vezina G., Packer R.J. Cerebrovascular abnormalities in a population of children with neurofibromatosis type 1. Neurology. 2005;64:553-555.
61. Jea A., Smith E.R., Robertson R., et al. Moyamoya syndrome associated with Down syndrome: outcome after surgical revascularization. Pediatrics. 2005;116:e694-e701.
62. Yamada I., Suzuki S., Matsushima Y. Moyamoya disease: comparison of assessment with MR angiography and MR imaging versus conventional angiography. Radiology. 1995;196:211-218.
63. Katz D.A., Marks M.P., Napel S.A., et al. Circle of Willis: evaluation with spiral CT angiography, MR angiography, and conventional angiography. Radiology. 1995;195:445-449.
64. Takanashi J.I., Sugita K., Niimi H. Evaluation of magnetic resonance angiography with selective maximum intensity projection in patients with childhood moyamoya disease. Eur J Paediatr Neurol. 1998;2:83-89.
65. Fujiwara H., Momoshima S., Kuribayashi S. Leptomeningeal high signal intensity (ivy sign) on fluid-attenuated inversion-recovery (FLAIR) MR images in moyamoya disease. Eur J Radiol. 2005;55:224-230.
66. Yamada I., Matsushima Y., Suzuki S. Moyamoya disease: diagnosis with three-dimensional time-of-flight MR angiography. Radiology. 1992;184:773-778.
67. Robertson R.L., Chavali R.V., Robson C.D., et al. Neurologic complications of cerebral angiography in childhood moyamoya syndrome. Pediatr Radiol. 1998;28:824-829.
68. Kodama N., Aoki Y., Hiraga H., et al. Electroencephalographic findings in children with moyamoya disease. Arch Neurol. 1979;36:16-19.
69. Fukui M. Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis (“moyamoya” disease). Research Committee on Spontaneous Occlusion of the Circle of Willis (Moyamoya Disease) of the Ministry of Health and Welfare, Japan. Clin Neurol Neurosurg. 1997;99(Suppl 2):S238-S240.
70. Ikezaki K. Rational approach to treatment of moyamoya disease in childhood. J Child Neurol. 2000;15:35035-35036.
71. Roach E.S. Immediate surgery for moyamoya syndrome? Not necessarily. Arch Neurol. 2001;58:130-131.
72. Scott R.M. Surgery for moyamoya syndrome? Yes. Arch Neurol. 2001;58:128-129.
73. Scott R.M. Moyamoya syndrome: a surgically treatable cause of stroke in the pediatric patient. Clin Neurosurg. 2000;47:378-384.
74. Bowen M.D., Burak C.R., Barron T.F. Childhood ischemic stroke in a nonurban population. J Child Neurol. 2005;20:194-197.
75. Matsushima T., Inoue T., Ikezaki K., et al. Multiple combined indirect procedure for the surgical treatment of children with moyamoya disease. A comparison with single indirect anastomosis with direct anastomosis. Neurosurg Focus. 1998;5:e4.
76. Kawaguchi S., Okuno S., Sakaki T. Effect of direct arterial bypass on the prevention of future stroke in patients with the hemorrhagic variety of moyamoya disease. J Neurosurg. 2000;93:397-401.
77. Houkin K., Abe H., Yoshimoto T., Takahashi A. Is “unilateral” moyamoya disease different from moyamoya disease? J Neurosurg. 1996;85:772-776.
78. Sencer S., Poyanli A., Kiris T., et al. Recent experience with moyamoya disease in Turkey. Eur Radiol. 2000;10:569-572.
79. Houkin K., Kuroda S., Nakayama N. Cerebral revascularization for moyamoya disease in children. Neurosurg Clin North Am. 2001;12:575-584. ix,
80. Dauser R.C., Tuite G.F., McCluggage C.W. Dural inversion procedure for moyamoya disease. Technical note. J Neurosurg. 1997;86:719-723.
81. Sato H., Ogawa A., Takahashi A., et al. [Influence of superior cervical ganglion on cerebral hemodynamics—measurements of cerebral blood flow and metabolism during superior cervical ganglionectomy in patients with moyamoya disease.]. No To Shinkei. 1990;42:203-208.
82. Ohtaki M., Uede T., Morimoto S., et al. Intellectual functions and regional cerebral haemodynamics after extensive omental transplantation spread over both frontal lobes in childhood moyamoya disease. Acta Neurochir. 1998;140:1043-1053.
83. Matsushima T., Inoue T., Katsuta T., et al. An indirect revascularization method in the surgical treatment of moyamoya disease—various kinds of indirect procedures and a multiple combined indirect procedure. Neurol Med Chir (Tokyo). 1998;38(Suppl):297-302.
84. Yoshioka N., Tominaga S., Inui T. Cerebral revascularization using omentum and serratus anterior muscle free flap transfer for adult moyamoya disease: case report. Surg Neurol. 1996;46:430-435. discussion 435–436
85. Yoshioka N., Tominaga S., Suzuki Y., et al. Cerebral revascularization using omentum and muscle free flap for ischemic cerebrovascular disease. Surg Neurol. 1998;49:58-65. discussion 66
86. Touho H., Karasawa J., Tenjin H., et al. Omental transplantation using a superficial temporal artery previously used for encephaloduroarteriosynangiosis. Surg Neurol. 1996;45:550-558. discussion 558–559
87. Karasawa J., Kikuchi H., Kawamura J., et al. Intracranial transplantation of the omentum for cerebrovascular moyamoya disease: a two-year follow-up study. Surg Neurol. 1980;14:444-449.
88. Karasawa J., Touho H., Ohnishi H., et al. Cerebral revascularization using omental transplantation for childhood moyamoya disease. J Neurosurg. 1993;79:192-196.
89. Havlik R.J., Fried I., Chyatte D., et al. Encephalo-omental synangiosis in the management of moyamoya disease. Surgery. 1992;111:156-162.
90. Suzuki J., Takaku A., Kodama N., et al. An attempt to treat cerebrovascular “moyamoya” disease in children. Childs Brain. 1975;1:193-206.
91. Matsushima Y. [Indirect anastomoses for moyamoya disease.]. No Shinkei Geka. 1998;26:769-786.
92. Nomura S., Kashiwagi S., Uetsuka S., et al. Perioperative management protocols for children with moyamoya disease. Childs Nerv Syst. 2001;17:270-274.
93. Kawano T., Fukui M., Hashimoto N., et al. Follow-up study of patients with “unilateral” moyamoya disease. Neurol Med Chir (Tokyo). 1994;34:744-747.
94. Hirotsune N., Meguro T., Kawada S., et al. Long-term follow-up study of patients with unilateral moyamoya disease. Clin Neurol Neurosurg. 1997;99(Suppl 2):S178-S181.